Abstract
Purpose
This study is to quantitatively estimate the health-related quality of life (HRQOL) impact of major age-related eye diseases (AREDs) including cataract, glaucoma, age-related macular degeneration (AMD), and diabetic retinopathy (DR) assessed by the EuroQoL Five-Dimensional Questionnaire (EQ-5D).
Methods
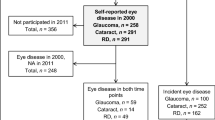
PubMed, Embase, Cochrane Library, and CINAHL were searched until October 20, 2022. Studies were included if they reported the EQ-5D health utility score (HUS) or visual analogue scale (VAS) score of both AREDs patients and healthy controls. The mean difference (MD) in HUS or VAS score between cases and controls and its 95% confidence interval (95%CI) were pooled using the random-effects model. We also performed sensitivity analysis using the leaving-one-out method and subgroup analyses by sample size and race. The prevalence in reporting any problems in the five EQ-5D dimensions was summarized and compared between cases and controls using the Chi-square test.
Results
Fifteen articles involving 30,491 participants were included in this review. Pooled estimates indicated reduced HUS in AMD patients (MD = – 0.04, 95%CI – 0.07, – 0.01; P = 0.009), DR patients (MD = – 0.03, 95%CI – 0.05, – 0.01; P = 0.01), and glaucoma patients (MD = – 0.06, 95%CI – 0.10, – 0.01; P = 0.01), compared with the controls. Significantly lower EQ-5D VAS score was also observed in cataract patients (MD = – 11.33, 95%CI – 13.47, – 9.18; P < 0.001) and DR patients (MD = – 6.41, 95%CI – 10.64, – 2.18; P = 0.003). AREDs patients reported usual activities and anxiety/depression problems more frequently than the control group.
Conclusions
Our findings confirmed the HRQOL impairment caused by major AREDs including AMD, cataract, DR, and glaucoma. High-quality studies with large sample sizes are warranted to further verify our results.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Gohdes DM, Balamurugan A, Larsen BA, Maylahn C (2005) Age-related eye diseases: an emerging challenge for public health professionals. Prev Chronic Dis 2:A17
Apm A, Jra B, Jc A, Tb C, Jhza D, Ij E, Mj F, An G, Hfh I, Ht J (2022) The economics of vision impairment and its leading causes: A systematic review. E Clin Med 46:101354
Abyu GY (2019) Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health 5(12):1221–34
Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J, Kempen JH, Leasher J, Limburg H, Naidoo K, Pesudovs K, Resnikoff S, Silvester A, Stevens GA, Tahhan N, Wong TY, Taylor HR (2017) Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 5:e888–e897. https://doi.org/10.1016/s2214-109x(17)30293-0
Brown RL, Barrett AE (2011) Visual impairment and quality of life among older adults: an examination of explanations for the relationship. J Gerontol: Ser B 66B:364–373. https://doi.org/10.1093/geronb/gbr015
Feeny D (2000) A utility approach to the assessment of health-related quality of life. Med Care 38:li151-4. https://doi.org/10.1097/00005650-200009002-00022
National Institute for H, Care E (2013) Guide to the Methods of Technology Appraisal 2013. London
Group EQ (1990) EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16.
Devlin NJ, Brooks R (2017) EQ-5D and the EuroQol Group: past, present and future. Appl Health Econ Health Policy 15:127–137. https://doi.org/10.1007/s40258-017-0310-5
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736
Buchholz I, Janssen MF, Kohlmann T, Feng YS (2018) A systematic review of studies comparing the measurement properties of the three-level and five-level versions of the EQ-5D. Pharmacoeconomics 36:645–661. https://doi.org/10.1007/s40273-018-0642-5
Haridoss M, Bagepally BS, Natarajan M (2021) Health-related quality of life in rheumatoid arthritis: systematic review and meta-analysis of EuroQol (EQ-5D) utility scores from Asia. Int J Rheum Dis 24:314–326. https://doi.org/10.1111/1756-185X.14066
Polack S, Kuper H, Mathenge W, Fletcher A, Foster A (2007) Cataract visual impairment and quality of life in a Kenyan population. Br J Ophthalmol 91:927–932. https://doi.org/10.1136/bjo.2006.110973
Coons SJ, Rao S, Keininger DL, Hays RD (2000) A comparative review of generic quality-of-life instruments. Pharmacoeconomics 17:13–35. https://doi.org/10.2165/00019053-200017010-00002
Soubrane G, Cruess A, Lotery A, Pauleikhoff D, Monès J, Xu X, Zlateva G, Buggage R, Conlon J, Goss TF (2007) Burden and health care resource utilization in neovascular age-related macular degeneration: findings of a multicountry study. Arch Ophthalmol (Chicago, III. : 1960) 125:1249–54. https://doi.org/10.1001/archopht.125.9.1249
Chatziralli I, Mitropoulos P, Parikakis E, Niakas D, Labiris G (2017) Risk factors for poor quality of life among patients with age-related macular degeneration. Semin Ophthalmol 32:772–780. https://doi.org/10.1080/08820538.2016.1181192
