Abstract
Aim
To evaluate pre-operative qualitative and quantitative parameters of external limiting membranes (ELM) and other associated full thickness macular holes (FTMH) features and their predictive values for post-operative anatomical and functional outcomes.
Methods
This was a retrospective study of 48 eyes that underwent vitrectomy with internal limiting membrane (ILM) peeling for FTMH and had type 1 closure. All subjects underwent optical coherence tomography (SDOCT, Heidelberg, Spectralis), and the eyes were divided into complete ELM closure (CEC) and incomplete ELM closure (IEC) groups based on the post-operative OCTs within 2 months, and ROC curves were used to estimate which of the pre-operative parameters could best predict eyes falling in the CEC group.
Results
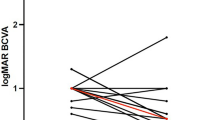
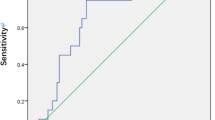
The mean pre-op ELM defect was smaller in CEC group (594 μm vs 1126 μm, p < 0.001) and so was the pre-op EZ defect (770 μm vs 1186 μm, p = 0.001). The mean ELM angle also was smaller in the CEC group (51.6° vs 102.5°, p < 0.001) and so was the mean hole inlet distance (353 μm vs 596 μm, p < 0.001). The post-operative ELM defect showed a significant negative correlation with visual acuity (r = − 0.319; p = 0.027). The ELM angle was most predictive with an AUROC of 0.958, and a cut-off of 68.3° had a sensitivity of 90% and a specificity of 89%.
Conclusion
Our study introduces a novel parameter called the ELM angle and proves that it has a high sensitivity and specificity in predicting complete ELM reformation post-surgery in the short term as well as the long term.




Similar content being viewed by others
References
Sano M, Shimoda Y, Hashimoto H, Kishi S (2009) Restored photoreceptor outer segment and visual recovery after macular hole closure. Am J Ophthalmol 147:313–318 e311. https://doi.org/10.1016/j.ajo.2008.08.002
Ko TH, Witkin AJ, Fujimoto JG, Chan A, Rogers AH, Baumal CR, Schuman JS, Drexler W, Reichel E, Duker JS (2006) Ultrahigh-resolution optical coherence tomography of surgically closed macular holes. Arch Ophthalmol 124:827–836. https://doi.org/10.1001/archopht.124.6.827
Inoue M, Watanabe Y, Arakawa A, Sato S, Kobayashi S, Kadonosono K (2008) Spectral-domain optical coherence tomography images of inner/outer segment junctions and macular hole surgery outcomes. Graefes Arch Clin Exp Ophthalmol 247:325. https://doi.org/10.1007/s00417-008-0999-9
Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J (2008) Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 246:823–830. https://doi.org/10.1007/s00417-007-0764-5
Shimozono M, Oishi A, Hata M, Kurimoto Y (2011) Restoration of the photoreceptor outer segment and visual outcomes after macular hole closure: spectral-domain optical coherence tomography analysis. Graefes Arch Clin Exp Ophthalmol 249:1469–1476. https://doi.org/10.1007/s00417-011-1681-1
Theodossiadis PG, Grigoropoulos VG, Theodossiadis GP (2011) The significance of the external limiting membrane in the recovery of photoreceptor layer after successful macular hole closure: a study by spectral domain optical coherence tomography. Ophthalmologica 225:176–184. https://doi.org/10.1159/000323322
Landa G, Gentile RC, Garcia PMT, Muldoon TO, Rosen RB (2012) External limiting membrane and visual outcome in macular hole repair: spectral domain OCT analysis. Eye 26:61–69. https://doi.org/10.1038/eye.2011.237
Wakabayashi T, Fujiwara M, Sakaguchi H, Kusaka S, Oshima Y (2010) Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology 117:1815–1824. https://doi.org/10.1016/j.ophtha.2010.01.017
Ooka E, Mitamura Y, Baba T, Kitahashi M, Oshitari T, Yamamoto S (2011) Foveal microstructure on spectral-domain optical coherence tomographic images and visual function after macular hole surgery. Am J Ophthalmol 152:283–290.e281. https://doi.org/10.1016/j.ajo.2011.02.001
Chhablani J, Khodani M, Hussein A, Bondalapati S, Rao HB, Narayanan R, Sudhalkar A (2015) Role of macular hole angle in macular hole closure. Br J Ophthalmol 99:1634–1638. https://doi.org/10.1136/bjophthalmol-2015-307014
Venkatesh R, Sinha S, Gangadharaiah D, Gadde SGK, Mohan A, Shetty R, Yadav NK (2019) Retinal structural-vascular-functional relationship using optical coherence tomography and optical coherence tomography - angiography in myopia. Eye Vis (Lond) 6:8. https://doi.org/10.1186/s40662-019-0133-6
Ruiz-Moreno JM, Staicu C, Piñero DP, Montero J, Lugo F, Amat P (2008) Optical coherence tomography predictive factors for macular hole surgery outcome. Br J Ophthalmol 92:640–644. https://doi.org/10.1136/bjo.2007.136176
Kusuhara S, Teraoka Escaño MF, Fujii S, Nakanishi Y, Tamura Y, Nagai A, Yamamoto H, Tsukahara Y, Negi A (2004) Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol 138:709–716. https://doi.org/10.1016/j.ajo.2004.04.063
Altaweel M, Ip M (2003) Macular hole: improved understanding of pathogenesis, staging, and management based on optical coherence tomography Seminars in ophthalmology. Taylor & Francis, Abingdon, pp 58–66
Acknowledgements
All contributors have been acknowledged as authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Chaithanya Ethics Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of a topical collection on Macular Holes
Rights and permissions
About this article
Cite this article
Nair, U., Menon, R.R., Mohan, A. et al. External limiting membrane angle as a composite predictive index for post-operative ELM closure in full thickness macular holes. Graefes Arch Clin Exp Ophthalmol 258, 2603–2609 (2020). https://doi.org/10.1007/s00417-020-04949-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04949-5