Abstract
Background
Due to the guarded prognosis of acute retinal necrosis (ARN), it is relevant to develop a strategy to early categorize those patients in a higher risk of worse outcomes. The purpose of this study is to describe clinical features and predictive factors for retinal detachment (RD) in patients with ARN.
Methods
Retrospective observational case series of 34 adult patients (38 eyes) with ARN examined between January 2005 and July 2015 in the National Eye Institute (Bethesda, USA), the Department of Ophthalmology, University of Chile (Santiago, Chile), and APEC (CDMX, Mexico).
Results
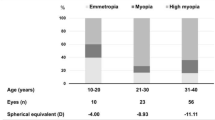
A total of 16 males and 18 females with a mean age at presentation of 44.5 ± 16.8 years were included. Twenty-seven patients (79.4%) received intravenous acyclovir as first-line treatment, and 7 patients received either oral antiviral (4 patients) or oral plus intravitreal antiviral (3 patients). All subjects were treated with prednisone, with a mean initial dose of 57.7 ± 16.3 mg per day. Seventeen patients (50.0%) developed retinal detachment. An association of retinal detachment with age at onset was observed (p = 0.04), with patients younger than 50 years presenting a higher risk (OR = 14.86, p = 0.0009). Additionally, patients in this higher risk group had more inflammation in both anterior chamber and vitreous (p = 0.04 and 0.03, respectively). No other predictive factor for retinal detachment was found in the present study.
Conclusions
RD represents an important complication in patients with ARN. Younger patients may be at higher risk of this complication, possibly secondary to the presence of a higher level of inflammation.


Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ARN:
-
Acute retinal necrosis
- RD:
-
Retinal detachment
- VZV:
-
Varicella zoster Virus
- NEI:
-
National Eye Institute
- APEC:
-
Asociacion para Evitar la Ceguera
- BCVA:
-
Best-corrected visual acuity
- ROC:
-
Receiver operating characteristic curve
- HSV:
-
Herpes simplex Virus
- PVD:
-
Posterior vitreous detachment
References
Muthiah MN, Michaelides M, Child CS, Mitchell SM (2007) Acute retinal necrosis: A national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 91(11):1452–1455
Holland GN, Standard diagnostic criteria for the acute retinal necrosis syndrome. (1994) Executive Committee of the American Uveitis Society. Am J Ophthalmol 117(5):663–667
Roy R, Pal BP, Mathur G, Rao C, Das D, Biswas J (2014) Acute retinal necrosis: Clinical features, management and outcomes–A 10 year consecutive case series. Ocul Immunol Inflamm 22(3):170–174
Lau CH, Missotten T, Salzmann J, Lightman SL (2007) Acute retinal necrosis features, management, and outcomes. Ophthalmology 114(4):756–762
Wong RW, Jumper JM, McDonald HR, Johnson NR, Fu A, Lujan BJ, Cunningham ET Jr (2013) Emerging concepts in the management of acute retinal necrosis. Br J Ophthalmol 97(5):545–552
Sims JL, Yeoh J, Stawell RJ (2009) Acute retinal necrosis: A case series with clinical features and treatment outcomes. Clin Exp Ophthalmol 37(5):473–477
Wong R, Pavesio CE, Laidlaw DA, Williamson TH, Graham EM, Stanford MR (2010) Acute retinal necrosis: The effects of intravitreal foscarnet and virus type on outcome. Ophthalmology 117(3):556–560
Park JJ, Pavesio C (2008) Prophylactic laser photocoagulation for acute retinal necrosis. Does it raise more questions than answers? Br J Ophthalmol 92(9):1161–1162
Risseeuw S, de Boer JH, Ten Dam-van Loon NH, van Leeuwen R (2019) Risk of rhegmatogenous retinal detachment in acute retinal necrosis with and without prophylactic intervention. Am J Ophthalmol 206:140–148
Yeh S, Suhler EB, Smith JR et al (2014) Combination systemic and intravitreal antiviral therapy in the management of acute retinal necrosis syndrome. Ophthalmic Surg Lasers Imaging Retina 45(5):399–407
Winterhalter S, Stuebiger N, Maier AK et al (2016) Acute retinal necrosis: Diagnostic and treatment strategies in Germany. Ocul Immunol Inflamm 24(5):537–543
Jabs DA, Nussenblatt RB, Rosenbaum JT (2005) Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 140(3):509–516
Butler NJ, Moradi A, Salek SS et al (2017) Acute retinal necrosis: Presenting characteristics and clinical outcomes in a cohort of polymerase chain reaction-positive patients. Am J Ophthalmol 179:179–189
Li AL, Fine HF, Shantha JG, Yeh S (2019) Update on the management of acute retinal necrosis. Ophthalmic Surg Lasers Imaging Retina 50(12):748–751
Van Gelder RN, Willig JL, Holland GN, Kaplan HJ (2001) Herpes simplex virus type 2 as a cause of acute retinal necrosis syndrome in young patients. Ophthalmology 108(5):869–876
Clark A, Morlet N, Ng JQ, Preen DB, Semmens JB (2012) Risk for retinal detachment after phacoemulsification: A whole-population study of cataract surgery outcomes. Arch Ophthalmol 130(7):882–888
Kakehashi A, Kado M, Akiba J, Hirokawa H (1997) Variations of posterior vitreous detachment. Br J Ophthalmol 81(7):527–532
Labalette P, Delhaes L, Margaron F, Fortier B, Rouland JF (2002) Ocular toxoplasmosis after the fifth decade. Am J Ophthalmol 133(4):506–515
Mitry D, Fleck BW, Wright AF, Campbell H, Charteris DG (2010) Pathogenesis of rhegmatogenous retinal detachment: Predisposing anatomy and cell biology. Retina 30(10):1561–1572
Author information
Authors and Affiliations
Contributions
Conception and design: CAU, JK. Data collection: CAU, JK, UM-P, RA. Analysis and interpretation: all authors. Drafting the work and revising it critically for important intellectual content: all authors. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients were seen under an Institutional Review Board–approved protocol at their respective clinics and the Ethics Committee of the University of Chile approved the study (ID: 0062019). The protocol fulfilled the tenets of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Urzua, C.A., Knickelbein, J., Cuitino, L. et al. Association of retinal detachment with age 50 years or younger at onset in patients with acute retinal necrosis. Graefes Arch Clin Exp Ophthalmol 259, 2905–2911 (2021). https://doi.org/10.1007/s00417-021-05166-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05166-4