Abstract
Purpose
To investigate color vision deficiency and the value of Hardy-Rand-Rittler (HRR) color plates in monitoring dysthyroid optic neuropathy (DON) to improve the diagnosis of DON.
Methods
The participants were divided into DON and non-DON (mild and moderate-to-severe) groups. All the subjects underwent HRR color examination and comprehensive ophthalmic examinations. The random forest and decision tree models based on the HRR score were constructed by R software. The ROC curve and accuracy of different models in diagnosing DON were calculated and compared.
Results
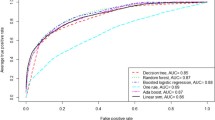
Thirty DON patients (57 eyes) and sixty non-DON patients (120 eyes) were enrolled. The HRR score was lower in DON patients than in non-DON patients (12.1 ± 6.2 versus 18.7 ± 1.8, p < 0.001). The major color deficiency was red-green deficiency in DON using HRR test. The HRR score, CAS, RNFL, and AP100 were found to be important factors in predicting DON from random forest and selected by decision tree to construct the multifactor model. The sensitivity, specificity, and the area under the curve (AUC) of the HRR score were 86%, 72%, and 0.87, respectively. The HRR score decision tree had a sensitivity, specificity, and AUC of 93%, 57%, and 0.75, respectively, with an accuracy of 82%. The data of the multifactor decision tree were 90%, 89%, and 0.93 for sensitivity, specificity, and AUC, respectively, with an accuracy of 91%.
Conclusion
The HRR test was valid as screening method for DON. The multifactor decision tree based on the HRR test improved the diagnostic efficacy for DON. An HRR score of less than 12 and red-green deficiency may be characteristic of DON.






Similar content being viewed by others
References
Neigel JM, Rootman J, Belkin RI, Nugent RA, Spinelli JA (1988) Dysthyroid optic neuropathy. The crowded orbital apex syndrome. Ophthalmology 95:1515–1521
Soni C, Johnson L (2010) Visual neuropraxia and progressive vision loss from thyroid-associated stretch optic neuropathy. Eur J Ophthalmol 20:429–436. https://doi.org/10.1177/112067211002000226
Bain AC, Meaney DF (2000) Tissue-level thresholds for axonal damage in an experimental model of central nervous system white matter injury. J Biomech Eng 122:615–622
Bain AC, Raghupathi R, Meaney DF (2001) Dynamic stretch correlates to both morphological abnormalities and electrophysiological impairment in a model of traumatic axonal injury. J Neurotrauma 18:499
Blandford A, Zhang D, Chundury R, Perry J (2017) Dysthyroid optic neuropathy: update on pathogenesis, diagnosis, and management. Expert Rev Ophthalmol 12:111–121. https://doi.org/10.1080/17469899.2017.1276444
Tagami M, Honda S, Azumi A (2022) Insights into current management strategies for dysthyroid optic neuropathy: a review. J Clin Ophthalmol 16:841–850. https://doi.org/10.2147/opth.S284609
Fichter N, Guthoff RF, Schittkowski MP (2012) Orbital decompression in thyroid eye disease. ISRN Ophthalmol 2012:739236
Char DH (1996) Thyroid eye disease. Br J Ophthalmol 80:922
McKeag D, Lane C, Lazarus J et al (2007) Clinical features of dysthyroid optic neuropathy: a European Group on Graves’ Orbitopathy (EUGOGO) survey. Br J Ophthalmol 91:455–458. https://doi.org/10.1136/bjo.2006.094607
Dolman P (2021) Dysthyroid optic neuropathy: evaluation and management. J Endocrinol Invest 44:421–429. https://doi.org/10.1007/s40618-020-01361-y
Tagami M, Honda S, Azumi A (2020) Preoperative clinical factors and visual outcomes following orbital decompression with dysthyroid optic neuropathy. BMC Ophthalmol 20:30. https://doi.org/10.1186/s12886-020-1314-8
Jeon C, Shin J, Woo K, Kim Y (2012) Clinical profile and visual outcomes after treatment in patients with dysthyroid optic neuropathy. Korean J Ophthalmol 26:73–79. https://doi.org/10.3341/kjo.2012.26.2.73
Nichols BE, Thompson HS, Stone EM (1997) Evaluation of a significantly shorter version of the Farnsworth-Munsell 100-hue test in patients with three different optic neuropathies. J Neuroophthalmol 17:1
