Abstract
Purpose
With the aging population, the prevalence of presbyopia and the popularity of multifocal intraocular lenses is also growing worldwide. Unfortunately, in some cases, they are still associated with postoperative visual disturbances. Recent literature started to evaluate angle kappa- and angle alpha-derived metrics of chord mu and chord alpha as possible predictive values for visual outcomes after multifocal intraocular lens implantation but the published results are inconsistent between studies. Thus, this article aims to review the role of chord mu and chord alpha as postoperative predictors after multifocal intraocular lens implantation and lay the foundation for further research.
Methods
Relevant articles were identified using the following keywords: “presbyopia,” “multifocal intraocular lens,” “angle kappa,” “angle alpha,” “Chord mu,” and “Chord alpha” up to June 2022. An attempt was made to present the majority of publications that addressed the topic.
Conclusions
Chord mu and chord alpha have a predictive role on the outcomes after multifocal intraocular lens implantation but to a different extent. Cataract surgeons should take them into consideration and avoid implanting a multifocal intraocular lens for patients with speculated critical values of chord mu and alpha above 0.5–0.6 mm, depending on the device used for measurement and the multifocal intraocular lens implanted. Currently, chord alpha seems to be a more stable, more widely applicable, and reliable determinant in predicting postoperative outcomes and in patient selection prior to multifocal intraocular lens implantation when compared to chord mu. To draw conclusions on the topic, a controlled study is needed.



Similar content being viewed by others
References
Hoffer KJ, Savini G (2014) Multifocal intraocular lenses: historical perspective. Essentials in Ophthalmology. Springer, New York, pp 5–28
Zvorničanin J, Zvorničanin E (2018) Premium intraocular lenses: the past, present and future. J Curr Ophthalmol 30:287
Keates RH, Pearce JL, Schneider RT (1987) Clinical results of the multifocal lens. J Cataract Refract Surg 13:557–560
Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM et al (2018) Global prevalence of presbyopia and vision impairment from uncorrected presbyopia systematic review, meta-analysis, and modelling. Ophthalmology 125:1492–1499. https://doi.org/10.1016/j.ophtha.2018.04.013
Schallhorn JM, Pantanelli SM, Lin CC, Al-Mohtaseb ZN, Steigleman WA, Santhiago MR et al (2021) Multifocal and accommodating intraocular lenses for the treatment of presbyopia: a report by the American Academy of Ophthalmology. Ophthalmology 128:1469–1482
Salerno L, Tiveron M, Alió J (2017) Multifocal intraocular lenses: types, outcomes, complications and how to solve them. Taiwan J Ophthalmol 7:179
Braga-Mele R, Chang D, Dewey S, Foster G, Henderson BA, Hill W et al (2014) Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cart Refract Surg 40:313–322. https://doi.org/10.1016/j.jcrs.2013.12.011
Prakash G, Prakash DR, Agarwal A, Kumar DA, Jacob S (2011) Predictive factor and kappa angle analysis for visual satisfactions in patients with multifocal IOL implantation. Nature 25:1187–1193
Tchah H, Nam K, Yoo A (2017) Predictive factors for photic phenomena after refractive, rotationally asymmetric, multifocal intraocular lens implantation. Int J Ophthalmol 10:241–245
Qi Y, Lin J, Leng L, Zhao G, Wang Q, Li C, Liting Hu (2018) Role of angle κ in visual quality in patients with a trifocal diffractive intraocular lens. J Cataract Refract Surg 44:949–954
