Abstract
Purpose
To determine the difference between the attempted and the achieved postoperative refractive error after sutureless intrascleral fixation of the haptics of an implanted intraocular lens (IOL).
Patients and methods
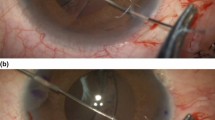
This was a retrospective study of the medical charts of patients who had undergone sutureless intrascleral fixation of an IOL. The IOLs were fixed by inserting the haptics into scleral tunnels with or without flanges. The differences between the attempted and achieved postoperative refractive error (spherical equivalent) were determined. The relationships between the surgical options and the differences of the refractive error and degree of astigmatism were also determined.
Results
Two hundred and twenty-three eyes were studied. There was a myopic shift of − 0.38 ± 1.13 diopters (D). The mean of the differences between the achieved postoperative and the attempted refractive error was 0.89 ± 0.79 D. The achieved refractive error was significantly correlated with the attempted refractive error (P < 0.001, R2 = 0.631). The surgical procedures selected were not significantly associated with the differences between the attempted and achieved refractive error. The size of sclerocorneal incision and presence of sutures were significantly associated with the final degree of astigmatism (P = 0.006 and 0.008, respectively).
Conclusions
The postoperative refractive error was significantly correlated with the attempted refractive error after intrascleral fixation of an IOL. The wound construction was associated with the postoperative degree of astigmatism.


Similar content being viewed by others
References
Weene LE (1993) Flexible open-loop anterior chamber intraocular lens implants. Ophthalmology 100:1636–1639. https://doi.org/10.1016/s0161-6420(13)31445-6
Hennig A, Evans JR, Pradhan D, Johnson GJ, Pokhrel RP, Gregson RM, Hayes R, Wormald RP, Foster A (1997) Randomised controlled trial of anterior-chamber intraocular lenses. Lancet 349:1129–1133. https://doi.org/10.1016/s0140-6736(96)11043-6
Toro MD, Longo A, Avitabile T, Nowomiejska K, Gagliano C, Tripodi S, Choragiewicz T, Kaminska A, Figus M, Posarelli C, Forlini M, Junemann AGM, Reibaldi M, Rejdak R (2019) Five-year follow-up of secondary iris-claw intraocular lens implantation for the treatment of aphakia: Anterior chamber versus retropupillary implantation. PLoS ONE 14:e0214140. https://doi.org/10.1371/journal.pone.0214140
Insler MS, Mani H, Peyman GA (1988) A new surgical technique for dislocated posterior chamber intraocular lenses. Ophthalmic Surg 19:480–481
Sarrafizadeh R, Ruby AJ, Hassan TS, Williams GA, Garretson BR, Trese MT, Margherio RR (2001) A comparison of visual results and complications in eyes with posterior chamber intraocular lens dislocation treated with pars plana vitrectomy and lens repositioning or lens exchange. Ophthalmology 108:82–89. https://doi.org/10.1016/s0161-6420(00)00410-3
Apple DJ, Brems RN, Park RB, Norman DK, Hansen SO, Tetz MR, Richards SC, Letchinger SD (1987) Anterior chamber lenses. Part I: Complications and pathology and a review of designs. J Cataract Refract Surg 13:157–174. https://doi.org/10.1016/s0886-3350(87)80131-1
Liarakos VS, Ham L, Dapena I, Tong CM, Quilendrino R, Yeh RY, Melles GR (2013) Endothelial keratoplasty for bullous keratopathy in eyes with an anterior chamber intraocular lens. J Cataract Refract Surg 39:1835–1845. https://doi.org/10.1016/j.jcrs.2013.05.045
Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L (2006) Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol 141:308–312. https://doi.org/10.1016/j.ajo.2005.09.012
Price MO, Price FW Jr, Werner L, Berlie C, Mamalis N (2005) Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg 31:1320–1326. https://doi.org/10.1016/j.jcrs.2004.12.060
Kristianslund O, Raen M, Ostern AE, Drolsum L (2017) Late in-the-bag intraocular lens dislocation: a randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology 124:151–159. https://doi.org/10.1016/j.ophtha.2016.10.024
Schechter RJ (1990) Suture-wick endophthalmitis with sutured posterior chamber intraocular lenses. J Cataract Refract Surg 16:755–756. https://doi.org/10.1016/s0886-3350(13)81021-8
