Abstract
Purpose
To describe the clinical outcomes of Descemet membrane endothelial keratoplasty combined with phacoemulsification/posterior chamber intraocular lens implantation (triple procedure) for treatment of corneal decompensation induced by a phakic anterior chamber intraocular lens (AC IOL) implantation.
Methods
Ten patients (10 eyes) with corneal decompensation due to phakic AC IOL implantation that had undergone the triple procedure were included in this study. Among the 10 eyes, 5 eyes underwent explantation of AC IOL prior to the transplantation, and then underwent the triple procedure. The remaining 5 eyes with a phakic AC IOL in situ underwent the triple procedure with concurrent explantation of AC IOL. Corrected distance visual acuity (CDVA), subjective refraction, endothelial cell density (ECD), and complications were documented.
Results
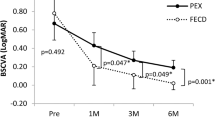
The triple procedure was performed across all eyes without any adverse events. The average CDVA improved from 1.32 ± 0.24 preoperatively to 0.15 ± 0.05 logarithm of the minimum angle of resolution (logMAR), which represents an improvement in Snellen equivalent from 20/400 (0.05) preoperatively to 20/28 (0.71) at 12 months after surgery. At 12 months, all eyes reached a CDVA of 20/32 (0.63) or better, and 50% of eyes reached a CDVA of 20/25 (0.8) or better. The mean donor ECD±SD was 2868.7 ± 67.9 cells/mm2, which decreased to 1724.1 ± 84.6 cells/mm2 at 12 months, representing 39.9% of endothelial cell loss. Patients did not experience any severe adverse events.
Conclusion
The triple procedure is a safe and effective option for corneal decompensation induced by a phakic AC IOL implantation, helping achieve a satisfactory visual rehabilitation with few complications.




Similar content being viewed by others
References
Huang D, Schallhorn SC, Sugar A, Farjo AA, Majmudar PA, Trattler WB, Tanzer DJ (2009) Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology 116:2244–2258
Dick HB, Budo C, Malecaze F, Güell JL, Marinho AA, Nuijts RM, Luyten GP, Menezo JL, Kohnen T (2009) Foldable Artiflex phakic intraocular lens for the correction of myopia: two-year follow-up results of a prospective European multicenter study. Ophthalmology 116:671–677
Alio JL, Peña-García P, Pachkoria K, Alio JL, EI Aswad A (2013) Intraocular optical quality of phakic intraocular lenses: comparison of angle-supported, iris-fixated, and posterior chamber lenses. Am J Ophthalmol 156:789–799
Guerra MG, Silva AMM, Marques SHM, Melo SH, Póvoa JA, Lobo C, Murta JN (2017) Phakic intraocular lens implantation: refractive outcome and safety in patients with anterior chamber depth between 2.8 and 3.0 versus ≥3.0 mm. Ophthalmic Res 57:239–246
Pechméja J, Guinguet J, Colin J, Binder PS (2012) Severe endothelial cell loss with anterior chamber phakic intraocular lenses. J Cataract Refract Surg 38:1288–1292
Bouheraoua N, Bonnet C, Labbé A, Sandali O, Lecuen N, Ameline B, Borderie V, Laroche L (2015) Iris-fixated phakic intraocular lens implantation to correct myopia and a predictive model of endothelial cell loss. J Cataract Refract Surg 41:2450–2457
Shajari M, Scheffel M, Koss MJ, Kohnen T (2016) Dependency of endothelial cell loss on anterior chamber depth within first 4 years after implantation of iris-supported phakic intraocular lenses to treat high myopia. J Cataract Refract Surg 42:1562–1569
Jonker SMR, Berendschot TTJM, Ronden AE, Saelens IEY, Bauer NJC, Nuijts RMMA (2018) Five year endothelial cell loss after implantation with Artiflex myopia and Artiflex toric phakic intraocular lenses. Am J Ophthalmol 194:110–119
Kohnen T, LaFontaine L, Andrew R (2017) Long–term safety follow-up of an anterior chamber angle-supported phakic intraocular lens. J Cataract Refract Surg 43:1163–1170
Kim M, Kim JK, Lee HK (2008) Corneal endothelial decompensation after iris-claw phakic intraocular lens implantation. J Cataract Refract Surg 34:517–519