Lee CY, Huang JY, Sun CC, Yang SF, Chen HC, Lin HY (2019) Correlation and predictability of ocular aberrations and the visual outcome after quadrifocal intraocular lens implantation: a retrospective longitudinal study. BMC Ophthalmol 19:188
Chang DH, Waring GO (2014) The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol 158:863–874
Sun H, Fritz A, Dröge G, Neuhann T, Bille JF (2019) Femtosecond-laser-assisted cataract surgery (FLACS). High resolution imaging in microscopy and ophthalmology. Springer, 301–317
Eto T, Teikari P, Najjar RP, Nishimura Y, Motomura Y, Kuze M, Higuchi S (2020) A Purkinje image-based system for an assessment of the density and transmittance spectra of the human crystalline lens in vivo. Sci Rep 10:1–12
Rodríguez-Vallejo M, Piñero DP, Fernández J (2019) Avoiding misinterpretations of Kappa angle for clinical research studies with Pentacam. J Optom 12:71
Holladay JT (2019) Apparent chord mu and actual chord mu and their clinical value. J Cataract Refract Surg 45:1198–1199
Orbscan II and IIz Operators Manual Software 3.12 - Version 2.1 Available at: https://www.bioclinicalservices.com.au/bausch-lomb/corneal-topography-systems--2/orbscan-ii-and-iiz-operators-manual-software-3-12-version-2-1. Accessed: 13 June 2023
Sella R, Shouchane-Blum K, Reitblat O, Bahar I (2022) The association between pupil diameter and apparent chord mu length value. Investig Ophthalmol Vis Sci 63:1698
Qin M, Yuan Y, Wang Y, Li P, Chen W, Wang Y et al (2022) Comparison of preoperative angle kappa measurements in the eyes of cataract patients obtained from Pentacam Scheimpflug system, optical low-coherence reflectometry, and ray-tracing aberrometry. BMC Ophthalmol 22:1–9
Fu Y, Kou J, Chen D, Wang D, Zhao Y, Hu M et al (2019) (2019): Influence of angle kappa and angle alpha on visual quality after implantation of multifocal intraocular lenses. J Cataract Refract Surg 45:1258–1264
Rocha-De-lossada C, Sánchez-González JM, Borroni D, Llorens-Bellés V, Rachwani-Anil R, Torras-Sanvicens J et al (2021) Chord mu (µ) and chord alpha (α) length changes in fuchs endothelial corneal dystrophy before and after Descemet membrane endothelial keratoplasty (DMEK) surgery. J Clin Med 10:4844
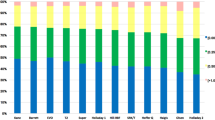
Baenninger PB, Rinert J, Bachmann LM, Iselin KC, Sanak F, Pfaeffli O et al (2022) Distribution of preoperative angle alpha and angle kappa values in patients undergoing multifocal refractive lens surgery based on a positive contact lens test. Graefes Arch Clin Exp Ophthalmol 260:621–628
Cervantes-Coste G, Tapia A, Corredor-Ortega C, Osorio M, Valdez R et al (2022) The influence of angle alpha, angle kappa, and optical aberrations on visual outcomes after the implantation of a high-addition trifocal IOL. J Clin Med 11:896
Meng J, Du Y, Wei L, Yao Y, He W, Qian D et al (2021) Distribution of angle α and angle κ in a population with cataract in Shanghai. J Cataract Refract Surg 47:579–584
Jiang JY, Hodge C, Lawless M (2020) Understanding chord mu through a large population-based study. Clin Exp Ophthalmol 48:998–1001
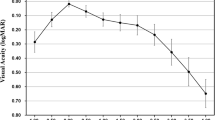
Miháltz K, Vécsei-Marlovits PV (2021) The impact of visual axis position on the optical quality after implantation of multifocal intraocular lenses with different asphericity values. Graefe’s Arch Clin Exp Ophthalmol 259:673–683
Mahr MA, Simpson MJ, Erie JC (2020) Angle alpha orientation and magnitude distribution in a cataract surgery population. J Cataract Refract Surg 46:372–377
