Abstract
Purpose
This study aims to evaluate the efficacy and safety of intralesional diode laser pretreatment for facilitating surgery for orbital venous malformations (OVMs).
Methods
This is a retrospective, non-comparative, interventional cohort involving 23 consecutive OVM patients undergoing intralesional laser pretreatment followed by surgical excision. The main outcome measures included volumetric changes, exophthalmometry, cosmesis, and symptom scores as well as treatment-related adverse events.
Results
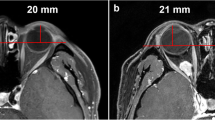
Following intralesional diode laser, the mean volume dropped significantly from 2366 ± 1887 to 129 ± 119 mm3 (t = 5.716; p < 0.001). After a single treatment session, a mean 90 ± 13% volume shrinkage was achieved in all 23 OVM. The mean Hertel exophthalmometry decreased significantly from 14 ± 3 to 13 ± 1 mm (t = 2.515; P < 0.02). The resolution of periocular dyschromasia and swelling were evident in 20 patients (87%). Symptom scores improved significantly from 6.5 ± 1.4 (very intense discomfort or effect on daily living) to 1.2 ± 1.0 (very mild discomfort or effect on daily living; p < 0.001). Short-term bruises and swelling were reported in 20 patients (87%).
Conclusion
Intralesional laser pretreatment is effective to facilitate surgery especially for the deep involving orbital venous malformations.




Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
Abbreviations
- BCVA:
-
Best-corrected visual acuity
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- OVM:
-
Orbital venous malformation
References
Wright JE (1974) Orbital vascular anomalies. Trans Am Acad Ophthalmol Otolaryngol 78:OP606-616
Boon LM, Ballieux F, Vikkula M (2011) Pathogenesis of vascular anomalies. Clin Plast Surg 38:7–19. https://doi.org/10.1016/j.cps.2010.08.012
Snebold N (1989) Diseases of the orbit: a multidisciplinary approach. Arch Ophthalmol 107:1285–1286. https://doi.org/10.1001/archopht.1989.01070020355014%JArchivesofOphthalmology
Dompmartin A, Vikkula M, Boon LM (2010) Venous malformation: update on aetiopathogenesis, diagnosis and management. Phlebology 25:224–235. https://doi.org/10.1258/phleb.2009.009041
Rootman J, Heran MK, Graeb DA (2014) Vascular malformations of the orbit: classification and the role of imaging in diagnosis and treatment strategies*. Ophthalmic Plast Reconstr Surg 30:91–104. https://doi.org/10.1097/iop.0000000000000122
Yen MT (2016) Vascular lesions of the orbit and face. Imaging Managhttps://doi.org/10.1007/978-3-319-29704-0
Lacey B, Rootman J, Marotta TR (1999) Distensible venous malformations of the orbit: clinical and hemodynamic features and a new technique of management. Ophthalmology 106:1197–1209. https://doi.org/10.1016/s0161-6420(99)90245-2
Couch SM, Garrity JA, Cameron JD, Cloft HJ (2009) Embolization of orbital varices with N-butyl cyanoacrylate as an aid in surgical excision: results of 4 cases with histopathologic examination. Am J Ophthalmol 148:614-618.e611. https://doi.org/10.1016/j.ajo.2009.04.024
Jia R, Xu S, Huang X, Song X, Pan H, Zhang L, He F, Lin M, Ge S, Fan X (2014) Pingyangmycin as first-line treatment for low-flow orbital or periorbital venous malformations: evaluation of 33 consecutive patients. JAMA ophthalmology 132:942–948. https://doi.org/10.1001/jamaophthalmol.2013.8229
Bagazgoitia L, Boixeda P, Lopez-Caballero C, Beà S, Santiago JL, Jaén P (2008) Venous malformation of the eyelid treated with pulsed-dye-1064-nm neodymium yttrium aluminum garnet sequential laser: an effective and safe treatment. Ophthalmic Plast Reconstr Surg 24:488–490. https://doi.org/10.1097/IOP.0b013e31818bed57
Mokhtarzadeh A, Garrity JA, Cloft HJ (2014) Recurrent orbital varices after surgical excision with and without prior embolization with n-butyl cyanoacrylate. Am J Ophthalmol 157:447-450.e441. https://doi.org/10.1016/j.ajo.2013.10.011
Schick U, Hassler W (2009) Treatment of deep vascular orbital malformations. Clin Neurol Neurosurg 111:801–807. https://doi.org/10.1016/j.clineuro.2009.08.004
Arat YO, Mawad ME, Boniuk M (2004) Orbital venous malformations: current multidisciplinary treatment approach. Arch Ophthalmol 122:1151–1158. https://doi.org/10.1001/archopht.122.8.1151
