Abstract
Purpose
This article is a scoping review of published and peer-reviewed articles using deep-learning (DL) applied to ultra-widefield (UWF) imaging. This study provides an overview of the published uses of DL and UWF imaging for the detection of ophthalmic and systemic diseases, generative image synthesis, quality assessment of images, and segmentation and localization of ophthalmic image features.
Methods
A literature search was performed up to August 31st, 2021 using PubMed, Embase, Cochrane Library, and Google Scholar. The inclusion criteria were as follows: (1) deep learning, (2) ultra-widefield imaging. The exclusion criteria were as follows: (1) articles published in any language other than English, (2) articles not peer-reviewed (usually preprints), (3) no full-text availability, (4) articles using machine learning algorithms other than deep learning. No study design was excluded from consideration.
Results
A total of 36 studies were included. Twenty-three studies discussed ophthalmic disease detection and classification, 5 discussed segmentation and localization of ultra-widefield images (UWFIs), 3 discussed generative image synthesis, 3 discussed ophthalmic image quality assessment, and 2 discussed detecting systemic diseases via UWF imaging.
Conclusion
The application of DL to UWF imaging has demonstrated significant effectiveness in the diagnosis and detection of ophthalmic diseases including diabetic retinopathy, retinal detachment, and glaucoma. DL has also been applied in the generation of synthetic ophthalmic images. This scoping review highlights and discusses the current uses of DL with UWF imaging, and the future of DL applications in this field.




Similar content being viewed by others
Abbreviations
- 7SF:
-
7 Standard Field
- AMD:
-
Age-related macular degeneration
- AD:
-
Alzheimer’s Disease
- AUROC:
-
Area under ROC
- AUPRC:
-
Area under precision-recall
- ANN:
-
Artificial neural network
- AutoML:
-
Automated machine learning
- BCVA:
-
Best corrected visual acuity
- baPWV :
-
Brachial-Ankle Pulse-Wave Velocity
- BRVO :
-
Branch RVO
- CRVO:
-
Central RVO
- CNNs:
-
Convolutional neural networks
- DL:
-
Deep learning
- DNN:
-
Deep neural network
- DME:
-
Diabetic macular edema
- DR:
-
Diabetic retinopathy
- FA:
-
Fluorescein angiography
- FI:
-
Fundus image
- GC-IPL:
-
Ganglion cell-inner plexiform layer
- GANs:
-
Generative adversarial networks
- GON :
-
Glaucomatous optic neuropathy
- Grad-CAM:
-
Gradient-weighted class activation mapping
- HITL :
-
Human-in-the-loop
- IMH:
-
Idiopathic macular hole
- ML:
-
Machine learning
- MAE :
-
Mean absolute error
- MAPE:
-
Mean-absolute-percent error
- NPDR:
-
Non-proliferative DR
- NPRLs:
-
Notable peripheral retinal lesions
- OCTA:
-
OCT angiography
- OCT:
-
Optical coherence tomography
- PDR:
-
Proliferative diabetic retinopathy
- PSR:
-
Proliferative sickle cell retinopathy
- ROC:
-
Receiver operating characteristic
- RDR:
-
Referrable DR
- ROI:
-
Region of interest
- RD:
-
Retinal detachment
- RED:
-
Retinal exudates And/Or Drusen
- RH:
-
Retinal hemorrhage
- RVO:
-
Retinal vein occlusion
- RVA:
-
Retinal vessel areas
- RP:
-
Retinitis pigmentosa
- RMSE :
-
Root-mean-square error
- SLO:
-
Scanning laser ophthalmoscope
- SCR:
-
Sickle cell retinopathy
- SSIM:
-
Structural similarity
- UWF:
-
Ultra-widefield
- UWF-FA:
-
Ultra-widefield fluorescein angiography
- UWFI:
-
Ultra-widefield image
- UWF-FAF:
-
UWF fundus autofluorescence
- UWF-ICGA:
-
UWF indocyanine green angiography
- VTDR:
-
Vision-threatening DR
- VA:
-
Visual acuity
- WF:
-
Widefield
- WFIs:
-
Widefield images
References
Agarwal A (2007) Fundus Fluorescein and Indocyanine Green Angiography: A Textbook and Atlas, 1st edn. Slack Incorporated, Thorofare, NJ
(1981) Diabetic retinopathy study. Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy. Prepared by the Diabetic Retinopathy. Invest Ophthalmol Vis Sci 21:1–226
