Abstract
Purpose
In prospective no-masking, comparative, crossover monocenter clinical trial, we aimed to evaluate whether the optimal subjective refraction technique varies with the keratoconus topography and to identify relevant topographic criteria.
Method
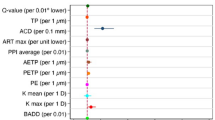
This study included 72 keratoconus eyes with impaired visual acuity. Each eye tested three methods of refraction (Jackson cylinder, astigmatism dial, stenopeic slit), resulting in three eyeglass lenses. Patients were assigned to the group corresponding to the eyeglass lens offering the best visual acuity. Five topographical characteristics were collected via the Pentacam: mean keratometry (Km), maximum keratometry (Kmax), distance from corneal center to Kmax (dKmax), Belin/Ambrosio Display (BAD_D), and index of surface variance (ISV).
Results
Forty-six eyes were included in the dial group (64.8%), 23 eyes in the cylinder group (32.4%), and only 2 eyes in the slit group (2.8%); thus, we only compared dial and cylinder groups. The main analysis retrieved a significant probability to choose dial technic for BAD_D (p = 0.024); when BAD_D is > 9.71 (ROC threshold), the positive predictive value (PPV) = 89.5%, and for ISV, p = 0.012; when ISV is > 77, PPV = 89.1%. The sub-analysis of patients with different visual acuities between cylinder and dial confirmed these results with slightly different thresholds: the probability to choose dial technic was for BAD_D, p = 0.03; when BAD_D is > 7.55, PPV = 90%, and for ISV, p = 0.0084; when ISV is > 71, PPV = 88.5%.
Conclusion
Refraction method is linked to topographic indices ISV and BAD_D. A BAD_D > 7.55 indicates the dial method. In addition to keratoconus screening and diagnosis, this study suggests a new application of the topographer to select a suitable refraction method for eyeglass prescription.
Trial registration
Study registered on the ClinicalTrials.gov database under n°: NCT04174209.





Similar content being viewed by others
References
Gomes JAP, Tan D, Rapuano CJ et al (2015) Global consensus on keratoconus and ectatic diseases. Cornea 34:359–369. https://doi.org/10.1097/ICO.0000000000000408
Bourdiol AM, Bron A, Amalric P (2012) Kératocône. In: SNOF. https://www.snof.org/encyclopedie/k%C3%A9ratoc%C3%B4ne. Accessed 26 Nov 2019
Gokhale NS (2013) Epidemiology of keratoconus. Indian J Ophthalmol 61:382–383. https://doi.org/10.4103/0301-4738.116054
Tuft SJ, Moodaley LC, Gregory WM et al (1994) Prognostic factors for the progression of keratoconus. Ophthalmology 101:439–447. https://doi.org/10.1016/s0161-6420(94)31313-3
Zadnik K, Steger-May K, Fink BA et al (2002) Between-eye asymmetry in keratoconus. Cornea 21:671–679. https://doi.org/10.1097/00003226-200210000-00008
McMahon TT, Edrington TB, Szczotka-Flynn L et al (2006) Longitudinal changes in corneal curvature in keratoconus. Cornea 25:296–305. https://doi.org/10.1097/01.ico.0000178728.57435.df
Levit A, Benwell M, Evans BJW (2020) Randomised controlled trial of corneal vs. scleral rigid gas permeable contact lenses for keratoconus and other ectatic corneal disorders. Cont Lens Anterior Eye 43(6):543–552. https://doi.org/10.1016/j.clae.2019.12.007
Jinabhai AN (2020) Customised aberration-controlling corrections for keratoconic patients using contact lenses. Clin Exp Optom 103:31–43. https://doi.org/10.1111/cxo.12937
Yuksel Elgin C, Iskeleli G, Aydin O (2018) Effects of the rigid gas permeable contact lense use on tear and ocular surface among keratoconus patients. Cont Lens Anterior Eye 41:273–276. https://doi.org/10.1016/j.clae.2017.12.013
Li W, Wang B (2017) Efficacy and safety of transepithelial corneal collagen crosslinking surgery versus standard corneal collagen crosslinking surgery for keratoconus: a meta-analysis of randomized controlled trials. BMC Ophthalmol 17:262. https://doi.org/10.1186/s12886-017-0657-2
Kaiserman I, Mimouni M, Rabina G (2019) Epithelial photorefractive keratectomy and corneal cross-linking for keratoconus: the Tel-Aviv protocol. J Refract Surg 35:377–382. https://doi.org/10.3928/1081597X-20190514-01
Montalt JC, Porcar E, España-Gregori E, Peris-Martínez C (2019) Visual quality with corneo-scleral contact lenses after intracorneal ring segment (ICRS) implantation for keratoconus management. Cont Lens Anterior Eye 42:111–116. https://doi.org/10.1016/j.clae.2018.07.006
Soeters N, Muijzer MB, Molenaar J et al (2018) Autorefraction versus manifest refraction in patients with keratoconus. J Refract Surg 34:30–34. https://doi.org/10.3928/1081597X-20171130-01
