Abstract
Purpose
To investigate the effectiveness and cutoffs of axial length/corneal radius (AL/CR) ratio for myopia detection in children by age.
Methods
Totally, 21 kindergartens and schools were enrolled. Non-cycloplegic autorefraction (NCAR), axial length (AL), horizontal and vertical meridian of corneal radius (CR1, CR2), and cycloplegic autorefraction were measured. Receiver operating characteristic (ROC) curve was used to obtain the effectiveness and cutoff for myopia detection.
Results
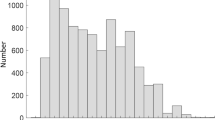
Finally, 7803 participants aged 3–18 years with mean AL/CR ratio of 2.99 ± 0.16 were included. Area under the ROC curve (AUC) of AL/CR ratio for myopia detection (0.958 for AL/CR1, 0.956 for AL/CR2, 0.961 for AL/CR) was significantly larger than that of AL (0.919, all P < 0.001), while AUCs of the three were similar with different cutoffs (> 2.98, > 3.05, and > 3.02). When divided by age, the ROC curves of AL/CR ratio in 3- to 5-year-olds showed no significance or low accuracy (AUCs ≤ 0.823) in both genders. In ≥ 6-year-olds, the accuracies were promising (AUCs ≥ 0.883, all P < 0.001), the cutoffs basically increased with age (from > 2.93 in 6-year-olds to > 3.07 in 18-year-olds among girls, and from > 2.96 in 6-year-olds to > 3.07 in 18-year-olds among boys). In addition, boys presented slightly larger cutoffs than girls in all ages except for 16 and 18 years old. For children aged 3–5 years, AL/CR ratio or AL combined with NCAR increased AUC to > 0.900.
Conclusion
AL/CR ratio provided the best prediction of myopia with age-dependent cutoff values for all but preschool children, and the cutoffs of boys were slightly larger than those of girls. For preschool children, AL/CR ratio or AL combined with NCAR is recommended to achieve satisfactory accuracy. AL/CR ratio calculated by two meridians showed similar predictive power but with different cutoffs.


Similar content being viewed by others
References
Morgan IG, French AN, Ashby RS et al (2018) The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res 62:134–149. https://doi.org/10.1016/j.preteyeres.2017.09.004
Wu PC, Huang HM, Yu HJ, Fang PC, Chen CT (2016) Epidemiology of myopia. Asia Pac J Ophthalmol (Phila) 5(6):386–393. https://doi.org/10.1097/apo.0000000000000236
Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW (2020) The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci 61(4):49. https://doi.org/10.1167/iovs.61.4.49
Ohno-Matsui K, Lai TY, Lai CC, Cheung CM (2016) Updates of pathologic myopia. Prog Retin Eye Res 52:156–187. https://doi.org/10.1016/j.preteyeres.2015.12.001
Morgan IG, Iribarren R, Fotouhi A, Grzybowski A (2015) Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol 93(6):581–585. https://doi.org/10.1111/aos.12642
Hashemi H, Khabazkhoob M, Asharlous A et al (2016) Cycloplegic autorefraction versus subjective refraction: the Tehran eye study. Br J Ophthalmol 100(8):1122–1127. https://doi.org/10.1136/bjophthalmol-2015-307871
Foo VH, Verkicharla PK, Ikram MK et al (2016) Axial length/corneal radius of curvature ratio and myopia in 3-year-old children. Transl Vis Sci Technol 5(1):5. https://doi.org/10.1167/tvst.5.1.5
Wang J, Li Y, Zhao Z et al (2020) School-based epidemiology study of myopia in Tianjin. China Int Ophthalmol 40(9):2213–2222. https://doi.org/10.1007/s10792-020-01400-w
Luo HD, Gazzard G, Liang Y, Shankar A, Tan DT, Saw SM (2006) Defining myopia using refractive error and uncorrected logMAR visual acuity >0.3 from 1334 Singapore school children ages 7–9 years. Br J Ophthalmol 90(3):362–6. https://doi.org/10.1136/bjo.2005.079657
Tong L, Saw SM, Chan ES et al (2004) Screening for myopia and refractive errors using LogMAR visual acuity by optometrists and a simplified visual acuity chart by nurses. Optom Vis Sci 81(9):684–691. https://doi.org/10.1097/01.opx.0000144747.88341.b2
