Abstract
Purpose
To characterize the fixation and macular integrity of subjects with multiple sclerosis (MS) with and without previous optic neuritis (ON) using microperimetry (MP).
Methods
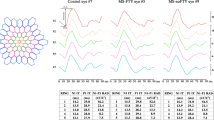
Fifty-five eyes of MS patients, subdivided into three groups (28 eyes without ON, 16 with previous ON, and 11 eyes with previous ON in the contralateral eye), and 43 healthy eyes were enrolled (January–November 2018). All cases were evaluated using the MAIA microperimeter (Centervue), analyzing the following parameters: average macular threshold (AT), fixation indexes (P1 and P2), bivariate contour ellipse area (BCEA) for 95% and 63% of points, and horizontal (H) and vertical (V) axes of the ellipse of fixation.
Results
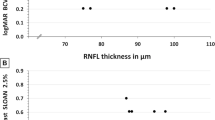
All MS groups showed a significant reduced AT compared with the control group (p < 0.001). This reduction was more representative (p < 0.001) in eyes with previous ON. No statistically significant differences were found between MS patients with and without previous ON (p > 0.05). Mean AT was correlated with the examination time in all three groups (between ρ = − 0.798 p < 0.001 and ρ = − 0.49 p < 0.001). Significant differences in fixation parameters were only found between control and MS with ON groups (p < 0.02). The ratio of the disease showed a significant correlation with fixation parameters in MS groups (p < 0.02), but not with AT.
Conclusions
In MS patients, macular sensitivity is altered, especially in eyes with previous ON. Likewise, a fixational instability is present in MS patients with ON, with more increase of the V axis of the fixation area than of the H. The ratio of the disease also affects the patient fixation pattern.



Similar content being viewed by others
References
Lublin FD, Reingold SC, Cohen JA et al (2014) Defining the clinical course of multiple sclerosis. Am Acad Neurol 83:278–286
Serra A, Chisari CG, Matta M (2018) Eye movement abnormalities in multiple sclerosis: pathogenesis, modeling, and treatment. Front Neurol 9:31
Pozzilli C, Tomassini V, Marinelli F, Paolillo A, Gasperini C, Bastianello S (2003) “Gender gap” in multiple sclerosis: magnetic resonance imaging evidence. Eur J Neurol 10:95–97
Galetta KM, Balcer LJ (2013) Measures of visual pathway structure and function in MS: clinical usefulness and role for MS trials. Mult Scler Relat Disord 2:172–182
Villoslada P, Cuneo A, Gelfand J, Hauser SL, Green A (2012) Color vision is strongly associated with retinal thinning in multiple sclerosis. Mult Scler 18:991–999
Cheng H, Laron M, Schiffman JS, Tang RA, Frishman LJ (2007) The relationship between visual field and retinal nerve fiber layer measurements in patients with multiple sclerosis. Invest Ophthalmol Vis Sci 48:5798–5805
Cerovski B, Vidović T, Petricek I et al (2005) Multiple sclerosis and neuro-ophthalmologic manifestations. Coll Antropol 29(Suppl 1):153–158
Bhatia I, Lukhmana S, Singh D, Menon V, Sharma P, Saxena R (2016) Microperimetry in optic neuritis. Ophthalmol Open J 1:21–28
Chan JW (2002) Optic neuritis in multiple sclerosis. Ocul Immunol Inflamm 10:161–186
Molina-Martín A, Pérez-Cambrodí RJ, Piñero DP (2018) Current clinical application of Microperimetry: a review. Semin Ophthalmol 33:620–628
Markowitz SN, Reyes SV (2013) Microperimetry and clinical practice: an evidence-based review. Can J Ophthalmol 48:350–357
Molina-Martín A, Piñero DP, Pérez-Cambrodí RJ (2015) Decreased perifoveal sensitivity detected by microperimetry in patients using hydroxychloroquine and without visual field and fundoscopic anomalies. J Ophthalmol 2015:10–13
Tarita-Nistor L, González EG, Markowitz SN, Steinbach SM (2008) Fixation characteristics of patients with macular degeneration recorded with the mp-1 microperimeter. Retina 28:125–133