Al-Tuwairqi WS, Ogbuehi KC, Razzouk H et al (2017) Agreement between autorefraction and subjective refraction in keraring-implanted keratoconic eyes. Eye Contact Lens 43:116–122. https://doi.org/10.1097/ICL.0000000000000244
Jinabhai A, O’Donnell C, Radhakrishnan H (2010) A comparison between subjective refraction and aberrometry-derived refraction in keratoconus patients and control subjects. Curr Eye Res 35:703–714. https://doi.org/10.3109/02713681003797921
Greenstein SA, Fry KL, Hersh PS (2011) Corneal topography indices after corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg 37:1282–1290. https://doi.org/10.1016/j.jcrs.2011.01.029
Alió JL, Piñero DP, Alesón A et al (2011) Keratoconus-integrated characterization considering anterior corneal aberrations, internal astigmatism, and corneal biomechanics. J Cataract Refract Surg 37:552–568. https://doi.org/10.1016/j.jcrs.2010.10.046
Jia H-Z, Peng X-J (2018) Efficacy of iontophoresis-assisted epithelium-on corneal cross-linking for keratoconus. Int J Ophthalmol 11:687–694. https://doi.org/10.18240/ijo.2018.04.25
Raiskup F, Theuring A, Pillunat LE, Spoerl E (2015) Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg 41:41–46. https://doi.org/10.1016/j.jcrs.2014.09.033
Kojima T, Nishida T, Nakamura T et al (2020) Keratoconus screening using values derived from auto-keratometer measurements: a multicenter study. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2020.02.017
Kandel H, Pesudovs K, Watson SL (2020) Measurement of quality of life in keratoconus. Cornea 39:386–393. https://doi.org/10.1097/ICO.0000000000002170
Colin J, Cochener B, Savary G, Malet F (2000) Correcting keratoconus with intracorneal rings. J Cataract Refract Surg 26:1117–1122. https://doi.org/10.1016/s0886-3350(00)00451-x
Vega-Estrada A, Alio JL, Brenner LF et al (2013) Outcome analysis of intracorneal ring segments for the treatment of keratoconus based on visual, refractive, and aberrometric impairment. Am J Ophthalmol 155:575-584.e1. https://doi.org/10.1016/j.ajo.2012.08.020
Song Y, Zhang J, Pan Z (2019) Systematic review and meta-analysis of clinical outcomes of penetrating keratoplasty versus deep anterior lamellar keratoplasty for keratoconus. Exp Clin Transplant. https://doi.org/10.6002/ect.2019.0123
Naderan M, Jahanrad A (2017) Topographic, tomographic and biomechanical corneal changes during pregnancy in patients with keratoconus: a cohort study. Acta Ophthalmol 95:e291–e296. https://doi.org/10.1111/aos.13296
Taradaj K, Ginda T, Maciejewicz P et al (2018) Pregnancy and the eye. Changes in morphology of the cornea and the anterior chamber of the eye in pregnant woman. Ginekol Pol 89:695–699. https://doi.org/10.5603/GP.a2018.0117
Agrawal N, Agarwal LT, Lavaju P, Chaudhary SK (2018) Physiological ocular changes in various trimesters of pregnancy. Nepal J Ophthalmol 10:16–22. https://doi.org/10.3126/nepjoph.v10i1.21685
Lopes T, B, Lopes T, C Ramos I, et al (2012) Correlation of topometric and tomographic indices with visual acuity in patients with keratoconus. International Journal of Keratoconus and Ectatic Corneal Diseases 1:167–172. https://doi.org/10.5005/jp-journals-10025-1032
Fredriksson A, Behndig A (2016) Eccentric small-zone ray tracing wavefront aberrometry for refraction in keratoconus. Acta Ophthalmol 94:679–684. https://doi.org/10.1111/aos.13183
Schmitt P-T, Simonpoli S, Colin J (2008) Kératocône : corrélations clinico-topographiques évaluées par l’Orbscan ®. J Fr Ophtalmol. 8 mars 29 9:1001‑11. 101019-200607892
Değirmenci C, Palamar M, İsmayilova N et al (2019) Topographic evaluation of unilateral keratoconus patients. Turk J Ophthalmol 49:117–122. https://doi.org/10.4274/tjo.galenos.2018.90958
Lombardo M, Giannini D, Lombardo G, Serrao S (2017) Randomized controlled trial comparing transepithelial corneal cross-linking using iontophoresis with the Dresden protocol in progressive keratoconus. Ophthalmology 124:804–812. https://doi.org/10.1016/j.ophtha.2017.01.040
Wittig-Silva C, Chan E, Islam FMA et al (2014) A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophthalmology 121:812–821. https://doi.org/10.1016/j.ophtha.2013.10.028
Kosekahya P, Caglayan M, Koc M et al (2019) Longitudinal evaluation of the progression of keratoconus using a novel progression display. Eye Contact Lens 45:324–330. https://doi.org/10.1097/ICL.0000000000000582