Ma Y, He X, Zou H, Lu L, Qu X, Zhu J (2013) Myopia screening: combining visual acuity and noncycloplegic autorefraction. Optom Vis Sci 90(12):1479–1485. https://doi.org/10.1097/opx.0000000000000095
Lai YH, Tseng HY, Hsu HT, Chang SJ, Wang HZ (2013) Uncorrected visual acuity and noncycloplegic autorefraction predict significant refractive errors in Taiwanese preschool children. Ophthalmology 120(2):271–276. https://doi.org/10.1016/j.ophtha.2012.08.009
He X, Sankaridurg P, Naduvilath T et al (2021) Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4–18 years. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319431
Tong L, Saw SM, Tan D et al (2002) Sensitivity and specificity of visual acuity screening for refractive errors in school children. Optom Vis Sci 79(10):650–657. https://doi.org/10.1097/00006324-200210000-00011
Leone JF, Mitchell P, Morgan IG, Kifley A, Rose KA (2010) Use of visual acuity to screen for significant refractive errors in adolescents: is it reliable? Arch Ophthalmol 128(7):894–899. https://doi.org/10.1001/archophthalmol.2010.134
O’Donoghue L, Rudnicka AR, McClelland JF, Logan NS, Saunders KJ (2012) Visual acuity measures do not reliably detect childhood refractive error–an epidemiological study. PLoS One 7(3):e34441. https://doi.org/10.1371/journal.pone.0034441
Wang J, Xie H, Morgan I et al (2022) How to conduct school myopia screening: comparison among myopia screening tests and determination of associated cutoffs. Asia Pac J Ophthalmol (Phila) 11(1):12–18. https://doi.org/10.1097/apo.0000000000000487
Lin S, Ma Y, He X, Zhu J, Zou H (2019) Using decision curve analysis to evaluate common strategies for myopia screening in school-aged children. Ophthalmic Epidemiol 26(4):286–294. https://doi.org/10.1080/09286586.2019.1616774
Sankaridurg P, He X, Naduvilath T et al (2017) Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol 95(7):e633–e640. https://doi.org/10.1111/aos.13569
He X, Zou H, Lu L et al (2015) Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS One 10(2):e0111766. https://doi.org/10.1371/journal.pone.0111766
Igarashi-Yokoi T, Shinohara K, Fang Y et al (2021) Prognostic factors for axial length elongation and posterior staphyloma in adults with high myopia: a Japanese observational study. Am J Ophthalmol 225:76–85. https://doi.org/10.1016/j.ajo.2020.11.023
Tideman JWL, Polling JR, Vingerling JR et al (2018) Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol 96(3):301–309. https://doi.org/10.1111/aos.13603
Scheiman M, Gwiazda J, Zhang Q et al (2016) Longitudinal changes in corneal curvature and its relationship to axial length in the Correction of Myopia Evaluation Trial (COMET) cohort. J Optom 9(1):13–21. https://doi.org/10.1016/j.optom.2015.10.003
Zhao KK, Yang Y, Wang H et al (2019) Axial length/corneal radius of curvature ratio and refractive development evaluation in 3- to 4-year-old children: the Shanghai Pudong Eye Study. Int J Ophthalmol 12(6):1021–1026. https://doi.org/10.18240/ijo.2019.06.23
Zhang Y, Su M, Liu H et al (2021) Development of refractive parameters in 3- to 6-year-old children and its application in myopia prediction and intervention guidance. Comput Math Methods Med 2021:3656831. https://doi.org/10.1155/2021/3656831
Goss DA, Jackson TW (1995) Clinical findings before the onset of myopia in youth. I. Ocular optical components. Optom Vis Sci 72(12):870–8. https://doi.org/10.1097/00006324-199512000-00005
Wang J, Liu J, Ma W et al (2021) Prevalence of myopia in 3–14-year-old Chinese children: a school-based cross-sectional study in Chengdu. BMC Ophthalmol 21(1):318. https://doi.org/10.1186/s12886-021-02071-6