Kumar V, Surve A, Kumawat D et al (2021) Ultra-wide field retinal imaging: a wider clinical perspective. Indian J Ophthalmol 69:824–835. https://doi.org/10.4103/ijo.IJO_1403_20
Choudhry N, Duker JS, Freund KB et al (2019) Classification and guidelines for widefield imaging. Ophthalmology Retina 3:843–849. https://doi.org/10.1016/j.oret.2019.05.007
Kaines A, Oliver S, Reddy S, Schwartz SD (2009) Ultrawide angle angiography for the detection and management of diabetic retinopathy. Int Ophthalmol Clin 49:53–59. https://doi.org/10.1097/IIO.0b013e31819fd471
Nagiel A, Lalane RA, Sadda SR, Schwartz SD (2016) Ultra-widefield fundus imaging: a review of clinical applications and future trends. Retina 36:660–678. https://doi.org/10.1097/IAE.0000000000000937
Witmer MT, Kiss S (2012) The clinical utility of ultra-wide-field imaging. In: Review of ophthalmology. https://www.reviewofophthalmology.com/article/the-clinical-utility-of-ultra-wide-field-imaging. Accessed 1 Oct 2021
Optos Inc. (2021) Optos.com - Optos products. In: Optos Products. https://www.optos.com/products/. Accessed 21 Aug 2021
Zeiss Inc. CLARUS 500. In: Clarus 500 Product Information. https://www.zeiss.com/meditec/int/product-portfolio/retinal-cameras/clarus-500.html. Accessed 23 Apr 2022
Wessel MM, Aaker GD, Parlitsis G et al (2012) Ultra–wide-field angiography improves the detection and classification of diabetic retinopathy. Retina 32:785–791. https://doi.org/10.1097/IAE.0b013e3182278b64
Antaki F, Coussa RG, Mikhail M et al (2020) The prognostic value of peripheral retinal nonperfusion in diabetic retinopathy using ultra-widefield fluorescein angiography. Graefe’s Arch Clin Exp ogy 258:2681–2690
Liu TA, Arevalo JF (2019) Wide-field imaging in proliferative diabetic retinopathy. Int J Retin Vitreous 5:1–4
Fogliato G, Borrelli E, Iuliano L et al (2019) Comparison between ultra-widefield pseudocolor imaging and indirect ophthalmoscopy in the detection of peripheral retinal lesions. Ophthalmic Surg Lasers Imaging Retina 50:544–549. https://doi.org/10.3928/23258160-20190905-02
Quinn NB, Azuara-Blanco A, Graham K et al (2018) Can ultra-wide field retinal imaging replace colour digital stereoscopy for glaucoma detection? Ophthalmic Epidemiol 25:63–69. https://doi.org/10.1080/09286586.2017.1351998
Forshaw TRJ, Minör ÅS, Subhi Y, Sørensen TL (2019) Peripheral retinal lesions in eyes with age-related macular degeneration using ultra-widefield imaging: a systematic review with meta-analyses. Ophthalmol Retin 3:734–743. https://doi.org/10.1016/j.oret.2019.04.014
Sadda S (2019) Wide-field imaging in retina and vitreous diseases. In: International Journal of Retina and Vitreous
El Naqa I, Murphy MJ (2015) What Is Machine Learning? In: El Naqa I, Li R, Murphy MJ (eds) Machine learning in radiation oncology: theory and applications. Springer International Publishing, Cham, pp 3–11
Sathya R, Abraham A (2013) Comparison of supervised and unsupervised learning algorithms for pattern classification. International Journal of Advanced Research in Artificial Intelligence 2:34–38
Deng L (2014) Deep Learning: Methods and Applications. FNT in Signal Process 7:197–387. https://doi.org/10.1561/2000000039
Russell S, Norvig P (2020) Artificial intelligence: a modern approach, 4th edn. Pearson, Hoboken
Zhou X, Belkin M (2014) Chapter 22 - Semi-Supervised Learning. In: Diniz PSR, Suykens JAK, Chellappa R, Theodoridis S (eds) Academic Press Library in Signal Processing. Elsevier, pp 1239–1269
Hinton G (1999) Unsupervised learning: foundations of neural computation, 1st edn. Bradford Books, Cambridge, Mass
Monarch R (2021) Human-in-the-loop machine learning: active learning and annotation for human-centered AI. Manning
Dongare AD, Kharde RR, Kachare AD (2012) Introduction to artificial neural network. Int J Eng Innov Technol (IJEIT) 2:189–194
Zhou V (2019) Machine learning for beginners: an introduction to neural networks. In: Medium. https://towardsdatascience.com/machine-learning-for-beginners-an-introduction-to-neural-networks-d49f22d238f9. Accessed 21 Aug 2021