Lloyd A, Nafees B, Gavriel S, Rousculp MD, Boye KS, Ahmad A (2008) Health utility values associated with diabetic retinopathy. Diabet Med : J Bri Diabet Assoc 25:618–624. https://doi.org/10.1111/j.1464-5491.2008.02430.x
Ryu SJ, Lee WJ, Tarver LB, Shin YU, Kang MH, Seong M, Cho HY (2017) Depressive symptoms and quality of life in age-related macular degeneration based on Korea National Health and Nutrition Examination Survey (KNHANES). Korean J Ophthalmol : KJO 31:412–423. https://doi.org/10.3341/kjo.2016.0086
Rojananuangnit K, Sudjinda N (2021) Utility index and patient-reported outcome measures in glaucomatous patients comparing with normal participants. Clin Ophthalmol (Auckland, N Z.) 15:835–43. https://doi.org/10.2147/opth.S300226
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, Niu Y, Du L (2015) The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 8:2–10. https://doi.org/10.1111/jebm.12141
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Walters SJ, Brazier JE (2005) Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Res : An Int J Qual Life Aspects Treat, Care Rehabil 14:1523–1532. https://doi.org/10.1007/s11136-004-7713-0
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Meas Inconsistency Meta-Analyses BMJ (Clin Research Ed) 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Benavides-Varela S, ZandonellaCallegher C, Fagiolini B, Leo I, Altoè G, Lucangeli D (2020) Effectiveness of digital-based interventions for children with mathematical learning difficulties: a meta-analysis. Comput Educ 157:103953. https://doi.org/10.1016/j.compedu.2020.103953
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res Ed) 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Pan CW, Wang S, Wang P, Xu CL, Song E (2018) Diabetic retinopathy and health-related quality of life among Chinese with known type 2 diabetes mellitus. Qual Life Res : An Int J Qual Life Asp Treat, Care Rehabil 27:2087–2093. https://doi.org/10.1007/s11136-018-1876-6
Polack S, Alavi Y, RachapalleReddi S, Kulothungan V, Kuper H (2015) Utility values associated with diabetic retinopathy in Chennai, India. Ophthalmic Epidemiol 22:20–27. https://doi.org/10.3109/09286586.2014.885057
Javanbakht M, Abolhasani F, Mashayekhi A, Baradaran HR, Jahangirinoudeh Y (2012) Health related quality of life in patients with type 2 diabetes mellitus in Iran: a national survey. PloS one 7:e44526
Park S, Kho YL, Kim HJ, Kim J, Lee EH (2015) Impact of glaucoma on quality of life and activities of daily living. Hong Kong J Occup Ther 25:39–44. https://doi.org/10.1016/j.hkjot.2015.04.002
Sakamaki H, Ikeda S, Ikegami N, Uchigata Y, Iwamoto Y, Origasa H, Otani T, Otani Y (2006) Measurement of HRQL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value Health : J Int Soc Pharmacoeconomics Outcomes Res 9:47–53. https://doi.org/10.1111/j.1524-4733.2006.00080.x
Ben Â, de Souza CF, Locatelli F, Rosses APO, Szortika A, de Araujo AL, de Carvalho G, Lavinsky D, Neyeloff JL, Neumann CR (2021) Health-related quality of life associated with diabetic retinopathy in patients at a public primary care service in southern Brazil. Arch Endocrinol Metab 64:575–83. https://doi.org/10.20945/2359-3997000000223
Polack S, Kuper H, Wadud Z, Fletcher A, Foster A (2008) Quality of life and visual impairment from cataract in Satkhira district, Bangladesh. Br J Ophthalmol 92:1026–1030. https://doi.org/10.1136/bjo.2007.134791
Polack S, Eusebio C, Fletcher A, Foster A, Kuper H (2010) Visual impairment from cataract and health related quality of life: results from a case-control study in the Philippines. Ophthalmic Epidemiol 17:152–159. https://doi.org/10.3109/09286581003731536
Jung KI, Park CK (2016) Mental health status and quality of life in undiagnosed glaucoma patients: a nationwide population-based study. Med 95:e3523. https://doi.org/10.1097/md.0000000000003523
Sprangers MA (1996) Response-shift bias: a challenge to the assessment of patients’ quality of life in cancer clinical trials. Cancer Treat Rev 22:55–62. https://doi.org/10.1016/s0305-7372(96)90064-x
Funding
This study was funded by the National Natural Science Foundation of China (grant number 82122059).
Author information
Authors and Affiliations
Contributions
CWP and PW contributed substantially to the conception and design of this paper. JYK and YX conducted the literature searches and extracted the data from published papers. JYK, DLL, and MZ drafted the paper and carried out the statistical analysis. JYK and PW revised the article.
Corresponding authors
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kai, JY., Xu, Y., Li, DL. et al. Impact of major age-related eye disorders on health-related quality of life assessed by EQ-5D: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 261, 2455–2463 (2023). https://doi.org/10.1007/s00417-023-06034-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06034-z