Sikder S, Patel V, Holz HA, Mifflin MD, Davis S, Moshirfar M (2011) Management of corneal endothelial decompensation caused by iris-fixated phakic intraocular lenses with Descemet stripping automated endothelial keratoplasty. Cornea 30:1045–1047
Liarakos VS, Ham L, Dapena I, Tong CM, Quilendrino R, Yeh RY, Melles GR (2013) Endothelial keratoplasty for bullous keratopathy in eyes with an anterior chamber intraocular lens. J Cataract Refract Surg 39:1835–1845
Tannan A, Vo RC, Chen JL, Yu F, Deng SX, Aldave AJ (2015) Comparison of ACIOL retention with IOL exchange in patients undergoing Descemet stripping automated endothelial keratoplasty. Cornea 34:1030–1034
Wylegala E, Tarnawska D (2008) Management of pseudophakic bullous keratopathy by combined Descemet stripping endothelial keratoplasty and intraocular lens exchange. J Cataract Refract Surg 34:1708–1714
Sáles CS, Terry MA, Veldman PB, Mayko ZM, Straiko MD (2016) Relationship between tissue unscrolling time and endothelial cell loss. Cornea 35:471–476
Hamzaoglu EC, Straiko MD, Mayko ZM, Sáles CS, Terry MA (2015) The first 100 eyes of standardized Descemet stripping automated endothelial keratoplasty versus standardized Descemet membrane endothelial keratoplasty. Ophthalmology 122:2193–2199
Terry MA, Straiko MD, Veldman PB, Talajic JC, VanZyl C, Sales CS, Mayko ZM (2015) Standardized DMEK technique: reducing complications using prestripped tissue, novel glass injector, and sulfur hexafluoride (SF6) gas. Cornea 34:845–852
Schlögl A, Tourtas T, Kruse FE, Weller JM (2016) Long-term clinical outcome after Descemet membrane endothelial keratoplasty. Am J Ophthalmol 169:218–226
Coullet J, Mahieu L, Malecaze F, Fournié P, Leparmentier A, Moalic S, Arne JL (2007) Severe endothelial cell loss following uneventful angle-supported phakic intraocular lens implantation for high myopia. J Cataract Refract Surg 33:1477–1481
Saxena R, Boekhoom SS, Mulder PGH, Noordzij B, van Rij G, Luyten GP (2008) Long-term follow-up of endothelial cell change after Artisan phakic intraocular lens implantation. Ophthalmology 115:608–613
Coli A, Price FW, Whitson WE (1993) Intraocular lens exchange for anterior chamber intraocular lens-induced corneal endothelial damage. Ophthalmology 100:384–393
Fernandez-Vega L, Alfonso JF, Villacampa T (2003) Clear lens extraction for the correction of high myopia. Ophthalmology 110:2349–2354
Pucci V, Morselli S, Romanelli F, Pignatto S, Scandellari F, Bellucci R (2001) Clear lens phacoemulsification for correction of high myopia. J Cataract Refract Surg 27:896–900
Arne JL (2004) Phakic intraocular lens implantation versus clear lens extraction in highly myopic eyes of 30- to 50-year-old patients. J Cataract Refract Surg 30:2092–2096
Horgan N, Condon PI, Beatty S (2005) Refractive lens exchange in high myopia: long term follow up. Br J Ophthalmol 89:670–672
Colin J, Robinet A, Cochener B (1999) Retinal detachment after clear lens extraction for high myopia. Ophthalmology 106:2281–2285
Hole HA, Meyer JJ, Espandar L, Tabin GC, Mifflin MD, Moshirfar M (2008) Corneal profile analysis after Descemet stripping endothelial keratoplasty and its relationship to postoperative hyperopic shift. J Cataract Refract Surg 34:211–214
Funding
This work was supported by the National Natural Science Foundation of China (grant number 81870628).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This study adhered to the tenets of the Declaration of Helsinki. The Ethics Committee of Zhongshan Ophthalmic Center (Guangzhou, China) approved the study protocol.
Consent to participate
Written informed consent forms for research participation were signed by all participants prior to surgery.
Consent for publication
Written informed consent forms for research participation were signed by all participants prior to surgery.
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, T., Wu, J., Dong, X. et al. Descemet membrane endothelial keratoplasty for corneal decompensation caused by a phakic anterior chamber intraocular lens implantation. Graefes Arch Clin Exp Ophthalmol 258, 2761–2766 (2020). https://doi.org/10.1007/s00417-020-04928-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04928-w