Abstract
Purpose
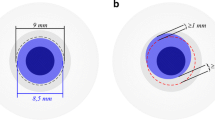
Unfolding and attachment of the posterior donor lamella may be the most challenging part in Descemet membrane endothelial keratoplasty (DMEK) procedure. We investigated the correlation of the difficulty degrees of this step to the postoperative clinical outcome 6 years after surgery.
Methods
One hundred sixty-nine consecutive DMEKs between September 2012 and August 2013 at the Charité–University Medicine Berlin were graded prospectively into 4 groups according to their grade of difficulty in unfolding and attachment of the graft lamella. Postoperative visual acuity, endothelial cell density, and rate of graft failure were measured after 1 year, after 2 years, and after 6 years and analyzed according to their grading group.
Results
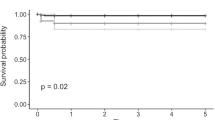
Visual acuity improved significantly in all groups and did not differ significantly between the grading groups at any time point postoperatively. There was a significant decrease of endothelial cell density in all groups with a significantly higher endothelial cell loss in group IV compared with the other groups within the first 24 months after surgery. The graft failure rate was significantly higher in eyes graded III and IV than in groups I and II (p = 0.012).
Conclusion
Although the endothelial cell loss and the graft failure rate increase significantly with a more difficult graft unfolding and attachment, DMEK surgery is a promising procedure with a good long-term postoperative outcome. A direct manipulation of the graft lamella for unfolding and centering by cannula or forceps should be avoided if possible to reduce the risk of an increased endothelial cell loss and a higher graft failure rate.
Trial registration
NCT02020044




Similar content being viewed by others
Data availability
The authors have full control of all primary data and agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review data upon request.
References
Melles GR, Wijdh RH, Nieuwendaal CP (2004) A technique to excise the Descemet membrane from a recipient cornea (descemetorhexis). Cornea 23(3):286–288
Price FW Jr, Price MO (2006) Descemet’s stripping with endothelial keratoplasty in 200 eyes: Early challenges and techniques to enhance donor adherence. J Cataract Refract Surg 32:411–418
Melles GR, Ong TS, Ververs B, van der Wees J (2006) Descemet membrane endothelial keratoplasty (DMEK). Cornea 25:987–990
Melles GR, Ong TS, Ververs B, van der Wees J (2008) Preliminary clinical results of Descemet membrane endothelial keratoplasty. Am J Ophthalmol 145(2):222–227
Heinzelmann S, Hüther S, Böhringer D, Eberwein P, Reinhard T, Maier P (2014) Influence of donor characteristics on Descemet membrane endothelial keratoplasty. Cornea 33(6):644–648
Maier AK, Gundlach E, Schroeter J, Klamann MK, Gonnermann J, Riechardt AI, Bertelmann E, Joussen AM, Torun N (2015) Influence of the difficulty of graft unfolding and attachment on the outcome in Descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol 253(6):895–900
Gerber-Hollbach N, Baydoun L, López EF, Frank LE, Dapena I, Liarakos VS, Schaal SC, Ham L, Oellerich S, Melles GRJ (2017) Clinical outcome of rebubbling for graft detachment after Descemet membrane endothelial keratoplasty. Cornea 36(7):771–776
Dirisamer M, van Dijk K, Dapena I, Ham L, Oganes O, Frank LE, Melles GR (2012) Prevention and management of graft detachment in Descemet membrane endothelial keratoplasty. Arch Ophthalmol 130(3):280–291
Feng MT, Price MO, Miller JM, Price FW Jr (2014) Air reinjection and endothelial cell density in Descemet membrane endothelial keratoplasty: five-year follow-up. J Cataract Refract Surg 40(7):1116–1121
Joussen AM, Heussen FM, Joeres S, Llacer H, Prinz B, Rohrschneider K, Maaijwee KJ, van Meurs J, Kirchhof B (2006) Autologous translocation of the choroid and retinal pigment epithelium in age-related macular degeneration. Am J Ophthalmol 142(1):17–30
