Abstract
Purpose
Superior limbic keratoconjunctivitis (SLK) is an uncommon and often overlooked chronic ocular surface disease. This retrospective consecutive case series study on Chinese patients aimed to characterize the features of this disease, including those undescribed in previous literature.
Methods
Two hundred thirty-six patients diagnosed with SLK were enrolled into this consecutive case study from 2016 to 2019. The demographics, symptoms, Ocular Surface Disease Index, and ocular signs were collected and analyzed. A scoring system (SLK scale index, SSI) that integrated five major sign scores was applied to evaluate SLK severity.
Results
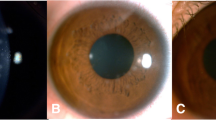
Of the 236 SLK patients, dryness was the most common complaint (59.3%). Of 459 SLK eyes, superior limbus/conjunctival staining (SCS) was present in 98% eyes, followed by the superior tarsal conjunctival alterations (85.2%) and superior bulbar conjunctiva hyperemia (80.8%). Approximately 63% of eyes were accompanied by corneal staining. Superior bulbar conjunctivochalasis was a relatively rare sign (41.6%). Among the five major signs, only the prevalence of SCS gradually increased with its severity. In addition, fluorescein staining at the inferior limbus and adjacent conjunctiva (ICS) was found positive in 163 eyes of 84 patients (36%) who had significantly higher SSI than those without ICS (p = 0.013).
Conclusions
We found that SCS is the most common out of the 5 typical signs of SLK. ICS, a new sign, occurred in one-third of patients. SCS, a simple marker of SLK, as well as SSI, an integrated evaluation system, had the advantage of evaluating the severity and objectively characterizing SLK in clinical practice.
Similar content being viewed by others
Data availability
All data and materials support our published claims and comply with field standards.
Code availability
Not applicable.
Abbreviations
- SLK:
-
Superior limbic keratoconjunctivitis
- SCS:
-
Conjunctival staining at the superior conjunctiva and limbus
- SCH:
-
Superior bulbar conjunctiva hyperemia
- SBC:
-
Superior bulbar conjunctivochalasis
- CS:
-
Cornea staining
- TCP:
-
Papillary hypertrophy and hyperemia of the superior tarsal conjunctiva
- ICS:
-
Fluorescein staining at the inferior limbus and adjacent conjunctiva
- SSI:
-
SLK scale index
- OSDI:
-
Ocular Surface Disease Index©
- BCVA:
-
Best-corrected visual acuity
- IOP:
-
Intraocular pressure
- logMAR:
-
Logarithm of minimal angle of resolution
- TBUT:
-
Tear break-up time
References
Braley AE, Alexander RC (1953) Superficial punctate keratitis; isolation of a virus. AMA Arch Ophthalmol 50(2):147–154
Thygeson P (1969) Observations on conjunctival neoplasms masquerading as chronic conjunctivitis or keratitis. Trans Am Acad Ophthalmol Otolaryngol 73(5):969–978
Theodore FH, Ferry AP (1970) Superior limbic keratoconjunctivitis. Clinical and pathological correlations. Arch Ophthalmol 84(4):481–484
Lahoti S, Weiss M, Johnson D, Kheirkhah A (2021) Superior limbic keratoconjunctivitis: a comprehensive review. Surv Ophthalmol. https://doi.org/10.1016/j.survophthal.2021.05.009
Yokoi N, Komuro A, Maruyama K, Tsuzuki M, Miyajima S, Kinoshita S (2003) New surgical treatment for superior limbic keratoconjunctivitis and its association with conjunctivochalasis. Am J Ophthalmol 135(3):303–308. https://doi.org/10.1016/s0002-9394(02)01975-x