Fornito A, Zalesky A, Bullmore ET (2016) Chapter 2 - Nodes and Edges. Fundamentals of brain network analysis. Academic Press, San Diego, pp 37–88
Ciresan DC, Meier U, Masci J et al (2011) Flexible, high performance convolutional neural networks for image classification. Proc Twenty-Second Int Joint Conf Artif Intell 2:1237–1242
Saha S (2018) A comprehensive guide to convolutional neural networks — the ELI5 way. In: Medium. https://towardsdatascience.com/a-comprehensive-guide-to-convolutional-neural-networks-the-eli5-way-3bd2b1164a53. Accessed 21 Aug 2021
LeCun Y, Boser B, Denker JS et al (1989) Backpropagation applied to handwritten zip code recognition. Neural Comput 1:541–551. https://doi.org/10.1162/neco.1989.1.4.541
Krizhevsky A, Sutskever I, Hinton GE (2012) ImageNet Classification with Deep Convolutional Neural Networks. In: Pereira F, Burges CJ, Bottou L, Weinberger KQ (eds) Advances in Neural Information Processing Systems. Curran Associates Inc
Alippi C, Disabato S, Roveri M (2018) Moving convolutional neural networks to embedded systems: the alexnet and VGG-16 Case. In: 2018 17th ACM/IEEE International Conference on Information Processing in Sensor Networks (IPSN), pp 212–223
MathWorks Pretrained Inception-ResNet-v2 convolutional neural network - MATLAB inceptionresnetv2. In: MATLAB Mathworks. https://www.mathworks.com/help/deeplearning/ref/inceptionresnetv2.html;jsessionid=ae4b2abd60579ecab16f783b4f26. Accessed 21 Aug 2021
Waring J, Lindvall C, Umeton R (2020) Automated machine learning: review of the state-of-the-art and opportunities for healthcare. Artif Intell Med 104:101822. https://doi.org/10.1016/j.artmed.2020.101822
Faes L, Wagner SK, Fu DJ et al (2019) Automated deep learning design for medical image classification by health-care professionals with no coding experience: a feasibility study. The Lancet Digital Health 1:e232–e242. https://doi.org/10.1016/S2589-7500(19)30108-6
Korot E, Guan Z, Ferraz D et al (2021) Code-free deep learning for multi-modality medical image classification. Nat Mach Intell 3:288–298. https://doi.org/10.1038/s42256-021-00305-2
Alphabet Inc. Cloud automl custom machine learning models. In: Googlel cloud. https://cloud.google.com/automl. Accessed 5 May 2022
Touma S, Antaki F, Duval R (2022) Development of a code-free machine learning model for the classification of cataract surgery phases. Sci Rep 12:2398. https://doi.org/10.1038/s41598-022-06127-5
Antaki F, Coussa RG, Hammamji K, Duval R (2021) Revisiting the problem of optic nerve detection in a retinal image using automated machine learning. Asia Pac J Ophthalmol (Phila) 10:335–336. https://doi.org/10.1097/APO.0000000000000398
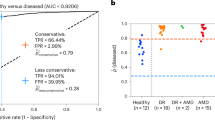
Antaki F, Coussa RG, Kahwati G et al (2021) Accuracy of automated machine learning in classifying retinal pathologies from ultra-widefield pseudocolour fundus images. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319030
Antaki F, Kahwati G, Sebag J et al (2020) Predictive modeling of proliferative vitreoretinopathy using automated machine learning by ophthalmologists without coding experience. Sci Rep 10:19528. https://doi.org/10.1038/s41598-020-76665-3
Shah T (2020) About train, validation and test sets in machine learning. In: Medium. https://towardsdatascience.com/train-validation-and-test-sets-72cb40cba9e7. Accessed 21 Aug 2021
Talebi H, Milanfar P (2021) Learning to resize images for computer vision tasks. CoRR abs/2103.09950
Calderon-Auza G, Perez A, Nakano-Miyatake M et al (2019) CNN-based quality assessment for retinal image captured by wide field of view non-mydriatic fundus camera. 2019 42nd International Conference on Telecommunications and Signal Processing (TSP) 282–285
Perez L, Wang J (2017) The effectiveness of data augmentation in image classification using deep learning
Nagasawa T, Tabuchi H, Masumoto H et al (2018) Accuracy of deep learning, a machine learning technology, using ultra-wide-field fundus ophthalmoscopy for detecting idiopathic macular holes. PeerJ 6:e5696. https://doi.org/10.7717/peerj.5696
