Abstract
Purpose
To quantify a passive range of cyclorotation using a smartphone application and evaluate its associations with fundus torsion and rectus muscle cyclorotation in superior oblique palsy (SOP) and V-pattern strabismus.
Methods
Fifty-two patients showing overelevation in adduction (30 with congenital SOP and 22 with V-pattern strabismus) underwent forced cyclorotation on the photographs. A photograph of the globe was taken in maximally excyclorotated and incyclorotated positions after marking at the 6 and 12 o’clock limbus under general anaesthesia, and the rotational alignment of these markings was read using the toriCAM application. The degrees of forced cyclorotation were compared between the two groups. Disc-fovea angle on fundus photographs and rectus muscle cyclorotation in the coronal view on orbital computed tomography were correlated with the range of forced excyclorotation.
Results
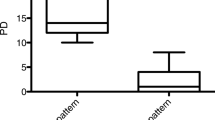
The range of forced excyclorotation was greater in V-pattern strabismus than that in SOP (58.5° vs. 46.8°, p < 0.001), whereas the ranges of incyclorotation were similar between the two groups (39.0° vs. 39.0°, p = 0.543). Regression analysis revealed a significant increase in the range of excyclorotation with the degree of rectus muscle excyclorotation, after accounting for age and angle of hypertropia (r2 = 0.475, p = 0.001). The range of excyclorotation did not correlate with the amount of fundus extorsion and grade of overelevation in adduction.
Conclusions
The range of excyclorotation was correlated with the rectus muscle excyclorotation in these populations, suggesting that the results from this forced cyclorotation test may reflect orbital alignment and oblique muscle status.




Similar content being viewed by others
References
Jung JH, Holmes JM (2015) Quantitative intraoperative torsional forced duction test. Ophthalmology 122:1932–1938
Lemos J, Eggenberger E (2013) Clinical utility and assessment of cyclodeviation. Curr Opin Ophthalmol 24:558–565
Lim HW, Lee JW, Hong E, Song Y, Kang MH, Seong M, Cho HY, Oh SY (2014) Quantitative assessment of inferior oblique muscle overaction using photographs of the cardinal positions of gaze. Am J Ophthalmol 158:793–799
Guyton DL (1981) Exaggerated traction test for the oblique muscles. Ophthalmology 88:1035–1040
Pallas A, Yeo TK, Trevenen M, Barrett G (2018) Evaluation of the accuracy of two marking methods and the novel toriCAM application for toric intraocular lens alignment. J Refract Surg 34:150–155
Lee JE, Yang HK, Kim JH, Hwang JM (2017) Ocular torsion according to trochlear nerve absence in unilateral superior oblique palsy. Invest Ophthalmol Vis Sci 58:5526–5531
Dagi LR, MacKinnon S, Zurakowski D, Prabhu SP (2017) Rectus muscle excyclorotation and V-pattern strabismus: a quantitative appraisal of clinical relevance in syndromic craniosynostosis. Br J Ophthalmol 101:1560–1565
Hao R, Suh SY, Le A, Demer JL (2016) Rectus extraocular muscle size and pulley location in concomitant and pattern exotropia. Ophthalmology 123:2004–2012
Weiss AH, Phillips J, Kelly JP (2014) Crouzon syndrome: relationship of rectus muscle pulley location to pattern strabismus. Invest Ophthalmol Vis Sci 55:310–317
Clark RA, Demer JL (2006) Magnetic resonance imaging of the effects of horizontal rectus extraocular muscle surgery on pulley and globe positions and stability. Invest Ophthalmol Vis Sci 47:188–194
Tan KP, Sargent MA, Poskitt KJ, Lyons CJ (2005) Ocular overelevation in adduction in craniosynostosis: is it the result of excyclorotation of the extraocular muscles? J AAPOS 9:550–557
Stephens KF, Reinecke RD (1967) Quantitative forced duction. Trans Am Acad Ophthalmol Otolaryngol 71:324–329
Metz HS (1985) Quantitative evaluation of the strabismus patient. Int Ophthalmol Clin 25:13–36
Rosenbaum AL, Myer JH (1980) New instrument for the quantitative determination of passive forced traction. Ophthalmology 87:158–163
Holmes JM, Hatt SR, Leske DA (2012) Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS 16:136–140
McCall LC, Isenberg SJ, Apt L (1993) The effect of torsional muscle dysfunction and surgery on eye position under general anesthesia. J Pediatr Ophthalmol Strabismus 30:154–156
Ludwig IH, Clark RA, Stager DR Sr (2013) New strabismus surgical techniques. J AAPOS 17:79–88
Ludwig IH (2009) Principles and management of complex strabismus. In: Wilson ME, Saunders RA, Trivedi RH (eds) Pediatric ophthalmology: current thought and a practical guide. Springer, Berlin, pp 141–152
Kono R, Okanobu H, Ohtsuki H, Demer JL (2008) Displacement of the rectus muscle pulleys simulating superior oblique palsy. Jpn J Ophthalmol 52:36–43
Suh SY, Le A, Clark RA, Demer JL (2016) Rectus pulley displacements without abnormal oblique contractility explain strabismus in superior oblique palsy. Ophthalmology 123:1222–1231
Demer JL (2014) Connective tissues reflect different mechanisms of strabismus over the life span. J AAPOS 18:309–315
von Noorden GK, Campos EC (2002) Binocular vision and ocular motility, 6th edn. CV Mosby, Philadelphia, pp 55–56
Shin KH, Lee HJ, Lim HT (2013) Ocular torsion among patients with intermittent exotropia: relationships with disease severity factors. Am J Ophthalmol 155:177–182
Lee TH, Ji YS, Park SW, Yoon KC, Heo H (2017) Intermittent exotropia with a positive Bielschowsky head-tilt test. Br J Ophthalmol 101:251–255
Kim DH, Lim HT (2019) Comparison of ocular torsion between congenital and acquired unilateral superior oblique palsy. Eye (Lond) 33:1658–1663
Deng H, Irsch K, Gutmark R, Phamonvaechavan P, Foo FY, Anwar DS, Guyton DL (2013) Fusion can mask the relationships between fundus torsion, oblique muscle overaction/underaction, and A-and V-pattern strabismus. J AAPOS 17:177–183
Funding
This study was supported by the National Research Foundation of Korea funded by the Ministry of Science, ICT, and Future Planning (2017R1C1B5017453; Seoul, South Korea).
Author information
Authors and Affiliations
Contributions
Design of the study: SAC. Conduct of the study: SAC and SJH. Collection and management of data: SAC and SJH. Analysis and interpretation of data: SAC and JHJ. Preparation, review, or approval of the manuscript: SAC, SJH, and JHJ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Patient consent for publication
Not required.
Ethics approval
This study was conducted in accordance with the tenets of the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of Ajou University School of Medicine, Suwon, South Korea (AJIRB-MED-OBS-20-096).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chung, S.A., Ha, S.J. & Jung, J.H. Range of forced cyclorotation in superior oblique palsy and V-pattern strabismus. Graefes Arch Clin Exp Ophthalmol 259, 1035–1043 (2021). https://doi.org/10.1007/s00417-020-04994-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04994-0