Jin Y, Lin X, Li W, Hu X, Ma G, Wang W (2008) Sclerotherapy after embolization of draining vein: a safe treatment method for venous malformations. J Vasc Surg 47:1292–1299. https://doi.org/10.1016/j.jvs.2008.01.010
Lin M, Li J, Jia RB, Fu Y, Fan XQJOiC (2009) Surgical flap raising and Nd:YAG lasers coagulation in the treatment of nondistensible orbital venous malformations. Ophthalmol in China 18:395–398
Schwarcz RM, Ben Simon GJ, Cook T, Goldberg RA (2006) Sclerosing therapy as first line treatment for low flow vascular lesions of the orbit. Am J Ophthalmol 141:333–339. https://doi.org/10.1016/j.ajo.2005.09.026
Anderson RR, Parrish JA (1983) Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science (New York, NY) 220:524–527. https://doi.org/10.1126/science.6836297
Proebstle TM, Lehr HA, Kargl A, Espinola-Klein C, Rother W, Bethge S, Knop J (2002) Endovenous treatment of the greater saphenous vein with a 940-nm diode laser: thrombotic occlusion after endoluminal thermal damage by laser-generated steam bubbles. J Vasc Surg 35:729–736. https://doi.org/10.1067/mva.2002.121132
Liu G, Liu X, Li W, Shi H, Ye K, Yin M, Huang Y, Lu X, Huang X, Lu M, Jiang M (2014) Ultrasound-guided intralesional diode laser treatment of congenital extratruncular venous malformations: mid-term results. Eur J Vasc Endovasc Surg 47:558–564. https://doi.org/10.1016/j.ejvs.2014.02.014
Patil U, Dhami L (2008) Overview of lasers. Indian J Plast Surg 41:S101–S113
Railan D, Parlette EC, Uebelhoer NS, Rohrer TE (2006) Laser treatment of vascular lesions. Clin Dermatol 24:8–15. https://doi.org/10.1016/j.clindermatol.2005.10.026
McHugh JD, Marshall J, Ffytche TJ, Hamilton AM, Raven A, Keeler CR (1989) Initial clinical experience using a diode laser in the treatment of retinal vascular disease. Eye (Lond) 3(Pt 5):516–527. https://doi.org/10.1038/eye.1989.83
Proebstle TM, Sandhofer M, Kargl A, Gül D, Rother W, Knop J, Lehr HA (2002) Thermal damage of the inner vein wall during endovenous laser treatment: key role of energy absorption by intravascular blood. Dermatol Surg 28:596–600. https://doi.org/10.1046/j.1524-4725.2002.01309.x
Sidhu MK, Perkins JA, Shaw DW, Bittles MA, Andrews RT (2005) Ultrasound-guided endovenous diode laser in the treatment of congenital venous malformations: preliminary experience. J Vasc Interv Radiol 16:879–884. https://doi.org/10.1097/01.Rvi.0000163005.50283.62
Álvarez-Camino JC, España-Tost AJ, Gay-Escoda C (2013) Endoluminal sclerosis with diode laser in the treatment of orofacial venous malformations. Med Oral Patol Oral Cir Bucal 18:e486-490. https://doi.org/10.4317/medoral.18528
Acknowledgements
We would like to include the surgery team of the ophthalmology department for their exquisite surgery and good care of the patients. We were grateful of the pathology department and the radiology department for offering fine reports. Medical editor Katharine O’Moore-Klopf, ELS (East Setauket, NY, USA), provided professional English language editing of the manuscript.
Funding
The present study was supported by the National Natural Science Foundation of China (grant number 81570884, 81872339, 81802702), Shanghai Sailing Program (grant number 17YF1410700), and Interdisciplinary Program of Shanghai Jiao Tong University (YG2016MS02), hospital-level nursing research projects funded by Shanghai 9th People’s Hospital (JYHL20161914), the “top priority” in nursing research projects funded by Shanghai Jiaotong University, School of Medicine (JYHZ1814).
Author information
Authors and Affiliations
Contributions
Renbing Jia and Ludwig M. Heindl designed the study and made detailed plan. Yinwei Li, Yefei Wang, and Xianqun Fan checked and operated on the patients. Yingxiu Luo collected the patients’ information. Minyue Xie and Tianyuan Li reviewed all data and wrote the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of the institutional ethical review board of Shanghai Ninth People’s Hospital.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xie, M., Li, T., Luo, Y. et al. Intralesional diode laser pretreatment facilitates surgery for orbital venous malformations: initial experience with 23 consecutive patients. Graefes Arch Clin Exp Ophthalmol 260, 303–309 (2022). https://doi.org/10.1007/s00417-021-05272-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05272-3