Velasco-Barona C, Corredor-Ortega C, Avendaño-Domínguez A, Cervantes-Coste G, Cantú-Treviño MP, Gonzalez-Salinas R (2021) Impact of correlation of angle α with ocular biometry variables. J Cataract Refract Surg 47:1279–1284
Basmak H, Sahin A, Yildirim N, Papakostas TD, Kanellopoulos AJ (2007) Measurement of angle kappa with synoptophore and Orbscan II in a normal population. J Refract Surg 23:456–460
Sivakumar S, Sivakumar (2019) Angle kappa in myopes and hyperopes and its role in multifocal lens implantations. Investig Ophthalmol Vis Sci 60:516
Ranka MP, Steele MA (2015) Esotropia associated with high myopia. Curr Opin Ophthalmol 26:362–365
Prakash G, Agarwal A, Prakash DR, Kumar DA, Agarwal A, Jacob S (2011) Role of angle kappa in patient dissatisfaction with refractive-design multifocal intraocular lenses. J Cataract Refract Surg 37:1739–1740
Park CY, Oh SY, Chuck RS (2012) Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol 23:269–275
Karhanova M, Marešova K, Pluhaček F, Mlčak P, Vlačil O, Sín M (2013) The importance of angle kappa for centration of multifocal intraocular lenses. Cesk Slov Oftalmol 69:64–68
Madrid-Costa D, Pérez-Vives C, Ruiz-Alcocer J, Albarrán-Diego C, Montés-Micó R (2012) Visual simulation through different intraocular lenses in patients with previous myopic corneal ablation using adaptive optics: effect of tilt and decentration. J Cataract Refract Surg 38:774–786
Hayashi K, Hayashi H, Nakao F, Hayashi F (2001) Correlation between pupillary size and intraocular lens decentration and visual acuity of a zonal-progressive multifocal lens and a monofocal lens. Ophthalmology 108:2011–2017
Ashena Z, Maqsood S, Ahmed SN, Nanavaty MA (2020) Effect of intraocular lens tilt and decentration on visual acuity, dysphotopsia and wavefront aberrations. Vision 4:41
Soda M, Yaguchi S (2012) Effect of decentration on the optical performance in multifocal intraocular lenses. Ophthalmologica 227:197–204
Tabernero J, Benito A, Nourrit V, Artal P, Liang BJ, Grimm S (2006) Instrument for measuring the misalignments of ocular surfaces. Optics Express 14:10945–56
Moshirfar M, Hoggan R, Muthappan V (2013) Angle kappa and its importance in refractive surgery. Oman J Ophthalmol 6:151
Sun M, Alarcon A, Canovas C, State M, Weeber HA, Domingo J, Piers P (2018) The effect of angle kappa in visual performance in diffractive intraocular lenses. Investig Ophthalmol Vis Sci 59:2966
Karhanová M, Pluháček F, Mlčák P, Vláčil O, Šín M, Marešová K (2015) The importance of angle kappa evaluation for implantation of diffractive multifocal intra-ocular lenses using pseudophakic eye model. Acta Ophthalmol 93:123–128
Berdahl JP, Waring GO (2012) Match right lens to patient needs: 10 objective measurements can improve multifocal IOL implantation outcomes. Ophthalmol Times 1:28–29
Garzón N, García-Montero M, López-Artero E, Albarrán-Diego C, Pérez-Cambrodí R, Illarramendi I, Poyales F (2020) Influence of angle κ on visual and refractive outcomes after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg 46:721–727
Liu Y, Gao Y, Liu R, Hu C, Ma B, Miao J et al (2020) Influence of angle kappa-customized implantation of rotationally asymmetric multifocal intraocular lens on visual quality and patient satisfaction. Acta Ophthalmol 98:734–742
Velasco-Barona C, Corredor-Ortega C, Mendez-Leon A, Casillas-Chavarín NL, Valdepeña-López Velarde D, Cervantes-Coste G et al (2019) Influence of angle and higher-order aberrations on visual quality employing two diffractive trifocal IOLs. J Ophthalmol 7018937
