Abstract
Purpose
To investigate the prognostic factors and visual outcomes for patients with epiretinal membrane after pars plana vitrectomy and possible interactions between multiple factors.
Methods
A retrospective chart review of adult patients with epiretinal membrane treated with pars plana vitrectomy performed by a single surgeon between February 1, 2015, and January 31, 2017 was conducted. The surgical procedures included standard 25-gauge vitrectomy with peeling of the epiretinal membrane and internal limiting membrane (ILM). Factors including age, sex, vision, intraocular pressure (IOP), lens status, and baseline optical coherence tomography angiography were analyzed to determine any association with visual outcomes. IOP and lens status were evaluated at every visit point and were used for analysis.
Results
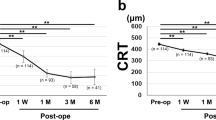
Visual changes after pars plana vitrectomy in patients with epiretinal membrane were significantly associated with time, lens status, baseline ellipsoid zone integrity, baseline vision, baseline parafoveal vessel density of superficial capillary plexus (SPVD), and IOP. Further investigation using Johnson-Neyman analysis revealed that vision improved over time, especially in pseudophakic eyes. High IOP at baseline or during follow-up was identified as a significant factor associated with limited visual improvement.
Conclusion
Our study showed that vision improved over time after vitrectomy for patients with epiretinal membrane. The surgical outcomes are more stable in pseudophakic eyes, and vision improved after cataract extraction in phakic eyes. IOP should be managed and monitored closely to optimize surgical and visual outcomes in patients.







Similar content being viewed by others
References
Dupas B, Tadayoni R, Gaudric A (2015) Epiretinal membranes. J Fr d’ophtalmologie 38:861–875
Inoue M, Kadonosono K (2014) Macular diseases: epiretinal membrane. Dev Ophthalmol 54:159–163
Iuliano L, Fogliato G, Gorgoni F, Corbelli E, Bandello F, Codenotti M (2019) Idiopathic epiretinal membrane surgery: safety, efficacy and patient related outcomes. Clin Ophthalmol 13:1253–1265
Schechet SA, DeVience E, Thompson JT (2017) The effect of internal limiting membrane peeling on idiopathic epiretinal membrane surgery, with a review of the literature. Retina. 37:873–880. https://doi.org/10.1097/IAE.0000000000001263
Fernandes TF, Sousa K, Azevedo I, Gouveia P, Calvão-Santos G, Gomes N, Falcão M (2020) Baseline visual acuity and interdigitation zone as predictors in idiopathic epiretinal membranes: a retrospective cohort study. Eur J Ophthalmol 8:1120672120932094. https://doi.org/10.1177/1120672120932094
Zur D, Iglicki M, Feldinger L, Schwartz S, Goldstein M, Loewenstein A, Barak A (2018) Disorganization of retinal inner layers as a biomarker for idiopathic epiretinal membrane after macular surgery-the DREAM study. Am J Ophthalmol 196:129–135. https://doi.org/10.1016/j.ajo.2018.08.037
Elhusseiny AM, Flynn HW Jr, Smiddy WE (2020) Long-term outcomes after idiopathic epiretinal membrane surgery. Clin Ophthalmol 14:995–1002. https://doi.org/10.2147/OPTH.S242681 eCollection 2020
Kim YJ, Kim S, Lee JY, Kim JG, Yoon YH (2018) Macular capillary plexuses after epiretinal membrane surgery: an optical coherence tomography angiography study. Br J Ophthalmol 102:1086–1091. https://doi.org/10.1136/bjophthalmol-2017-311188
Chen H, Chi W, Cai X, Deng Y, Jiang X, Wei Y, Zhang S (2019) Macular microvasculature features before and after vitrectomy in idiopathic macular epiretinal membrane: an OCT angiography analysis. Eye (Lond) 33(4):619–628. https://doi.org/10.1038/s41433-018-0272-3
Rommel F, Brinkmann MP, Sochurek JAM, Prasuhn M, Grisanti S, Ranjbar M (2020) Ocular blood flow changes impact visual acuity gain after surgical treatment for idiopathic epiretinal membrane. J Clin Med 9:E1768. https://doi.org/10.3390/jcm9061768
Chang S (2006) LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol 141:1033–1043
Fujikawa M, Sawada O, Kakinoki M et al (2014) Long-term intraocular pressure changes after vitrectomy for epiretinal membrane and macular hole. Graefes Arch Clin Exp Ophthalmol 252:389–393
Yu AL, Brummeisl W, Schaumberger M et al (2010) Vitrectomy does not increase the risk of open-angle glaucoma or ocular hypertension—a 5-year follow-up. Graefes Arch Clin Exp Ophthalmol 248:1407–1414
Tognetto D, Pastore MR, Cirigliano G, D’Aloisio R, Borelli M, De Giacinto C (2019) Long-term intraocular pressure after uncomplicated pars plana vitrectomy for idiopathic epiretinal membrane. Retina. 39:163–171. https://doi.org/10.1097/IAE.0000000000001933
Barbazetto IA, Liang J, Chang S et al (2004) Oxygen tension in the rabbit lens and vitreous before and after vitrectomy. Exp Eye Res 78:917–924
Holekamp NM, Shui YB, Beebe DC (2005) Vitrectomy surgery increases oxygen exposure to the lens: a possible mechanism for nuclear cataract formation. Am J Ophthalmol 139:302–310
Spaide RF, Klancnik JM, Cooney MJ (2015) Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol 133:45–50
Gregori NZ, Feuer W, Rosenfeld PJ (2010) Novel method for analyzing Snellen visual acuity measurements. Retina. 30:1046–1050
Zeger SL, Liang K-Y, Albert PS (1988) Models for longitudinal data: a generalized estimating equation approach. Biometrics 44:1049–1060
Shin HJ, Lee SH, Chung H, Kim HC (2012) Association between photoreceptor integrity and visual outcome in diabetic macular edema. Graefes Arch Clin Exp Ophthalmol 250:61–70
Sheu SJ, Lee YY, Horng YH, Lin HS, Lai WY, Tsen CL (2018) Characteristics of diabetic macular edema on optical coherence tomography may change over time or after treatment. Clin Ophthalmol 12:1887–1893
Banaee T, Singh RP, Champ K, Conti FF, Wai K, Bena J, Beven L, Ehlers JP (2018) Ellipsoid zone mapping parameters in retinal vein occlusive disease with associated macular edema. Ophthalmol Retina 2:836–841
Do DV, Gichuhi S, Vedula SS, Hawkins BS (2013) Surgery for post-vitrectomy cataract. Cochrane Database Syst Rev 12:CD006366
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Kaohsiung Veterans General hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Since this research was retrospective in design using already existing information, patients’ informed consent was waived.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, GC., Lin, HS., Horng, YH. et al. Intraocular pressure might play a role in the surgical management of patients with epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 258, 2691–2699 (2020). https://doi.org/10.1007/s00417-020-04870-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04870-x