Abstract
Purpose
To investigate the accuracy of modern intraocular lens (IOL) power calculation formulas in eyes with axial length (AL) ≥ 26.00 mm.
Methods
A total of 193 eyes with one type of lens were analysed. An IOL Master 700 (Carl Zeiss Meditec, Jena, Germany) was used for optical biometry. Thirteen formulas and their modifications were evaluated: Barrett Universal II, Haigis, Hoffer QST, Holladay 1 MWK, Holladay 1 NLR, Holladay 2 NLR, Kane, Naeser 2, SRK/T, SRK/T MWK, T2, VRF and VRF-G. The User Group for Laser Interference Biometry lens constants were used for IOL power calculation. The mean prediction error (PE) and its standard deviation (SD), the median absolute error (MedAE), the mean absolute error (MAE) and the percentage of eyes with PEs within ± 0.25 D, ± 0.50 D and < ± 1.00 D were calculated.
Results
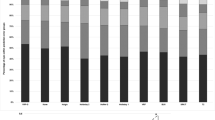
The modern formulas (Barrett Universal II, Hoffer QST, Kane, Naeser 2 and VRF-G) produced the smallest MedAE among all methods (0.30 D, 0.30 D, 0.30 D, 0.29 D and 0.28 D, respectively). The percentage of eyes with a PE within ± 0.50 D ranged from 67.48% to 74.85% for SRK/T and Hoffer QST, Naeser 2 and VRF-G, respectively.
Conclusions
Dunn’s post hoc test of the absolute errors revealed statistically significant differences (P < 0.05) between some of the newer formulas (Naeser 2 and VRF-G) and the remaining ones. From a clinical perspective the Hoffer QST, Naeser 2 and VRF-G formulas were more accurate predictors of postoperative refraction with the largest proportion of eyes within ± 0.50 D.



Similar content being viewed by others
References
Shammas J, Taroni L, Pellegrini M et al (2022) Accuracy of newer IOL power formulas in short and long eyes using sum-of-segments biometry. J Cataract Refract Surg 48:1113–1120. https://doi.org/10.1097/j.jcrs.0000000000000958
Hoffer KJ, Savini G (2017) IOL power calculation in short and long eyes. Asia Pac J Ophthalmol (Phila) 6:330–331. https://doi.org/10.22608/APO.2017338.
Voytsekhivskyy O, Hoffer KJ, Savini G, Tutchenko L, Hipólito-Fernandes D (2021) Clinical Accuracy of 18 IOL power formulas in 241 short eyes. Curr Eye Res 46:1832–1843. https://doi.org/10.1080/02713683.2021.1933056
Liu J, Wang L, Chai F et al (2019) Comparison of intraocular lens power calculation formulas in Chinese eyes with axial myopia. J Cataract Refract Surg 45:725–731. https://doi.org/10.1016/j.jcrs.2019.01.018
Lin L, Xu M, Mo E et al (2021) Accuracy of newer generation IOL power calculation formulas in eyes with high axial myopia. J Refract Surg 37:754–758. https://doi.org/10.3928/1081597X-20210712-08
Mo E, Lin L, Wang J et al (2021) Clinical Accuracy of 6 intraocular lens power calculation formulas in elongated eyes, according to anterior chamber depth. Am J Ophthalmol 233:153–162. https://doi.org/10.1016/j.ajo.2021.07.017
Norrby S (2008) Sources of error in intraocular lens power calculation. J Cataract Refract Surg 34:368–376. https://doi.org/10.1016/j.jcrs.2007.10.031
Zaldivar R, Shultz MC, Davidorf MJ, Holladay JT (2000) Intraocular lens power calculations in patients with extreme myopia. J Cataract Refract Surg 26:668–674. https://doi.org/10.1016/s0886-3350(00)00367-9
MacLaren RE, Sagoo MS, Restori M, Allan BDS (2005) Biometry accuracy using zero- and negative-powered intraocular lenses. J Cataract Refract Surg 31:280–290. https://doi.org/10.1016/j.jcrs.2004.04.054
Haigis W, Lege B, Miller N, Schneider B (2000) Comparison of immersion ultrasound biometry and partial coherence interferometry for IOL calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 238:765–773. https://doi.org/10.1007/s004170000188
Wang L, Shirayama M, Ma XJ, Kohnen T, Koch DD (2011) Optimizing intraocular lens power calculations in eyes with axial lengths above 25.0 mm. J Cataract Refract Surg 37:2018–2027. https://doi.org/10.1016/j.jcrs.2011.05.042
Savini G, Hoffer KJ, Shammas HJ et al (2017) Accuracy of a new swept-source optical coherence tomography biometer for IOL power calculation and comparison to IOLMaster. J Refract Surg 33:690–695. https://doi.org/10.3928/1081597X-20170721-05
Hoffer KJ, Hoffmann PC, Savini G (2016) Comparison of a new optical biometer using swept-source optical coherence tomography and a biometer using optical low-coherence reflectometry. J Cataract Refract Surg 42:1165–1172. https://doi.org/10.1016/j.jcrs.2016.07.013
Barret GD (1993) An improved universal theoretical formula for intraocular lens power prediction. J Cataract Refract Surg 19:713–720. https://doi.org/10.1016/s0886-3350(13)80339-2
Holladay JT, Prager TC, Chandler TY et al (1988) A three-part system for refining intraocular lens power calculations. J Cataract Refract Surg 14:17–24. https://doi.org/10.1016/s0886-3350(88)80059-2
Wang L, Koch DD (2018) Modified axial length adjustment formulas in long eyes. J Cataract Refract Surg 44:1396–1397. https://doi.org/10.1016/j.jcrs.2018.07.049
Wang L, Holladay JT, Koch DD (2018) Wang-Koch axial length adjustment for the Holladay 2 formula in long eyes. J Cataract Refract Surg 44:1291–1292; erratum (2019) 45:117. https://doi.org/10.1016/j.jcrs.2018.06.057, https://doi.org/10.1016/j.jcrs.2018.11.006.
