Abstract
Purpose
To evaluate the treatment efficacy of the preoperative base-out recovery point as the surgical target angle for acute acquired comitant esotropia.
Methods
Prospective study. Twenty-two patients with acute acquired comitant esotropia (AACE) underwent strabismus surgery based on the target angle of the preoperative base-out recovery point. The postoperative deviation, positive fusional vergence, and negative fusional vergence were evaluated and compared with those of 23 normal individuals.
Results
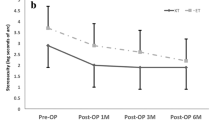
The mean follow-up period was 18.68 ± 19.48 months. At the last follow-up, 19 (86.4%) of 22 subjects had orthophoria, whereas 3 (13.6%) had minimal esophoria. The postoperative angle of deviation was significantly smaller than the preoperative angle of deviation at near (P < 0.001) and distance (P < 0.001). Postoperative sensory fusion was significantly better than preoperative fusion at near (P < 0.001) and distance (P < 0.001). The postoperative stereoacuity improved significantly after the surgery at near (P < 0.001) and distance (P < 0.001). Compared with the controls, the convergence and divergence amplitudes in the AACE patients were similar at distance (P > 0.05) but were still narrower at near (P < 0.001).
Conclusion
Good alignment and binocular balance were obtained with the surgical target angle of the base-out recovery point in AACE.



Similar content being viewed by others
Availability of data and materials
Not applicable.
Code availability
Not applicable.
References
Lee JM, Kim SH, Lee JI, Ryou JY, Kim SY (2009) Acute comitant esotropia in a child with a cerebellar tumor. Korean J Ophthalmol 23:228–231. https://doi.org/10.3341/kjo.2009.23.3.228
Hentschel SJ, Yen KG, Lang FF (2005) Chiari I malformation and acute acquired comitant esotropia: case report and review of the literature. J Neurosurg 102:407–412. https://doi.org/10.3171/ped.2005.102.4.0407
Weeks CL, Hamed LM (1999) Treatment of acute comitant esotropia in Chiari I malformation. Ophthalmology 106:2368–2371. https://doi.org/10.1016/S0161-6420(99)90541-9
Kemmanu V, Hegde K, Seetharam R, Shetty BK (2012) Varied aetiology of acute acquired comitant esotropia: a case series. Oman J Ophthalmol 5:103–105. https://doi.org/10.4103/0974-620X.99373
Cruysberg JR, Draaijer RW, Sellar PW (1996) When is acute onset concomitant esotropia a sign of serious neurological disease? Br J Ophthalmol 80:380. https://doi.org/10.1136/bjo.80.4.380
Burian HM, Miller JE (1958) Comitant convergent strabismus with acute onset. Am J Ophthalmol 45:55–64. https://doi.org/10.1016/0002-9394(58)90223-x
Lee HS, Park SW, Heo H (2016) Acute acquired comitant esotropia related to excessive Smartphone use. BMC Ophthalmol 16:37. https://doi.org/10.1186/s12886-016-0213-5
Prism Adaptation Study Research Group (1990) Efficacy of prism adaptation in the surgical management of acquired esotropia. Prism Adaptation Study Research Group. Arch Ophthalmol 108:1248–1256. https://doi.org/10.1001/archopht.1990.01070110064026
Scott WE, Thalacker JA (1984) Preoperative prism adaptation in acquired esotropia. Ophthalmologica 189:49–53. https://doi.org/10.1159/000309384
Repka MX, Connett JE, Scott WE (1996) The one-year surgical outcome after prism adaptation for the management of acquired esotropia. Ophthalmology 103:922–928. https://doi.org/10.1016/s0161-6420(96)30586-1
Campos EC (2008) Why do the eyes cross? A review and discussion of the nature and origin of essential infantile esotropia, microstrabismus, accommodative esotropia, and acute comitant esotropia. J AAPOS 12:326–331. https://doi.org/10.1016/j.jaapos.2008.03.013
Burke JP, Firth AY (1995) Temporary prism treatment of acute esotropia precipitated by fusion disruption. Br J Ophthalmol 79:787. https://doi.org/10.1136/bjo.79.8.787
Dawson EL, Marshman WE, Adams GG (1999) The role of botulinum toxin A in acute-onset esotropia. Ophthalmology 106:1727–1730. https://doi.org/10.1016/S0161-6420(99)90360-3
Ali MH, Berry S, Qureshi A, Rattanalert N, Demer JL (2018) Decompensated esophoria as a benign cause of acquired esotropia. Am J Ophthalmol 194:95–100. https://doi.org/10.1016/j.ajo.2018.07.007