Bonaque-González S, Jaskulski MT, Carmona-Ballester D, Pareja-Ríos A, Trujillo-Sevilla JM (2021) Influence of angle kappa on the optimal intraocular orientation of asymmetric multifocal intraocular lenses. J Optom 14:78
Kumar DA, Agarwal A, Agarwal A, Prakash G, Jacobet S (2011) Glued intraocular lens implantation for eyes with defective capsules: a retrospective analysis of anatomical and functional outcome. Saudi J Ophthalmol 25:245
Solomon R, Barsam A, Voldman A, Holladay J, Bhogal M, Perry HD, Donnenfeld ED (2012) Argon laser iridoplasty to improve visual function following multifocal intraocular lens implantation. J Refract Surg 28:281–283
Melki SA, Harissi-Dagher M (2011) Coaxially sighted intraocular lens light reflex for centration of the multifocal single piece intraocular lens. Can J Ophthalmol 46:319–321
Assia EI, Wong JXH, Shochot Y (2020) The effect on post-operative intraocular lens centration by manual intraoperative centration versus auto-centration. Clin Ophthalmol 14:3475
Xie T, Liu X, Zhu J, Li X (2021) Effect of capsular tension ring on optical and multifunctional lens position outcomes: a systematic review and a meta-analysis. Int Ophthalmol 41:3971–3984
Miyoshi T, Fujie S, Yoshida H, Iwamoto H, Tsukamoto H, Oshika T (2020) Effects of capsular tension ring on surgical outcomes of premium intraocular lens in patients with suspected zonular weakness. PLoS ONE 15(2):e0228999
Piracha AR (2016) Using angle alpha in premium IOL screening. Cataract Refract Surg Today 16:5
Wang L, Guimaraes de Souza R, Weikert MP, Koch DD (2019) Evaluation of crystalline lens and intraocular lens tilt using a swept-source optical coherence tomography biometer. J Cataract Refract Surg 45:35–40
Li Z, Zhu Z, Li X, Meng Z, Qu W, Zhao Y (2021) Age-related changes in crystalline lens tilt and decentration: swept-source OCT study. J Cataract Refract Surg 47:1290–1295
Wang R, Long T, Gu X, Ma T (2020) Changes in angle kappa and angle alpha before and after cataract surgery. J Cataract Refract Surg 46:365–371
Qin M, Ji M, Zhou T, Yuan Y, Luo J, Li P et al (2022) Influence of angle alpha on visual quality after implantation of extended depth of focus intraocular lenses. BMC Ophthalmol 22:1–11
Sandoval HP, Potvin R, Solomon KD (2022) The effects of angle Kappa on clinical results and patient-reported outcomes after implantation of a trifocal intraocular lens. Clin Ophthalmol 16:1321–1329
Fischinger I, Seiler TG, Schmidinger G, Seiler T (2015) Verschiebung des Pupillenzentroids. Der Ophthalmol 112:661–664
Ordiñaga-Monreal E, Castanera-Gratacós D, Castanera F, Fambuena-Muedra I, Vega F, Millán MS (2022) Pupil size differences between female and male patients after cataract surgery. J Optom 15:179–185
Kanellopoulos AJ, Asimellis G, Georgiadou S (2015) Digital pupillometry and centroid shift changes after cataract surgery. J Cataract Refract Surg 41:408–414
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
Andrzej Grzybowki reports lecture fees from Viatris, Thea, Polpharma, Alcon, Topcon, and grants from Bausch& Lomb, Johnson & Johnson, Zeiss, Oculentis, Alcon, and Ocustar. Other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Montrimas, A., Žemaitienė, R., Yao, K. et al. Chord mu and chord alpha as postoperative predictors in multifocal intraocular lens implantation. Graefes Arch Clin Exp Ophthalmol 262, 367–380 (2024). https://doi.org/10.1007/s00417-023-06098-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06098-x