Gabor SG, Pavlidis MM (2007) Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg 33:1851–1854. https://doi.org/10.1016/j.jcrs.2007.07.013
Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S (2008) Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg 34:1433–1438. https://doi.org/10.1016/j.jcrs.2008.04.040
Kumar DA, Agarwal A, Packiyalakshmi S, Jacob S, Agarwal A (2013) Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules. J Cataract Refract Surg 39:1211–1218. https://doi.org/10.1016/j.jcrs.2013.03.004
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K (2017) Flanged intrascleral intraocular Lens fixation with double-needle technique. Ophthalmology 124:1136–1142. https://doi.org/10.1016/j.ophtha.2017.03.036
Todorich B, Stem MS, Kooragayala K, Thanos A, Faia LJ, Williams GA, Hassan TS, Woodward MA, Wolfe JD (2018) Structural analysis and comprehensive surgical outcomes of the sutureless intrascleral fixation of secondary intraocular lenses in human eyes. Retina 38(Suppl 1):S31–S40. https://doi.org/10.1097/IAE.0000000000001941
Abbey AM, Hussain RM, Shah AR, Faia LJ, Wolfe JD, Williams GA (2015) Sutureless scleral fixation of intraocular lenses: outcomes of two approaches. The 2014 Yasuo Tano Memorial Lecture. Graefes Arch Clin Exp Ophthalmol 253:1–5. https://doi.org/10.1007/s00417-014-2834-9
Czajka MP, Frajdenberg A, Stopa M, Pabin T, Johansson B, Jakobsson G (2020) Sutureless intrascleral fixation using different three-piece posterior chamber intraocular lenses: a literature review of surgical techniques in cases of insufficient capsular support and a retrospective multicentre study. Acta Ophthalmol 98:224–236. https://doi.org/10.1111/aos.14307
Retzlaff JA, Sanders DR, Kraff MC (1990) Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg 16:333–340. https://doi.org/10.1016/s0886-3350(13)80705-5
Kurimori HY, Inoue M, Hirakata A (2018) Adjustments of haptics length for tilted intraocular lens after intrascleral fixation. Am J Ophthalmol Case Rep 10:180–184. https://doi.org/10.1016/j.ajoc.2018.02.025
Yamane S, Maruyama-Inoue M, Kadonosono K (2019) Needle stabilizer for flanged intraocular lens fixation. Retina 39:801. https://doi.org/10.1097/IAE.0000000000002455
Steinert RF, Brint SF, White SM, Fine IH (1991) Astigmatism after small incision cataract surgery. A prospective, randomized, multicenter comparison of 4- and 6.5-mm incisions. Ophthalmology 98: 417–423; discussion 423–414
Churchill AJ, Hillman JS (1996) Post-operative astigmatism control by selective suture removal. Eye (Lond) 10(Pt 1):103–106. https://doi.org/10.1038/eye.1996.17
Stanford MR, Fenech T, Hunter PA (1993) Timing of removal of sutures in control of post-operative astigmatism. Eye (Lond) 7(Pt 1):143–147. https://doi.org/10.1038/eye.1993.30
Suto C, Hori S, Fukuyama E, Akura J (2003) Adjusting intraocular lens power for sulcus fixation. J Cataract Refract Surg 29:1913–1917. https://doi.org/10.1016/s0886-3350(03)00250-5
Acknowledgements
The authors thank Professor Emeritus Duco Hamasaki of the Bascom Palmer Eye Institute of the University of Miami for his critical discussion and editing of the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Chiba University Graduate School of Medicine and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
TB: personal fees from Bayer, Kowa, Santen, Senju, Alcon, grants, and personal fees from Novartis, outside the submitted work. SY: grants and personal fees from HOYA, Senju, Pfizer, Santen, Alcon Japan, Alcon Pharma, Bayer, Kowa, personal fees from Nikon, Wakamoto, Chuo Sangyo, Daiichi Sankyo, Jamecs, Sun Contact Lens, Finedex, Novartis, Chugai, Abbvie, outside the submitted work. The following authors have no financial disclosures: MK, TT, TI, TN, GM.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kakisu, M., Baba, T., Tatsumi, T. et al. Refractive errors after sutureless intrascleral fixation of intraocular lens. Graefes Arch Clin Exp Ophthalmol 259, 3003–3009 (2021). https://doi.org/10.1007/s00417-021-05268-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05268-z