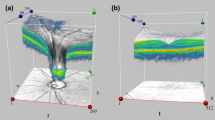
Li Z, Guo C, Nie D et al (2020) Deep learning for detecting retinal detachment and discerning macular status using ultra-widefield fundus images. Commun Biol 3:15. https://doi.org/10.1038/s42003-019-0730-x
Parikh R, Mathai A, Parikh S et al (2008) Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol 56:45–50
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5:1315–1316. https://doi.org/10.1097/JTO.0b013e3181ec173d
Boyd K, Eng KH, Page CD (2013) Area under the precision-recall curve: point estimates and confidence intervals. In: Blockeel H, Kersting K, Nijssen S, Železný F (eds) Machine Learning and Knowledge Discovery in Databases. Springer, Berlin, Heidelberg, pp 451–466
Zou KH, Warfield SK, Bharatha A et al (2004) Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol 11:178–189. https://doi.org/10.1016/S1076-6332(03)00671-8
Wang Z, Keane PA, Chiang M et al (2021) Artificial intelligence and deep learning in ophthalmology. In: Lidströmer N, Ashrafian H (eds) Artificial Intelligence in Medicine. Springer International Publishing, Cham, pp 1–34
Bawany MH, Ding L, Ramchandran RS et al (2020) Automated vessel density detection in fluorescein angiography images correlates with vision in proliferative diabetic retinopathy. PLoS ONE 15:e0238958. https://doi.org/10.1371/journal.pone.0238958
Oh K, Kang HM, Leem D et al (2021) Early detection of diabetic retinopathy based on deep learning and ultra-wide-field fundus images. Sci Rep 11:1897. https://doi.org/10.1038/s41598-021-81539-3
Tang F, Luenam P, Ran AR, et al (2021) Detection of diabetic retinopathy from ultra-wide field scanning laser ophthalmoscope images: a multi-center deep-learning analysis. Ophthalmology Retina S246865302100035X.https://doi.org/10.1016/j.oret.2021.01.013
Wang K, Jayadev C, Nittala MG et al (2018) Automated detection of diabetic retinopathy lesions on ultrawidefield pseudocolour images. Acta Ophthalmol 96:e168–e173. https://doi.org/10.1111/aos.13528
Nagasawa T, Tabuchi H, Masumoto H et al (2019) Accuracy of ultrawide-field fundus ophthalmoscopy-assisted deep learning for detecting treatment-naïve proliferative diabetic retinopathy. Int Ophthalmol 39:2153–2159. https://doi.org/10.1007/s10792-019-01074-z
Nagasawa T, Tabuchi H, Masumoto H et al (2021) Accuracy of diabetic retinopathy staging with a deep convolutional neural network using ultra-wide-field fundus ophthalmoscopy and optical coherence tomography angiography. J Ophthalmol 2021:6651175. https://doi.org/10.1155/2021/6651175
Ding L, Bawany MH, Kuriyan AE et al (2020) A novel deep learning pipeline for retinal vessel detection in fluorescein angiography. IEEE Trans Image Process 29:6561–6573. https://doi.org/10.1109/TIP.2020.2991530
Orlando JI, Fu H, Barbosa Breda J et al (2020) REFUGE Challenge: A unified framework for evaluating automated methods for glaucoma assessment from fundus photographs. Med Image Anal 59:101570. https://doi.org/10.1016/j.media.2019.101570
Ohsugi H, Tabuchi H, Enno H, Ishitobi N (2017) Accuracy of deep learning, a machine-learning technology, using ultra-wide-field fundus ophthalmoscopy for detecting rhegmatogenous retinal detachment. Sci Rep 7:9425. https://doi.org/10.1038/s41598-017-09891-x
Li Z, Guo C, Nie D et al (2019) A deep learning system for identifying lattice degeneration and retinal breaks using ultra-widefield fundus images. Annals of Translational Medicine 7:618–618. https://doi.org/10.21037/atm.2019.11.28
Zhang C, He F, Li B et al (2021) Development of a deep-learning system for detection of lattice degeneration, retinal breaks, and retinal detachment in tessellated eyes using ultra-wide-field fundus images: a pilot study. Graefes Arch Clin Exp Ophthalmol. https://doi.org/10.1007/s00417-021-05105-3
Li Z, Guo C, Lin D et al (2021) Deep learning for automated glaucomatous optic neuropathy detection from ultra-widefield fundus images. Br J Ophthalmol 105:1548–1554. https://doi.org/10.1136/bjophthalmol-2020-317327
