Abstract
Purpose
To compare drusen size metrics (apical height and basal width) on optical coherence tomography (OCT) B-scans with their size assessed on color photos in eyes with age-related macular degeneration (AMD) and normal aging.
Methods
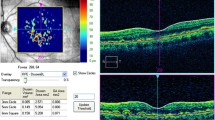
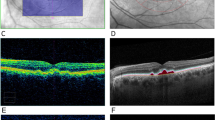
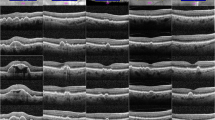
A total of 508 drusen were evaluated in this analysis. Flash color fundus photos (CFP), infrared reflectance (IR) images, and OCT B-scans obtained at the same visit were evaluated. Individual drusen were identified on CFPs and the diameters of the drusen were measured in planimetric grading software. CFPs were manually registered to the IR image with their corresponding OCT volume. After confirming correspondence between the CFP and OCT, the apical height and basal width of the same drusen were measured on OCT B-scans.
Results
Drusen were divided into small, medium, large, and very large categories based on their diameter on the CFP images (< 63, 63 to 124, 125 to 249, and \(\ge\) 250 μm, respectively). The OCT apical height of small drusen on CFP ranged from 20 to 31 μm, while medium drusen ranged from 31 to 46 μm, large drusen ranged from 45 μm to 111 µm, and very large drusen ranged from 55 μm to 208 μm. The OCT basal width measured < 99 μm in small drusen, from 99 to 143 μm in medium drusen, from 141 to 407 µm in large drusen, and > 209 µm in very large drusen.
Conclusion
Drusen of different size categories on color photographs may also be separated according to their apical height and basal width on OCT. The apical height and basal width ranges defined in this analysis may be of value in the design of an OCT-based grading scale for AMD.



Similar content being viewed by others
Data availability
The data used to support these findings of this study are available from the corresponding author upon request.
References
Friedman DS, O’Colmain BJ, Muñoz B et al (2004) Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol 122:564–572
Bressler NM, Bressler SB, Congdon NG et al (2003) Potential public health impact of Age-Related Eye Disease Study results: AREDS report no. 11. Arch Ophthalmol 121:1621–1624
Age-Related Eye Disease Study Research Group (2001) The Age-Related Eye Disease Study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: the Age-Related Eye Disease Study Report Number 6. Am J Ophthalmol 132:668–681
Meyer CH, Saxena S, Sadda SR (2017) Spectral domain optical coherence tomography in macular diseases. Springer India
Gheorghe A, Mahdi L, Musat O (2015) Age-related macular degeneration. Rom J Ophthalmol 59:74–77
Ferris FL 3rd, Wilkinson CP, Bird A et al (2013) Clinical classification of age-related macular degeneration. Ophthalmology 120:844–851
Zhang X, Sivaprasad S (2021) Drusen and pachydrusen: the definition, pathogenesis, and clinical significance. Eye 35:121–133
Klein R, Klein BEK, Tomany SC et al (2002) Ten-year incidence and progression of age-related maculopathy: The Beaver Dam eye study. Ophthalmology 109:1767–1779
Davis MD, Gangnon RE, Lee L-Y et al (2005) The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS Report No. 17. Arch Ophthalmol 123:1484–1498
Wang JJ, Foran S, Smith W, Mitchell P (2003) Risk of age-related macular degeneration in eyes with macular drusen or hyperpigmentation: the Blue Mountains Eye Study cohort. Arch Ophthalmol 121:658–663
Ferris FL, Davis MD, Clemons TE et al (2005) A simplified severity scale for age-related macular degeneration: AREDS Report No. 18. Arch Ophthalmol 123:1570–1574
Elsevier [No title]. https://www.elsevier.com/books/handbook-of-retinal-oct-optical-coherence-tomography/978-0-323-75772-0. Accessed 13 Aug 2022
Yehoshua Z, Wang F, Rosenfeld PJ et al (2011) Natural history of drusen morphology in age-related macular degeneration using spectral domain optical coherence tomography. Ophthalmology 118:2434–2441
Nittala MG, Song YE, Sardell R et al (2019) Amish Eye Study: baseline spectral domain optical coherence tomography characteristics of age-related macular degeneration. Retina 39:1540–1550
Gabriele ML, Wollstein G, Ishikawa H et al (2010) Three dimensional optical coherence tomography imaging: advantages and advances. Prog Retin Eye Res 29:556–579
Phadikar P, Saxena S, Ruia S et al (2017) The potential of spectral domain optical coherence tomography imaging based retinal biomarkers. Int J Retina Vitreous 3:1
Spaide RF, Curcio CA (2010) Drusen characterization with multimodal imaging. Retina 30:1441–1454
Holz FG, Sadda SR, Staurenghi G et al (2017) Imaging protocols in clinical studies in advanced age-related macular degeneration: recommendations from Classification of Atrophy Consensus Meetings. Ophthalmology 124:464–478