Kurita J, Shoji J, Inada N, Yoneda T, Sumi T, Kobayashi M, Hoshikawa Y, Fukushima A, Yamagami S (2018) Clinical severity classification using automated conjunctival hyperemia analysis software in patients with superior limbic keratoconjunctivitis. Curr Eye Res 43(6):679–682. https://doi.org/10.1080/02713683.2017.1419573
Rodriguez-Garcia A, Macias-Rodriguez Y, Gonzalez-Gonzalez JM (2017) Efficacy and safety of 0.1% lodoxamide for the long-term treatment of superior limbic keratoconjunctivitis. Int Ophthalmol 38(3):1243–1249. https://doi.org/10.1007/s10792-017-0588-1
Kadrmas EF, Bartley GB (1995) Superior limbic keratoconjunctivitis. A prognostic sign for severe Graves ophthalmopathy. Ophthalmology 102(10):1472–1475
Cher I (2000) Superior limbic keratoconjunctivitis: multifactorial mechanical pathogenesis. Clin Experiment Ophthalmol 28(3):181–184
Eiferman RA, Wilkins EL (1979) Immunological aspects of superior limbic keratoconjunctivitis. Can J Ophthalmol J canadien d’ophtalmologie 14(2):85–87
Sun YC, Hsiao CH, Chen WL, Wang IJ, Hou YC, Hu FR (2008) Conjunctival resection combined with tenon layer excision and the involvement of mast cells in superior limbic keratoconjunctivitis. Am J Ophthalmol 145(3):445–452. https://doi.org/10.1016/j.ajo.2007.10.025
Goto E, Shimmura S, Shimazaki J, Tsubota K (2001) Treatment of superior limbic keratoconjunctivitis by application of autologous serum. Cornea 20(8):807–810
Ohashi Y, Watanabe H, Kinoshita S, Hosotani H, Umemoto M, Manabe R (1988) Vitamin A eyedrops for superior limbic keratoconjunctivitis. Am J Ophthalmol 105(5):523–527
Kheirkhah A, Casas V, Esquenazi S, Blanco G, Li W, Raju V, Tseng S (2007) New surgical approach for superior conjunctivochalasis. Cornea 26(6):685–691. https://doi.org/10.1097/ICO.0b013e31805771c6
Sivaraman K, Jivrajka R, Soin K, Bouchard C, Movahedan A, Shorter E, Jain S, Jacobs D, Djalilian A (2016) Superior limbic keratoconjunctivitis-like inflammation in patients with chronic graft-versus-host disease. Ocul Surf 14(3):393–400. https://doi.org/10.1016/j.jtos.2016.04.003
Özcura F, Aydin S, Helvaci M (2007) Ocular surface disease index for the diagnosis of dry eye syndrome. Ocul Immunol Inflamm 15:389–393. https://doi.org/10.1080/09273940701486803
Balci O (2014) Clinical characteristics of patients with conjunctivochalasis. Clinical ophthalmology (Auckland, NZ) 8:1655–1660. https://doi.org/10.2147/opth.s61851
Sun Y, Tang Y, Liou H, Chen W, Hu F (2020) Tear cytokine profiling in patients with superior limbic keratoconjunctivitis who underwent medical treatment or in conjunction with surgical management. Br J Ophthalmol 104(5):735–740. https://doi.org/10.1136/bjophthalmol-2018-313358
Terry R, Schnider C, Holden B, Cornish R, Grant T, Sweeney D, La Hood D, Back A (1993) CCLRU standards for success of daily and extended wear contact lenses. Optometry Vision Sci 70(3):234–243. https://doi.org/10.1097/00006324-199303000-00011
Efron N (1998) Grading scales for contact lens complications. Ophthalmic Physiol Opt 18(2):182–186. https://doi.org/10.1016/s0275-5408(97)00066-5
Mimura T, Mori M, Obata H, Usui T, Yamagami S, Funatsu H, Noma H, Amano S (2012) Conjunctivochalasis: associations with pinguecula in a hospital-based study. Acta Ophthalmol 90(8):773–782. https://doi.org/10.1111/j.1755-3768.2011.02161.x
Efron N, Morgan P, Katsara S (2001) Validation of grading scales for contact lens complications. Ophthalmic Physiol Opt 21(1):17–29. https://doi.org/10.1046/j.1475-1313.2001.00575.x