Kuebler AG, Halfter K, Reznicek L, Klingenstein A, Priglinger S, Rudolph G, Hintschich C (2021) A pathological indicator for dysthyroid optic neuropathy: tritan color vision deficiency. Graefes Arch Clin Exp Ophthalmol 259:3421–3426
Kuebler AG, Halfter K, Reznicek L, Klingenstein A, Priglinger S, Hintschich C (2021) Subclinical dysthyroid optic neuropathy: tritan deficiency as an early sign of dysthyroid optic neuropathy. Br J Ophthalmol 105:1019–1023
Currò N, Covelli D, Vannucchi G et al (2014) Therapeutic outcomes of high-dose intravenous steroids in the treatment of dysthyroid optic neuropathy. Thyroid 24:897–905
Baril C, Pouliot D, Molgat Y (2014) Optic neuropathy in thyroid eye disease: results of the balanced decompression technique. Can J Ophthalmol 49:162–166. https://doi.org/10.1016/j.jcjo.2013.10.006
Wei Y, Chi M, Liao S (2011) Predictability of visual function and nerve fiber layer thickness by cross-sectional areas of extraocular muscles in graves ophthalmopathy. Am J Ophthalmol 151:901-906.e1. https://doi.org/10.1016/j.ajo.2010.11.001
Perry JD, Kadakia A, Foster J (2003) Transcaruncular orbital decompression for dysthyroid optic neuropathy. Ophthalmic Plast Reconstr Surg 19:353–358. https://doi.org/10.1097/01.Iop.0000083645.19368.99
Pelewicz M, Rymuza J, Pelewicz K, Miśkiewicz P (2022) Dysthyroid optic neuropathy: treatment with additional intravenous methylprednisolone pulses after the basic schedule is associated with stabilization or further improvement of clinical outcome. J Clin Med 11(8):2068. https://doi.org/10.3390/jcm11082068
Huna-Baron R, Glovinsky Y, Habot-Wilner Z (2013) Comparison between Hardy-Rand-Rittler 4th edition and Ishihara color plate tests for detection of dyschromatopsia in optic neuropathy. Graefes Arch Clin Exp Ophthalmol 251:585–589. https://doi.org/10.1007/s00417-012-2073-x
Belcher SJ, Greenshields KW, Wright WD (1958) Colour vision survey using the Ishihara, Dvorine, Boström and Kugelberg, Boström, and American-Optical Hardy-Rand-Rittler tests. Br J Ophthalmol 42:355
Crone RA (1961) Quantitative diagnosis of defective color vision. A comparative evaluation of the Ishihara test, the Farnsworth dichotomous test and the Hardy-Rand-Rittler polychromatic plates. Am J Ophthalmol 51:298–305
Cole BL, Lian KY, Lakkis C (2010) The new Richmond HRR pseudoisochromatic test for colour vision is better than the Ishihara test. Clin Exp Optom 89:73–80
Foote K, Neitz M, Neitz J (2014) Comparison of the Richmond HRR 4th edition and Farnsworth-Munsell 100 Hue Test for quantitative assessment of tritan color deficiencies. J Opt Soc Am A Opt Image Sci Vis 31: A186–188 https://doi.org/10.1364/josaa.31.00a186
Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly G, Marcocci C, Perros P, Salvi M, Wiersinga W (2016) The 2016 European Thyroid Association/European Group on Graves’ orbitopathy guidelines for the management of Graves’ orbitopathy. Eur Thyroid J 5:9–26. https://doi.org/10.1159/000443828
Mourits MP, Prummel MF, Wiersinga WM, Koornneef L (1997) Clinical activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin Endocrinol 47:9–14
Hardy LH, Rand G, Rittler MC (1954) The H-R-R polychromatic plates. II. Comparison of qualitative and quantitative classifications by H-R-R plates and other tests. AMA Arch Ophthalmol 52:353
Hardy LH, Rand G, Rittler MC (1954) H–R–R polychromatic plates. J Opt Soc Am 44:509–523. https://doi.org/10.1364/JOSA.44.000509
Bailey J, Neitz M, Tait D, Neitz J (2004) Evaluation of an updated HRR color vision test. Vis Neurosci 21:431–436. https://doi.org/10.1017/s0952523804213463
Dain SJ (2004) Colorimetric analysis of four editions of the Hardy-Rand-Rittler pseudoisochromatic tests. Vis Neurosci 21:437–443
McCully TJ, Golnik KC, Lam BL, Feuer WJ (2006) The effect of decreased visual acuity on clinical color vision testing. Am J Ophthalmol 141:194–196
Dave P, Villarreal G Jr, Friedman DS, Kahook MY, Ramulu PY (2015) Ability of bottle cap color to facilitate accurate patient-physician communication regarding medication identity in patients with glaucoma. Ophthalmology 122:2373–2379