Masumoto H, Tabuchi H, Nakakura S et al (2018) Deep-learning classifier with an ultrawide-field scanning laser ophthalmoscope detects glaucoma visual field severity. J Glaucoma 27:647–652. https://doi.org/10.1097/IJG.0000000000000988
Ran AR, Tham CC, Chan PP et al (2021) Deep learning in glaucoma with optical coherence tomography: a review. Eye 35:188–201. https://doi.org/10.1038/s41433-020-01191-5
Maetschke S, Antony B, Ishikawa H et al (2019) A feature agnostic approach for glaucoma detection in OCT volumes. PLoS ONE 14:e0219126. https://doi.org/10.1371/journal.pone.0219126
Matsuba S, Tabuchi H, Ohsugi H et al (2019) Accuracy of ultra-wide-field fundus ophthalmoscopy-assisted deep learning, a machine-learning technology, for detecting age-related macular degeneration. Int Ophthalmol 39:1269–1275. https://doi.org/10.1007/s10792-018-0940-0
Li Z, Guo C, Nie D et al (2021) Automated detection of retinal exudates and drusen in ultra-widefield fundus images based on deep learning. Eye 1–6. https://doi.org/10.1038/s41433-021-01715-7
Masumoto H, Tabuchi H, Nakakura S et al (2019) Accuracy of a deep convolutional neural network in detection of retinitis pigmentosa on ultrawide-field images. PeerJ 7:e6900. https://doi.org/10.7717/peerj.6900
Kim IK, Lee K, Park JH et al (2021) Classification of pachychoroid disease on ultrawide-field indocyanine green angiography using auto-machine learning platform. Br J Ophthalmol 105:856–861. https://doi.org/10.1136/bjophthalmol-2020-316108
Nagasato D, Tabuchi H, Ohsugi H et al (2018) Deep neural network-based method for detecting central retinal vein occlusion using ultrawide-field fundus ophthalmoscopy. Journal of Ophthalmology 2018:1–6. https://doi.org/10.1155/2018/1875431
Nagasato D, Tabuchi H, Ohsugi H et al (2019) Deep-learning classifier with ultrawide-field fundus ophthalmoscopy for detecting branch retinal vein occlusion. Int J Ophthalmol 12:94–99. https://doi.org/10.18240/ijo.2019.01.15
Shi Z, Wang T, Huang Z et al (2021) A method for the automatic detection of myopia in Optos fundus images based on deep learning. Int J Numer Methods Biomed Eng 37:e3460. https://doi.org/10.1002/cnm.3460
Li Z, Guo C, Nie D et al (2020) Development and evaluation of a deep learning system for screening retinal hemorrhage based on ultra-widefield fundus images. Transl Vision Sci Technol 9:3. https://doi.org/10.1167/tvst.9.2.3
Dai L, Wu L, Li H et al (2021) A deep learning system for detecting diabetic retinopathy across the disease spectrum. Nat Commun 12:3242. https://doi.org/10.1038/s41467-021-23458-5
Calderon-Auza G, Carrillo-Gomez C, Nakano M et al (2020) A teleophthalmology support system based on the visibility of retinal elements using the CNNs. Sensors 20:2838. https://doi.org/10.3390/s20102838
Li HH, Abraham JR, Sevgi DD et al (2020) Automated quality assessment and image selection of ultra-widefield fluorescein angiography images through deep learning. Trans Vis Sci Tech 9:52–52. https://doi.org/10.1167/tvst.9.2.52
Li Z, Guo C, Nie D et al (2020) Deep learning from “passive feeding” to “selective eating” of real-world data. NPJ Digit Med 3:143. https://doi.org/10.1038/s41746-020-00350-y
Ding L, Kuriyan AE, Ramchandran RS et al (2021) Weakly-supervised vessel detection in ultra-widefield fundus photography via iterative multi-modal registration and learning. IEEE Trans Med Imaging 40:2748–2758. https://doi.org/10.1109/TMI.2020.3027665
do Nunez Rio JM, Sen P, Rasheed R et al (2020) Deep learning-based segmentation and quantification of retinal capillary non-perfusion on ultra-wide-field retinal fluorescein angiography. J Clin Med 9:2537. https://doi.org/10.3390/jcm9082537
Wang Z, Jiang X, Liu J et al (2020) Multi-task siamese network for retinal artery/vein separation via deep convolution along vessel. IEEE Trans Med Imaging 39:2904–2919. https://doi.org/10.1109/TMI.2020.2980117