Hashemi H, Beiranvand A, Yekta A et al (2016) Pentacam top indices for diagnosing subclinical and definite keratoconus. Journal of Current Ophthalmology 28:21–26. https://doi.org/10.1016/j.joco.2016.01.009
Gatinel D (2019) Indices and screening tests for subclinical keratoconus. https://www.gatinel.com/recherche-formation/keratocone-2/indices-and-screening-tests-for-subclinical-keratoconus/. Accessed 24 Feb 2019
Shajari M, Steinwender G, Herrmann K et al (2019) Evaluation of keratoconus progression. Br J Ophthalmol 103:551–557. https://doi.org/10.1136/bjophthalmol-2017-311651
Orucoglu F, Toker E (2015) Comparative analysis of anterior segment parameters in normal and keratoconus eyes generated by Scheimpflug tomography. J Ophthalmol 2015:925414. https://doi.org/10.1155/2015/925414
Ferreira-Mendes J, Lopes BT, Faria-Correia F et al (2019) Enhanced ectasia detection using corneal tomography and biomechanics. Am J Ophthalmol 197:7–16. https://doi.org/10.1016/j.ajo.2018.08.054
Grzybowski A, Kanclerz P (2018) Beginnings of astigmatism understanding and management in the 19th century. Eye Contact Lens 44(Suppl 1):S22–S29. https://doi.org/10.1097/ICL.0000000000000449
Schiefer U, Kraus C, Baumbach P et al (2016) Refractive errors Dtsch Arztebl Int 113:693–702. https://doi.org/10.3238/arztebl.2016.0693
AAO, SFO, Albou-Ganem C (2015) Optique clinique. Elsevier Masson
Brooks NO, Greenstein S, Fry K, Hersh PS (2012) Patient subjective visual function after corneal collagen crosslinking for keratoconus and corneal ectasia. J Cataract Refract Surg 38:615–619. https://doi.org/10.1016/j.jcrs.2011.11.029
Delrivo M, Ruiseñor Vázquez PR, Galletti JD et al (2014) Agreement between placido topography and Scheimpflug tomography for corneal astigmatism assessment. J Refract Surg 30:49–53. https://doi.org/10.3928/1081597x-20131217-06
Asharlous A, Khabazkhoob M, Yekta A, Hashemi H (2017) Comprehensive profile of bilateral astigmatism: rule similarity and symmetry patterns of the axes in the fellow eyes. Ophthalmic Physiol Opt 37:33–41. https://doi.org/10.1111/opo.12344
Tabachnick BG, Fidell LS (2001) Using multivariate statistic, 4th edn. Allyn & Bacon, Boston
Comrey AL, Lee HB (1992) A first course in factor analysis, 2nd ed. Lawrence Erlbaum Associates, Inc
Kwiatkowski F, Girard M, Hacene K, Berlie J (2000) Sem: a suitable statistical software adapted for research in oncology. Bull Cancer 87:715–721
Piñero DP, Alio JL, Barraquer RI et al (2010) Corneal biomechanics, refraction, and corneal aberrometry in keratoconus: an integrated study. Invest Ophthalmol Vis Sci 51:1948–1955. https://doi.org/10.1167/iovs.09-4177
John AK, Asimellis G (2013) Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol 7:1539–1548. https://doi.org/10.2147/OPTH.S44741
Gatinel D (2019) Indices de dépistage. https://www.gatinel.com/recherche-formation/keratocone-2/indices-de-depistage/. Accessed 20 Nov 2019
Roshdy MM, Wahba SS, Fikry RR (2018) New corneal assessment index from the relational thickness and other OCULUS values (CAIRO Index). Clin Ophthalmol 12:1527–1532. https://doi.org/10.2147/OPTH.S171827
Atchison DA, Schmid KL, Edwards KP et al (2001) The effect of under and over refractive correction on visual performance and spectacle lens acceptance. Ophthalmic Physiol Opt 21:255–261. https://doi.org/10.1046/j.1475-1313.2001.00588.x
Freeman CE, Evans BJW (2010) Investigation of the causes of non-tolerance to optometric prescriptions for spectacles. Ophthalmic Physiol Opt 30:1–11. https://doi.org/10.1111/j.1475-1313.2009.00682.x
Orphanet (2018) Centre de référence du kératocône (CRNK) - centre de compétence. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=fr&Expert=512855. Accessed 6 Aug 2021
Woog K, Picherau L, Pean V, Gatinel D (2019) Répétabilité intra-examinateurs et reproductibilité inter-examinateurs d’une réfraction subjective. Réal Ophtalmol 47–53
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Committee for the Protection of Persons West III obtained October 23, 2019: 19.10.81/SI CNRIPH 19.09.12.62047/reference, 2019-A01624-53. Protocol V.1 (20/03/2019). This was approved by the CNIL and in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Metzger, M., Navel, V., Barrière, JV. et al. Benefits of using corneal topography to choose subjective refraction technique in keratoconus (RE-CON): a prospective comparative crossover clinical study. Graefes Arch Clin Exp Ophthalmol 260, 197–207 (2022). https://doi.org/10.1007/s00417-021-05382-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05382-y