Schlögl A, Tourtas T, Kruse FE, Weller JM (2016) Long-term clinical outcome after descemet membrane endothelial keratoplasty. Am J Ophthalmol 169:218–226
Vasiliauskaitė I, Oellerich S, Ham L, Dapena I, Baydoun L, van Dijk K, Melles GRJ (2020) Descemet membrane endothelial keratoplasty: ten-year graft survival and clinical outcomes [published online ahead of print, 2020 Apr 10]. Am J Ophthalmol S0002-9394(20)30172-0. https://doi.org/10.1016/j.ajo.2020.04.005
Heindl LM, Bucher F, Caramoy A, Hos D, Matthaei M, Cursiefen C (2014) Safety of donor tissue preparation and use of descemetoschisis and torn tissue in Descemet membrane endothelial keratoplasty. Cornea 33(10):e7–e9
Lazaridis A, Fydanaki O, Giallouros E, Georgalas I, Kymionis G, Sekundo W, Droutsas K (2018) Recovery of corneal clarity after DMEK followed by rebubbling versus uneventful DMEK. Cornea 37(7):840–847
Marques RE, Guerra PS, Sousa DC, Gonçalves AI, Quintas AM, Rodrigues W (2019) DMEK versus DSAEK for Fuchs’ endothelial dystrophy: a meta-analysis. Eur J Ophthalmol 29(1):15–22
Stuart AJ, Romano V, Virgili G, Shortt AJ (2018) Descemet’s membrane endothelial keratoplasty (DMEK) versus Descemet’s stripping automated endothelial keratoplasty (DSAEK) for corneal endothelial failure. Cochrane Database Syst Rev 25(6):CD012097
Esquenazi S, Rand W (2010) Safety of DSAEK in patients with previous glaucoma filtering surgery. J Glaucoma 19:219–220
Schoenberg ED, Levin KH, Savetsky MJ et al (2013) Surgical outcomes of DSAEK in patients with prior Ahmed glaucoma drainage device placement. Eur J Ophthalmol 23:807–813
Karadag R, Aykut V, Esen F, Oguz H, Demirok A (2020) Descemet’s membrane endothelial keratoplasty in aphakic and vitrectomized eye. GMS Ophthalmol Cases 14(10):Doc02. https://doi.org/10.3205/oc000129
Chiang CC, Lin JM, Tsai YY (2013) Descemet’s stripping automated endothelial keratoplasty in abnormal anterior segment: scleral indentation technique to enhance donor adherence. Graefes Arch Clin Exp Ophthalmol 251(6):1557–1563
Acknowledgments
The authors thank Simone Baar and Dirk Scharf for technical support.
Funding
Anna-Karina B. Maier: Financial support was provided by the “Friedrich C. Luft” Clinical Scientist Pilot Program funded by Volkswagen Foundation and Charité Foundation. Enken Gundlach: Financial support was provided by the “Ernst und Bertha Grimmke Stiftung.” Daniel Pilger is a participant in the BIH-Charité Clinician Scientist Program funded by the Charité–University Medicine Berlin and the Berlin Institute of Health.
Author information
Authors and Affiliations
Contributions
Anna-Karina B. Maier, Necip Torun, and Antonia M. Joussen contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Enken Gundlach, Nadiya Spiller, Daniel Pilger, and Anna-Karina B. Maier. The first draft of the manuscript was written by Enken Gundlach and Anna-Karina B. Maier and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study followed the ethical standards of the Declaration of Helsinki. Institutional ethical approval was obtained by the Ethics Committee of the Charité–Universitätsmedizin Berlin (EA2/108/12) for this prospective study and clinical trial registration was performed (http://www.clinicaltrials.gov, NCT02020044).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Code availability
(Software application or custom code) SPSS, RRID:SCR_002865
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 12 kb).
Rights and permissions
About this article
Cite this article
Gundlach, E., Spiller, N., Pilger, D. et al. Impact of difficult unfolding and attachment of the graft lamella on the long-term outcome after Descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol 258, 2459–2465 (2020). https://doi.org/10.1007/s00417-020-04852-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04852-z