Abstract
Purpose
To demonstrate whether pars plana vitrectomy (PPV) changes the progression of dry age-related macular degeneration (AMD) by assessing longitudinal changes in drusen volume over follow-up.
Methods
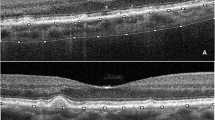
Dry AMD patients who had undergone unilateral PPV for symptomatic vitreomacular disorders were evaluated for the progression of disease by spectral domain-optical coherence tomography (SD-OCT) features including drusen volume, development of geographic atrophy, or choroidal neovascularization during follow-up. Drusen volume was manually calculated using an image processing software (ImageJ, NIH) on raster SD-OCT scans. Mean change in drusen volume of surgery eyes was compared with values of the fellow eyes of the same subjects (control group).
Results
Among 183 eyes with both vitreoretinal disorder and dry AMD, 48 eyes of 24 patients met the inclusion criteria and were included. The mean drusen volume change during a mean of 25.49 ± 23.35 months of follow-up (range: 6.00–86.87 months) was 4.236.899 ± 20.488.913 μm3 in the study eye and 7.796.357 ± 34.798.519 μm3 in the fellow eye (p = 0.297). Best-corrected visual acuity (BCVA) significantly increased from 0.40 ± 0.18 logMAR (≈ 20/50 Snellen equivalent) to 0.32 ± 0.31 (≈ 20/41 Snellen equivalent) after surgery (p = 0.012) in the study group while BCVA remained stable in the control group (0.19 ± 0.34 logMAR [≈ 20/30 Snellen equivalent] at baseline and 0.20 ± 0.31 logMAR [≈ 20/31 Snellen equivalent], p = 0.432). Choroidal neovascularization developed in 1 vitrectomized eye (4.54%) and in 1 eye (4.54%) from the control group during follow-up.
Conclusion
Vitrectomy did not seem to worsen dry AMD progression; even more visual acuity may improve despite a slight increase in drusen volume following surgery.



Similar content being viewed by others
References
Congdon N, O’Colmain B, Klaver CC et al (2004) Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 122:477–485
Klein R, Klein BE, Knudtson MD, Meuer SM, Swift M, Gangnon RE (2007) Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology 114:253–262
Smith W, Assink J, Klein R et al (2001) Risk factors for age-related macular degeneration: pooled findings from three continents. Ophthalmology 108:697–704
Ziada J, Hagenau F, Compera D et al (2018) Vitrectomy for intermediate age-related macular degeneration associated with tangential vitreomacular traction: a clinicopathologic correlation. Retina 38:531–540
Ciulla TA, Ying GS, Maguire MG et al (2015) Influence of the vitreomacular interface on treatment outcomes in the comparison of age-related macular degeneration treatments trials. Ophthalmology 122:1203–1211
Maggio E, Polito A, Guerriero M, Prigione G, Parolini B, Pertile G (2017) Vitreomacular adhesion and the risk of neovascular age-related macular degeneration. Ophthalmology 124:657–666
Krishnan R, Arora R, De Salvo G et al (2015) Vitreomacular traction affects anti-vascular endothelial growth factor treatment outcomes for exudative age-related macular degeneration. Retina 35:1750–1756
Kimura S, Morizane Y, Toshima S et al (2016) Efficacy of vitrectomy and inner limiting membrane peeling in age-related macular degeneration resistant to anti-vascular endothelial growth factor therapy, with vitreomacular traction or epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 254:1731–1736
Obeid A, Ali FS, Deaner JD, Gao X, Hsu J, Chiang A (2018) Outcomes of pars plana vitrectomy for epiretinal membrane in eyes with coexisting dry age-related macular degeneration. Ophthalmol Retina 2:765–770
Roller AB, Mahajan VB, Boldt HC, Abramoff MD, Russell SR, Folk JC (2010) Effects of vitrectomy on age-related macular degeneration. Ophthalmology 117:1381–1386
Abdelfattah NS, Zhang H, Boyer DS et al (2016) Drusen volume as a predictor of disease progression in patients with late age-related macular degeneration in the fellow eye. Invest Ophthalmol Vis Sci 57:1839–1846
Schlanitz FG, Baumann B, Kundi M et al (2017) Drusen volume development over time and its relevance to the course of age-related macular degeneration. Br J Ophthalmol 101:198–203
Folgar FA, Yuan EL, Sevilla MB et al (2016) Drusen volume and retinal pigment epithelium abnormal thinning volume predict 2-year progression of age-related macular degeneration. Ophthalmology 123:39–50
Freeman SR, Kozak I, Cheng L et al (2010) Optical coherence tomography-raster scanning and manual segmentation in determining drusen volume in age-related macular degeneration. Retina 30:431–435
Thiele S, Nadal J, Fleckenstein M et al (2018) Longitudinal analysis of drusen volume in intermediate age-related macular degeneration using two spectral-domain optical coherence tomography scan patterns. Ophthalmologica 239:110–120
Funding
This research is supported in part by NIH grant R01 EY016323-09A1 (D.U.B.), a core grant from the National Eye Institute P30 EY022589, and an unrestricted grant from Research to Prevent Blindness, NY (WRF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The University of California, San Diego Institutional Review Board approval was acquired for the review and analysis of patients’ medical records. The study adhered to the tenets of the Declaration of Helsinki for research involving human subjects and complied with Health Insurance Portability and Accountability Act (HIPAA) regulations.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Disclaimer
The funding organizations had no role in the design or conduct of this research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muftuoglu, I.K., Lin, T., Bartsch, DU. et al. Influence of vitrectomy on the progression of dry age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 259, 847–853 (2021). https://doi.org/10.1007/s00417-020-04943-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04943-x