Sadda SR, Guymer R, Holz FG et al (2018) Consensus definition for atrophy associated with age-related macular degeneration on OCT: Classification of Atrophy Report 3. Ophthalmology 125:537–548
Farsiu S, Chiu SJ, O’Connell RV et al (2014) Quantitative classification of eyes with and without intermediate age-related macular degeneration using optical coherence tomography. Ophthalmology 121:162–172
Yu JJ, Agrón E, Clemons TE et al (2019) Natural history of drusenoid pigment epithelial detachment associated with age-related macular degeneration: Age-Related Eye Disease Study 2 Report No. 17. Ophthalmology 126:261–273
Nittala MG, Ruiz-Garcia H, Sadda SR (2012) Accuracy and reproducibility of automated drusen segmentation in eyes with non-neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 53:8319–8324
Freeman SR, Kozak I, Cheng L et al (2010) Optical coherence tomography-raster scanning and manual segmentation in determining drusen volume in age-related macular degeneration. Retina 30:431–435
de Sisternes L, Simon N, Tibshirani R et al (2014) Quantitative SD-OCT imaging biomarkers as indicators of age-related macular degeneration progression. Invest Ophthalmol Vis Sci 55:7093–7103
Dieaconescu DA, Dieaconescu IM, Williams MA et al (2012) Drusen height and width are highly predictive markers for progression to neovascular AMD. Invest Ophthalmol Vis Sci 53:2910–2910
Gregori G, Yehoshua Z, Garcia Filho CA, de A, et al (2014) Change in drusen area over time compared using spectral-domain optical coherence tomography and color fundus imaging. Invest Ophthalmol Vis Sci 55:7662–7668
Jain N, Farsiu S, Khanifar AA et al (2010) Quantitative comparison of drusen segmented on SD-OCT versus drusen delineated on color fundus photographs. Invest Ophthalmol Vis Sci 51:4875–4883
Göbel AP, Fleckenstein M, Heeren TFC et al (2016) In-vivo mapping of drusen by fundus autofluorescence and spectral-domain optical coherence tomography imaging. Graefes Arch Clin Exp Ophthalmol 254:59–67
Cheung CMG, Shi Y, Tham YC et al (2018) Correlation of color fundus photograph grading with risks of early age-related macular degeneration by using automated OCT-derived drusen measurements. Sci Rep 8:12937
Diniz B, Ribeiro R, Heussen FM et al (2014) Drusen measurements comparison by fundus photograph manual delineation versus optical coherence tomography retinal pigment epithelial segmentation automated analysis. Retina 34:55–62
Laura K, Laurie D, Min S et al (2016) Predictors of macular atrophy detected by fundus autofluorescence in patients with neovascular age-related macular degeneration after long-term ranibizumab treatment. Ophthalmic Surg Lasers Imaging Retina 47:224–231
Nittala MG, Amirhossein H, Wong WT et al (2015) Image scaling difference between a confocal scanning laser ophthalmoscope and a flash fundus camera. Ophthalmic Surg Lasers Imaging Retina 46:872–879
Yehoshua Z, Gregori G, Sadda SR et al (2013) Comparison of drusen area detected by spectral domain optical coherence tomography and color fundus imaging. Invest Ophthalmol Vis Sci 54:2429–2434
Kim DY, Loo J, Farsiu S, Jaffe GJ (2021) Comparison of single drusen size on color fundus photography and spectral-domain optical coherence tomography. Retina 41:1715–1722
Funding
Research reported in this publication was supported by the National Eye Institute of the National Institutes of Health under Award Number RO1EY023164 and R01EY030614.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of California – Los Angeles Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Dr. Sadda has served as a consultant for Amgen, Allergan, Genentech/Roche, Iveric, Oxurion, Novartis, Regeneron, Pfizer, 4DMT, Centervue, Heidelberg, Optos, Nanoscope, Apellis, and Jannsen. He has received speaker fees from Carl Zeiss Meditec, Nidek, and Novartis. He has received research instruments from Nidek, Topcon, Heidelberg, Carl Zeiss Meditec, Optos, and Centervue. The remaining authors have no conflict of interest to disclose.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Srinivas R. Sadda: although the co-author is an Editor of the journal, he had no involvement with the peer review process for this article.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oncel, D., Corradetti, G., Wakatsuki, Y. et al. Drusen morphometrics on optical coherence tomography in eyes with age-related macular degeneration and normal aging. Graefes Arch Clin Exp Ophthalmol 261, 2525–2533 (2023). https://doi.org/10.1007/s00417-023-06088-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06088-z