Abstract
Purpose
To compare baseline biometry measurements in eyes with pediatric cataract versus age-matched controls
Methods
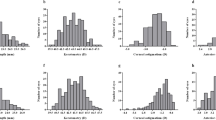
This is a cross-sectional study conducted at a tertiary care hospital that included two arms—prospective arm to collect data from normal eyes and retrospective arm for eyes with pediatric cataract. In the prospective arm, biometry measurements were obtained in healthy children aged 0 to 10 years. Children under the age of four had measurements under anesthesia for an unrelated procedure, while older children had in-office measurements using optical biometry. For comparison, biometric data was collected in children with pediatric cataract through record review. One eye of each patient was randomly selected. Axial length (AL) and keratometry (K) were compared by age and laterality. The medians were compared using Wilcoxon rank-sum tests and variances using Levene’s test.
Results
There were 100 eyes in each arm, 10 eyes in each age bin of 1-year interval. There was more variability in baseline biometry in eyes with pediatric cataract and a trend for longer AL and steeper K in cataract eyes than aged-matched controls. The difference in AL means was significant in age group 2–4 years, and variances were significant across all age groups (p=0.018). Unilateral cataracts (n=49) showed a trend toward greater variability in biometry than bilateral cataracts, but this did not reach statistical significance.
Conclusion
Baseline biometry measures are more variable in eyes with pediatric cataract compared to age-matched controls with a trend toward longer AL and steeper K.




Similar content being viewed by others
References
Infant Aphakia Treatment Study Group, Lambert SR, Lynn MJ, Hartmann EE et al (2014) Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol 132:676–682
Vasavada AR, Nihalani BR (2006) Pediatric cataract surgery. Curr Opin Ophthalmol 17:54–61
Neely DE, Plager DA, Borger SM, Golub RL (2005) Accuracy of intraocular lens calculations in infants and children undergoing cataract surgery. J AAPOS 9:160–165
Nihalani BR, VanderVeen DK (2010) Comparison of intraocular lens power calculation formulae in pediatric eyes. Ophthalmology 117:1493–1499
Vasavada V, Shah SK, Vasavada VA et al (2016) Comparison of IOL power calculation formulae for pediatric eyes. Eye (Lond) 30:1242–1250
Lambert SR, Lynn MJ, DuBois LG et al (2012) Axial elongation following cataract surgery during the first year of life in the infant aphakia treatment study. Invest Ophthalmol Vis Sci 53:7539–7545
Flitcroft DI, Knight-Nanan D, Bowell R et al (1999) Intraocular lenses in children: changes in axial length, corneal curvature, and refraction. Br J Ophthalmol 83:265–269
Fan DSP, Rao SK, Yu CBO et al (2006) Changes in refraction and ocular dimensions after cataract surgery and primary intraocular lens implantation in infants. J Cataract Refract Surg 32:1104–1108
Dahan E, Drusedau MU (1997) Choice of lens and dioptric power in pediatric pseudophakia. J Cataract Refract Surg 23:618–623
Vasavada AR, Raj SM, Nihalani B (2004) Rate of axial growth after congenital cataract surgery. Am J Ophthalmol 138:915–924
Seven E, Tekin S, Batur M et al (2019) Evaluation of changes in axial length after congenital cataract surgery. J Cataract Refract Surg 45:470–474
Khokhar SK, Tomar A, Pillay G, Agarwal E (2019) Biometric changes in Indian pediatric cataract and postoperative refractive status. Indian J Ophthalmol 67:1068–1072
Enyedi LB, Peterseim MW, Freedman SF, Buckley EG (1998) Refractive changes after pediatric intraocular lens implantation. Am J Ophthalmol 126:772–781
Crouch ER, Crouch ER, Pressman SH (2002) Prospective analysis of pediatric pseudophakia: myopic shift and postoperative outcomes. J AAPOS 6:277–282
Plager DA, Kipfer H, Sprunger DT et al (2002) Refractive change in pediatric pseudophakia: 6-year follow-up. J Cataract Refract Surg 28:810–815
Whitmer S, Xu A, McClatchey S (2013) Reanalysis of refractive growth in pediatric pseudophakia and aphakia. J AAPOS 17:153–157
Wilson ME, Trivedi RH, Weakley DR et al (2020) Infant Aphakia Treatment Study Group. Globe axial length growth at age 10.5 years in the infant aphakia treatment study. Am J Ophthalmol 216:147–155
VanderVeen DK, Oke I, Nihalani BR (2022) Deviations from age-adjusted normative biometry measures in children undergoing cataract surgery: implications for postoperative target refraction and IOL power selection. Am J Ophthalmol 239:190–201
Gordon RA, Donzis PB (1985) Refractive development of the human eye. Arch Ophthalmol 103:785–789
Zadnik K, Manny RE, Yu JA et al (2003) Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group. Ocular component data in schoolchildren as a function of age and gender. Optom Vis Sci 80:226–236
Bach A, Villegas VM, Gold AS et al (2019) Axial length development in children. Int J Ophthalmol 12:815–819
Mutti DO, Mitchell GL, Jones LA et al (2005) Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci 46:3074–3080
Trivedi RH, Wilson ME (2007) Biometry data from Caucasian and African-American cataractous pediatric eyes. Invest Ophthalmol Vis Sci 48:4671–4678
Truckenbrod C, Meigen C, Brandt M et al (2021) Longitudinal analysis of axial length growth in a German cohort of healthy children and adolescents. Ophthalmic Physiol Opt 41:532–540
Oke I, Nihalani BR, VanderVeen DK (2023) Axial length and corneal curvature of normal eyes in the first decade of life. Eur J Ophthalmol. https://doi.org/10.1177/11206721231167643
Wiesel TN, Raviola E (1977) Myopia and eye enlargement after neonatal lid fusion in monkeys. Nature 266:66–68
Von Noorden GK, Lewis RA (1987) Ocular axial length in unilateral congenital cataracts and blepharoptosis. Invest Ophthalmol Vis Sci 28:750–752
Gee SS, Tabbara KF (1988) Increase in ocular axial length in patients with corneal opacification. Ophthalmology 95:1276–1278
Rabin J, Van Sluyters RC, Malach R (1981) Emmetropization: a vision-dependent phenomenon. Invest Ophthalmol Vis Sci 20:561–564
Trivedi RH, Wilson ME (2008) Keratometry in pediatric eyes with cataract. Arch Ophthalmol 126:38–42
McClatchey SK, McClatchey TS, Cotsonis G et al (2021) Refractive growth variability in the Infant Aphakia Treatment Study. J Cataract Refract Surg 47:512–515
Funding
Boston Children’s Endowment Fund
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of Boston Children’s Hospital and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Written informed consent was obtained from legal guardians for the prospective arm of the study, while it was not required for the retrospective arm.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nihalani, B.R., Oke, I. & VanderVeen, D.K. Comparison of baseline biometry measures in eyes with pediatric cataract to age-matched controls. Graefes Arch Clin Exp Ophthalmol 261, 3007–3013 (2023). https://doi.org/10.1007/s00417-023-06122-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06122-0