Montesano G, Gervasoni A, Ferri P et al (2017) Structure-function relationship in early diabetic retinopathy: a spatial correlation analysis with OCT and microperimetry. Eye 31:931–939
Sanchez-Dalmau B, Martinez-Lapiscina EH, Torres-Torres R et al (2018) Early retinal atrophy predicts long-term visual impairment after acute optic neuritis. Mult Scler J 24:1196–1204
Molina A, Pérez-Cambrodí RJ, Ruiz-Fortes P, Laria C, Piñero DP (2013) Utility of microperimetry in nystagmus: a case report. Can J Ophthalmol 48:103–105
Molina-Martín A, Piñero DP, Pérez-Cambrodí RJ (2015) Fixation pattern analysis with microperimetry in nystagmus patients. Can J Ophthalmol 50:413–421
Martín AM, Piñero DP, Pérez-Cambrodí RJ (2017) Normal values for microperimetry with the MAIA microperimeter: sensitivity and fixation analysis in healthy adults and children. Eur J Ophthalmol 27:607–613
Ioyleva E, Krivosheeva M (2015) Microperimetry in the diagnosis of the first manifestation of optic neuritis in multiple sclerosis. J Neurol Sci 357(2015):e47
Romano MR, Angi M, Romano F (2007) Macular sensitivity change in multiple sclerosis followed with microperimetry. Eur J Ophthalmol 17:441–444
Mañago MM, Schenkman M, Berliner J, Hebert JR (2017) Gaze stabilization and dynamic visual acuity in people with multiple sclerosis. J Vestib Res 26(5–6):469–477
Subramanian PS (2018) Fixation instability: a new measure of neurologic dysfunction in multiple sclerosis. Invest Opthalmol Vis Sci 59:202
Mallery RM, Poolman P, Thurtell MJ et al (2018) Visual fixation instability in multiple sclerosis measured using SLO-OCT. Invest Opthalmol Vis Sci 59:196
Nij Bijvank JA, Petzold A, Coric D et al (2019) Quantification of visual fixation in multiple sclerosis. Invest Opthalmol Vis Sci 60:1372
Krupp LB, Alvarez LA, LaRocca NG, Scheinberg LC (1988) Fatigue in multiple sclerosis. Arch Neurol 45:435–437
Lima VC, Prata TS, De Moraes CGV et al (2010) A comparison between microperimetry and standard achromatic perimetry of the central visual field in eyes with glaucomatous paracentral visual-field defects. Br J Ophthalmol 94:64–67
Cennamo G, Romano MR, Vecchio EC et al (2016) Anatomical and functional retinal changes in multiple sclerosis. Eye (Lond) 30:456–462
Bsteh G, Hegen H, Altmann P et al (2020) Validation of inter-eye difference thresholds in optical coherence tomography for identification of optic neuritis in multiple sclerosis. Mult Scler Relat Disord 45:102403
Davion JB, Lopes R, Drumez É et al (2020) Asymptomatic optic nerve lesions: an underestimated cause of silent retinal atrophy in MS. Neurology 94:2468–2478
Khalil DH, Said MM, Abdelhakim MASE, Labeeb DM (2017) OCT and visual field changes as useful markers for follow-up of axonal loss in multiple sclerosis in Egyptian patients. Ocul Immunol Inflamm 25:315–322
Raz N, Chokron S, Ben-Hur T, Levin N (2013) Temporal reorganization to overcome monocular demyelination. Neurology 81:702–709
Funding
The author David P Piñero has been supported by the Ministry of Economy, Industry and Competitiveness of Spain within the program Ramón y Cajal, RYC-2016-20471. No additional funding was received for the performance of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of the University of Valencia (Valencia, Spain) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclosure
The authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gil-Casas, A., Piñero Llorens, D.P. & Molina-Martin, A. Ocular fixation and macular integrity by microperimetry in multiple sclerosis. Graefes Arch Clin Exp Ophthalmol 259, 157–164 (2021). https://doi.org/10.1007/s00417-020-04948-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04948-6