Sevgi DD, Srivastava SK, Wykoff C et al (2021) Deep learning-enabled ultra-widefield retinal vessel segmentation with an automated quality-optimized angiographic phase selection tool. Eye (Lond). https://doi.org/10.1038/s41433-021-01661-4
Niemeijer M, Xu X, Dumitrescu AV et al (2011) Automated measurement of the arteriolar-to-venular width ratio in digital color fundus photographs. IEEE Trans Med Imaging 30:1941–1950
Staal J, Abràmoff MD, Niemeijer M et al (2004) Ridge-based vessel segmentation in color images of the retina. IEEE Trans Med Imaging 23:501–509
Estrada R, Tomasi C, Schmidler SC, Farsiu S (2014) Tree topology estimation. IEEE Trans Pattern Anal Mach Intell 37:1688–1701
Ju L, Wang X, Zhou Q et al (2020) Bridge the domain gap between ultra-wide-field and traditional fundus images via adversarial domain adaptation. https://doi.org/10.48550/ARXIV.2003.10042
Ju L, Wang X, Zhao X et al (2021) Leveraging regular fundus images for training UWF fundus diagnosis models via adversarial learning and pseudo-labeling. IEEE Trans Med Imaging 40:2911–2925. https://doi.org/10.1109/TMI.2021.3056395
Xie H, Lei H, Zeng X et al (2020) AMD-GAN: Attention encoder and multi-branch structure based generative adversarial networks for fundus disease detection from scanning laser ophthalmoscopy images. Neural Netw 132:477–490. https://doi.org/10.1016/j.neunet.2020.09.005
Yoo TK, Ryu IH, Kim JK et al (2020) Deep learning can generate traditional retinal fundus photographs using ultra-widefield images via generative adversarial networks. Comput Methods Programs Biomed 197:105761. https://doi.org/10.1016/j.cmpb.2020.105761
Goodfellow I, Pouget-Abadie J, Mirza M et al (2014) Generative adversarial nets. In: Ghahramani Z, Welling M, Cortes C (eds) Advances in neural information processing systems. Curran Associates, Inc.
Karpathy A, Abbeel P, Brockman G et al (2016) Generative models. In: OpenAI. https://openai.com/blog/generative-models/. Accessed 18 Aug 2021
NVIDIA Research Projects (2021) StyleGAN - official tensorflow implementation. NVIDIA Research Projects
Nagasato D, Tabuchi H, Masumoto H et al (2020) Prediction of age and brachial-ankle pulse-wave velocity using ultra-wide-field pseudo-color images by deep learning. Scientific Reports 10:19369. https://doi.org/10.1038/s41598-020-76513-4
Wisely CE, Wang D, Henao R et al (2022) Convolutional neural network to identify symptomatic Alzheimer’s disease using multimodal retinal imaging. Br J Ophthalmol 106:388–395. https://doi.org/10.1136/bjophthalmol-2020-317659
Parikh RB, Teeple S, Navathe AS (2019) Addressing bias in artificial intelligence in health care. JAMA 322:2377–2378. https://doi.org/10.1001/jama.2019.18058
Selvaraju RR, Cogswell M, Das A et al (2020) Grad-CAM: visual explanations from deep networks via gradient-based localization. Int J Comput Vis 128:336–359. https://doi.org/10.1007/s11263-019-01228-7
Hanif AM, Beqiri S, Keane PA, Campbell JP (2021) Applications of interpretability in deep learning models for ophthalmology. Curr Opin Ophthalmol 32:452–458. https://doi.org/10.1097/ICU.0000000000000780
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants performed by any of the authors. As this is a review of previously published articles, no ethical or IRB approval was required.
Conflict of interest
Fares Antaki reports research funding from Bayer and honoraria from Snell Medical Communication. Renaud Duval reports speaker honoraria from Bayer, Roche, Novartis and Alcon, a research grant and an unrestricted education grant from Bayer, and equity ownership in Optina Diagnostics. Nishaant Bhambra, Farida El-Malt, and AnQi Xu declare that they have no conflicts of interest.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bhambra, N., Antaki, F., Malt, F.E. et al. Deep learning for ultra-widefield imaging: a scoping review. Graefes Arch Clin Exp Ophthalmol 260, 3737–3778 (2022). https://doi.org/10.1007/s00417-022-05741-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05741-3