Huntjens B, Basi M, Nagra M (2020) Evaluating a new objective grading software for conjunctival hyperaemia. Contact Lens Anterior Eye 43(2):137–143. https://doi.org/10.1016/j.clae.2019.07.003
Efron N, Pritchard N, Brandon K, Copeland J, Godfrey R, Hamlyn B, Vrbancic V (2011) A survey of the use of grading scales for contact lens complications in optometric practice. Clin Exp Optom 94(2):193–199. https://doi.org/10.1111/j.1444-0938.2010.00549.x
Fagehi R (2018) Impact of environmental adaptation on tear film assessments. J Fr Ophtalmol 41(3):231–237. https://doi.org/10.1016/j.jfo.2017.08.021
Tsubota K, Yokoi N, Shimazaki J, Watanabe H, Dogru M, Yamada M, Kinoshita S, Kim HM, Tchah HW, Hyon JY, Yoon KC, Seo KY, Sun X, Chen W, Liang L, Li M, Liu Z (2017) New perspectives on dry eye definition and diagnosis: a consensus report by the Asia Dry Eye Society. Ocul Surf 15(1):65–76. https://doi.org/10.1016/j.jtos.2016.09.003
Zoroquiain P, Sanft DM, Esposito E, Cheema D, Dias AB, Burnier MN Jr (2018) High inflammatory infiltrate correlates with poor symptomatic improvement after surgical treatment for superior limbic keratoconjunctivitis. Cornea 37(4):495–500. https://doi.org/10.1097/ico.0000000000001508
Cher I (1969) Clinical features of superior limbic keroconjunctivitis in Australia. A probable association withhyrotoxicosis. Arch Ophthalmol 82(5):580–586
Kabat AG (1998) Lacrimal occlusion therapy for the treatment of superior limbic keratoconjunctivitis. Optometry Vision Sci 75(10):714–718
Mendoza-Adam G, Rodríguez-García A (2013) Superior limbic keratoconjunctivitis (SLK) and its association to systemic diseases. Revista Mexicana De Oftalmologia 87(2):93–99
Nelson JD (1989) Superior limbic keratoconjunctivitis (SLK). Eye (Lond) 3(Pt 2):180–189. https://doi.org/10.1038/eye.1989.26
Miller KL, Walt JG, Mink DR, Satram-Hoang S, Wilson SE, Perry HD, Asbell PA, Pflugfelder SC (2010) Minimal clinically important difference for the Ocular Surface Disease Index. Arch Ophthalmol 128(1):94–101. https://doi.org/10.1001/archophthalmol.2009.356
Funding
This work was supported by grants from the Guangzhou Science Technology and Innovation Commission (201607020011) and the National Natural Science Foundation of China (81770896, 81970848).
Author information
Authors and Affiliations
Contributions
Conceptualization: Kaili Wu, Chao Cheng, Minyi Zhu; methodology: Chao Cheng, Minyi Zhu; formal analysis and investigation: Chao Cheng, Minyi Zhu, Tianlan Lin, Ziyan Chen, Weiting Zeng, Kunke Li, Ran Xue, Fang Duan; writing (original draft preparation): Chao Cheng; writing (review and editing): Kaili Wu; funding acquisition: Kaili Wu; supervision: Kaili Wu.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was obtained before the procedures adhered to the tenets of the 1964 Declaration of Helsinki. Protocols were approved by the Institutional Ethics Committee of Zhongshan Ophthalmic Center (approval ID: 2014MEKY013, 2018KYPJ140, Medical Ethics Committee, Sun Yat-sen University, Guangzhou, China).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, C., Zhu, M., Lin, T. et al. Recharacterization of superior limbic keratoconjunctivitis via a subdividing grading method in 236 Chinese patients. Graefes Arch Clin Exp Ophthalmol 260, 2291–2298 (2022). https://doi.org/10.1007/s00417-022-05575-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05575-z