Melamud A, Hagstrom S, Traboulsi E (2004) Color vision testing. Ophthalmic Genet 25:159–187. https://doi.org/10.1080/13816810490498341
Ng JS, Shih B (2017) Level of visual acuity necessary to avoid false-positives on the HRR and Ishihara color vision tests. Eur J Ophthalmol 27:363–366. https://doi.org/10.5301/ejo.5000855
Solomon SG, Lennie P (2007) The machinery of colour vision. Nat Rev Neurosci 8:276–286. https://doi.org/10.1038/nrn2094
Hendry SH, Calkins DJ (1998) Neuronal chemistry and functional organization in the primate visual system. Trends Neurosci 21:344–349. https://doi.org/10.1016/s0166-2236(98)01245-4
Cox J (1960) Colour vision defects acquired in diseases of the eye. Br J Physiol Opt 17:195–216
Hart WM (1987) Acquired dyschromatopsias. Surv Ophthalmol 32:10–31
Wu Y, Tu Y, Wu C, Bao L, Wang J, Lu F, Shen M, Chen Q (2020) Reduced macular inner retinal thickness and microvascular density in the early stage of patients with dysthyroid optic neuropathy. Eye Vis 7:16. https://doi.org/10.1186/s40662-020-00180-9
Pérez-López M, Sales-Sanz M, Rebolleda G, Casas-Llera P, González-Gordaliza C, Jarrín E, Muñoz-Negrete F (2011) Retrobulbar ocular blood flow changes after orbital decompression in Graves’ ophthalmopathy measured by color Doppler imaging. Invest Ophthalmol Vis Sci 52:5612–5617. https://doi.org/10.1167/iovs.10-6907
Guo J, Li X, Ma R, Gan L, Qian J (2022) The changes of retinal nerve fibre layer and ganglion cell layer with different severity of thyroid eye disease. Eye 36:129–134. https://doi.org/10.1038/s41433-021-01453-w
Goel R, Shah S (2022) Ganglion cell layer thickness - a marker for early dysthyroid optic neuropathy. Eye (Lond) 36(11):2224. https://doi.org/10.1038/s41433-022-02035-0
Johnson BT, Jameyfield E, Aakalu VK (2021) Optic neuropathy and diplopia from thyroid eye disease: update on pathophysiology and treatment. Curr Opin Neurol 34:116–121. https://doi.org/10.1097/wco.0000000000000894
Zarazaga AF, Vásquez JG, Royo VP (2019) Review of the main colour vision clinical assessment tests. Arch Soc Esp Oftalmol 94:25–32. https://doi.org/10.1016/j.oftal.2018.08.006
Monteiro M, Portes A, Moura F, Regensteiner D (2008) Using frequency-doubling perimetry to detect optic neuropathy in patients with Graves’ orbitopathy. Jpn J Ophthalmol 52:475–482. https://doi.org/10.1007/s10384-008-0579-x
Qi X, Tong B, Hu W, Luo BJE (2021) Comparing isolated-check visual evoked potential, pattern visual evoked potential, and standard automated perimetry in dysthyroid optic neuropathy eyes. Eye 35:2556–2563. https://doi.org/10.1038/s41433-020-01274-3
Acknowledgements
Support from numerous colleagues, friends, and experts from Sun Yat-sen Memorial Hospital of Sun Yat-sen University is gratefully acknowledged. The article is dedicated to the members of our research group who have helped a lot.
Funding
This study was supported by research grants from the Science and Technology Bureau of Guangzhou (grant numbers 2021–02-01–04-0203) and the Sun Yat-Sen Clinical Research Cultivating Program.
Author information
Authors and Affiliations
Contributions
All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consents to participate
This study adhered to the tenets of the Declaration of Helsinki and was approved by the research ethics committee of Sun Yat-sen Memorial Hospital, Sun Yat-sen University, China (SYSKY-2022–232-01). Informed consent was obtained from all patients included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiaqi Liang and Peng Tian have contributed equally to this work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, J., Tian, P., Wang, J. et al. A diagnostic model based on color vision examination for dysthyroid optic neuropathy using Hardy-Rand-Rittler color plates. Graefes Arch Clin Exp Ophthalmol 261, 2669–2678 (2023). https://doi.org/10.1007/s00417-023-06062-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06062-9