Zhang P, Zhang Y, Gao L, Yang J (2020) Comparison of the therapeutic effects of surgery following prism adaptation test versus surgery alone in acute acquired comitant esotropia. BMC Ophthalmol 20:303. https://doi.org/10.1186/s12886-020-01574-y
Ela-Dalman N, Velez G, Thacker N, Britt MT, Velez FG (2006) Maximum motor fusion combined with one-hour preoperative prism adaptation test in patients with acquired esotropia. J AAPOS 10:561–564. https://doi.org/10.1016/j.jaapos.2006.09.011
Velez FG, Rosenbaum AL (2002) Preoperative prism adaptation for acquired esotropia: long-term results. J AAPOS 6:168–173. https://doi.org/10.1067/mpa.2002.123397
Hoyt CS, Good WV (1995) Acute onset concomitant esotropia: when is it a sign of serious neurological disease? Br J Ophthalmol 79:498–501. https://doi.org/10.1136/bjo.79.5.498
Wright KW, Strube YNJ (2007) Color atlas of strabismus surgery: strategies and techniques, 3rd edn. Springer, New York
Von Noorden GK, Campos EC (2002) Binocular vision and ocular motility: theory and management of strabismus, 6th edn. Mosby, St. Louis
Goss DA (1995) Sheard’s Criterion. In: Goss DA (ed) Ocular accommodation, convergence, and fixation disparity: a manual of clinical analysis. Butterworth-Heinemann, Boston, pp 47–52
Scattergood KD, Brown MH, Guyton DL (1983) Artifacts introduced by spectacle lenses in the measurement of strabismic deviations. Am J Ophthalmol 96:439–448. https://doi.org/10.1016/s0002-9394(14)77906-1
Daum KM, Rutstein RP, Gt H, Clore KA, Corliss DA (1989) Evaluation of a new criterion of binocularity. Optom Vis Sci 66:218–228. https://doi.org/10.1097/00006324-198904000-00008
Alvarez TL, Scheiman M, Santos EM, Morales C, Yaramothu C, D’Antonio-Bertagnolli JV, Biswal BB, Gohel S, Li X (2020) The Convergence Insufficiency Neuro-mechanism in Adult Population Study (CINAPS) randomized clinical trial: design, methods, and clinical data. Ophthalmic Epidemiol 27:52–72. https://doi.org/10.1080/09286586.2019.1679192
Moon BY, Kim SY, Yu DS (2020) Receiver operating characteristic curve analysis of clinical signs for screening of convergence insufficiency in young adults. PLoS ONE 15:e0228313. https://doi.org/10.1371/journal.pone.0228313
Kattan JM, Velez FG, Demer JL, Pineles SL (2016) Relationship between binocular summation and stereoacuity after strabismus surgery. Am J Ophthalmol 165:29–32. https://doi.org/10.1016/j.ajo.2016.02.020
Spierer A (2003) Acute concomitant esotropia of adulthood. Ophthalmology 110:1053–1056. https://doi.org/10.1016/S0161-6420(03)00102-7
Legmann Simon A, Borchert M (1997) Etiology and prognosis of acute, late-onset esotropia. Ophthalmology 104:1348–1352. https://doi.org/10.1016/s0161-6420(97)30136-5
Sturm V, Menke MN, Knecht PB, Schoffler C (2011) Long-term follow-up of children with acute acquired concomitant esotropia. J AAPOS 15:317–320. https://doi.org/10.1016/j.jaapos.2011.03.018
Mims JL 3rd, Wood RC (2000) The maximum motor fusion test: a parameter for surgery for acquired esotropia. J AAPOS 4:211–216. https://doi.org/10.1067/mpa.2000.105307
Funding
This study was supported by the Zhejiang Provincial Natural Science Foundation of China (subject number: LY19H120004) and the Medical Health Science and Technology Project of the Zhejiang Provincial Health Commission (subject number: 2019KY110).
Author information
Authors and Affiliations
Contributions
Xinping Yu and Jinmao Chen contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Zhiyue Dai, Fuhao Zheng, Meiping Xu, Jinjing Zhou, Minghui Wan, Huanyun Yu, and Fang Hou. The first draft of the manuscript was written by Zhiyue Dai, and all authors commented on previous versions of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Eye Hospital of Wenzhou Medical University Scientific Ethics Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of the Eye Hospital of Wenzhou Medical University. This article does not contain any studies with animals performed by any of the authors.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent forms regarding publication of their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dai, Z., Zheng, F., Xu, M. et al. Effect of the base-out recovery point as the surgical target for acute acquired comitant esotropia. Graefes Arch Clin Exp Ophthalmol 259, 3787–3794 (2021). https://doi.org/10.1007/s00417-021-05318-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05318-6