Ma Y, Lin S, Morgan IG et al (2021) Eyes grow towards mild hyperopia rather than emmetropia in Chinese preschool children. Acta Ophthalmol. https://doi.org/10.1111/aos.14810
Ma Y, Qu X, Zhu X et al (2016) Age-specific prevalence of visual impairment and refractive error in children aged 3–10 years in Shanghai. China Invest Ophthalmol Vis Sci 57(14):6188–6196. https://doi.org/10.1167/iovs.16-20243
Ojaimi E, Rose KA, Morgan IG et al (2005) Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci 46(8):2748–2754. https://doi.org/10.1167/iovs.04-1324
Liu S, He X, Wang J et al (2022) Association between axial length elongation and spherical equivalent progression in Chinese children and adolescents. Ophthalmic Physiol Opt 42(5):1133–1140. https://doi.org/10.1111/opo.13023
Xiong S, Zhang B, Hong Y et al (2017) The associations of lens power with age and axial length in healthy Chinese children and adolescents aged 6 to 18 years. Invest Ophthalmol Vis Sci 58(13):5849–5855. https://doi.org/10.1167/iovs.17-22639
Gordon RA, Donzis PB (1985) Refractive development of the human eye. Arch Ophthalmol 103(6):785–789. https://doi.org/10.1001/archopht.1985.01050060045020
Guo X, Fu M, Ding X, Morgan IG, Zeng Y, He M (2017) Significant axial elongation with minimal change in refraction in 3- to 6-year-old Chinese preschoolers: the Shenzhen kindergarten eye study. Ophthalmology 124(12):1826–1838. https://doi.org/10.1016/j.ophtha.2017.05.030
Iribarren R (2015) Crystalline lens and refractive development. Prog Retin Eye Res 47:86–106. https://doi.org/10.1016/j.preteyeres.2015.02.002
González Blanco F, Sanz Ferńandez JC, Muńoz Sanz MA (2008) Axial length, corneal radius, and age of myopia onset. Optom Vis Sci 85(2):89–96. https://doi.org/10.1097/OPX.0b013e3181622602
Gaurisankar ZS, van Rijn GA, Lima JEE et al (2019) Correlations between ocular biometrics and refractive error: a systematic review and meta-analysis. Acta Ophthalmol 97(8):735–743. https://doi.org/10.1111/aos.14208
Acknowledgements
The authors thank all the children and parents who participated in this study.
Funding
This study was funded by the National Key R&D Program of China (No.2021YFC2702100; No.2021YFC2702101; No.2021YFC2702104; No.2019YFC0840607), National Natural Science Foundation of China (No.82003562; No.81900911), Science and Technology Innovation Action Project of Shanghai Science and Technology Commission (No.21S31900800).
Author information
Authors and Affiliations
Contributions
Conceptualization: Shang Liu, Jun Chen, Jingjing Wang, Jinliuxing Yang, Linlin Du, Xiangui He, Xun Xu; Data curation: Jingjing Wang, Linlin Du; Formal analysis: Shang Liu; Funding acquisition: Jingjing Wang, Haidong Zou, Xiangui He, Xun Xu; Investigation: Bo Zhang, Jinliuxing Yang; Methodology: Shang Liu; Project administration: Jianfeng Zhu, Haidong Zou, Xiangui He, Xun Xu; Resources: Jianfeng Zhu, Haidong Zou, Xiangui He, Xun Xu; Supervision: Xiangui He, Xun Xu; Writing-original draft: Shang Liu; Writing-review & editing: Jun Chen, Zhuoting Zhu, Junyao Zhang, Xiangui He.
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Shanghai General Hospital Ethics Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from children’s parents or legal guardians in this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiangui He and Xun Xu contributed equally as co-last authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Chen, J., Wang, J. et al. Cutoff values of axial length/corneal radius ratio for determining myopia vary with age among 3–18 years old children and adolescents. Graefes Arch Clin Exp Ophthalmol 262, 651–661 (2024). https://doi.org/10.1007/s00417-023-06176-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06176-0