Melles RB, Kane JX, Olsen T, Chang WJ (2019) Update on intraocular lens power calculation formulas. Ophthalmology 126:1334–1335. https://doi.org/10.1016/j.ophtha.2019.04.011
Retzlaff JA, Sanders DR, Kraff MC (1990) Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg 16:333–340; erratum (1990) 528. https://doi.org/10.1016/s0886-3350(13)80705-5.
Sheard RM, Smith GT, Cooke DL (2010) Improving the prediction accuracy of the SRK/T formula: the T2 formula. J Cataract Refract Surg 36:1829–1834. https://doi.org/10.1016/j.jcrs.2010.05.031
Voytsekhivskyy O (2018) Development and Clinical Accuracy of a New Intraocular Lens Power Formula (VRF) Compared to Other Formulas. Am J Ophthalmol 185:56–67. https://doi.org/10.1016/j.ajo.2017.10.020
Næser K, Savini G (2019) Accuracy of thick-lens intraocular lens power calculation based on cutting-card or calculated data for lens architecture. J Cataract Refract Surg 45:1422–1429. https://doi.org/10.1016/j.jcrs.2019.05.021
Hipólito-Fernandes D, Luís ME, Gil P et al (2020) VRF-G, a New Intraocular Lens Power Calculation Formula: A 13-Formulas Comparison Study. Clin Ophthalmol 14:4395–4402. https://doi.org/10.2147/OPTH.S290125
Wang L, Koch DD, Hill W, Abulafia A (2017) Pursuing perfection in intraocular lens calculations: III. Criteria for analyzing outcomes. J Cataract Refract Surg 43:999–1002. https://doi.org/10.1016/j.jcrs.2017.08.003
Simpson MJ, Charman WN (2014) The effect of testing distance on intraocular lens power calculation. J Refract Surg 30:726. https://doi.org/10.3928/1081597X-20141021-01
Savini G, Taroni L, Schiano-Lomoriello D, Hoffer KJ (2021) Repeatability of total Keratometry and standard Keratometry by the IOLMaster 700 and comparison to total corneal astigmatism by Scheimpflug imaging. Eye 35:307–315. https://doi.org/10.1038/s41433-020-01245-8
Cheng H, Li W, Kane JX et al (2021) Accuracy of artificial intelligence formulas and axial length adjustments for highly myopic eyes. Am J Ophthalmol 223:100–107. https://doi.org/10.1016/j.ajo.2020.09.019
Cheng H, Liu L, Sun A, Wu M (2020) Accuracy of modified axial length adjustment for intraocular lens power calculation in Chinese axial myopic eyes. Curr Eye Res 45:827–833. https://doi.org/10.1080/02713683.2019.1698053
Savini G, Hoffer KJ, Balducci N et al (2020) Comparison of formula accuracy for intraocular lens power calculation based on measurements by a swept-source optical coherence tomography optical biometer. J Cataract Refract Surg 46:27–33. https://doi.org/10.1016/j.jcrs.2019.08.044
Darcy K, Gunn D, Tavassoli S et al (2020) Assessment of the accuracy of new and updated intraocular lens power calculation formulas in 10 930 eyes from the UK National Health Service. J Cataract Refract Surg 46:2–7. https://doi.org/10.1016/j.jcrs.2019.08.014
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Larysa Tutchenko. The first draft of the manuscript was written by Oleksiy Voytsekhivskyy and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. Data collection for this retrospective study was approved by the Kyiv Clinical Ophthalmology Hospital Eye Microsurgery Center, Kyiv, Ukraine (IRB-CME-202021-E).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Dr. Voytsekhivskyy is the inventor and sole owner of the VRF and VRF-G formulas and has a patent on the method of estimation of postoperative lens position (ELP) and the calculation of optical power and is the author and copyright holder of a computer program VRF Suite V1.3.
Dr. Tutchenko declares no potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Voytsekhivskyy, O., Tutchenko, L. Comparison of the prediction accuracy of 13 formulas in long eyes. Graefes Arch Clin Exp Ophthalmol 261, 2575–2583 (2023). https://doi.org/10.1007/s00417-023-06060-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06060-x