Abstract
Purpose
To determine the presence of sickle cell retinopathy and maculopathy and to identify associations between markers of hemolysis and systemic and ocular manifestations in children affected by sickle cell disease.
Methods
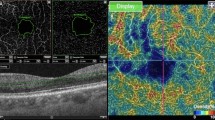
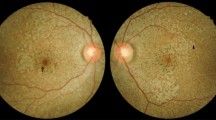
Eighteen children with sickle cell disease, aged 5–16 years, underwent complete eye examination including best-corrected visual acuity, slit-lamp biomicroscopy, ophthalmoscopy after pharmacological mydriasis, spectral-domain optical coherence tomography (SD-OCT), and optical coherence tomography angiography (OCTA). Blood test results and clinical history information were collected for each child, including fetal hemoglobin (HbF), hemoglobin (Hb), hematocrit (Htc), mean corpuscular volume (MCV), mean corpuscular hemoglobin concentration (MCHC), reticulocytes percentage (%ret), lactic dehydrogenase (LDH), total and direct bilirubin, glomerular filtration rate, number of painful crises, acute chest syndromes, and splenic sequestration. Therapeutic regimen and transfusion therapy were also evaluated.
Results
Sixteen of 36 eyes (44.4%) had non-proliferative sickle cell retinopathy on ophthalmoscopic evaluation. No patients had proliferative sickle cell retinopathy. In 13 of 36 eyes (36.1%), SD-OCT and OCTA detected signs of sickle cell maculopathy. Nine eyes (25%) presented sickle cell retinopathy and maculopathy, 7 eyes (19.4%) sickle cell retinopathy alone, and 4 eyes (11.1%) sickle cell maculopathy alone. A statistically significant association was found between sickle cell retinopathy; lower levels of HbF, Hb, and Htc; and higher MCV and percentage of reticulocytes. Sickle cell maculopathy was associated with lower values of H and Htc and higher levels of reticulocytes and total bilirubin.
Conclusions
We identified early signs of sickle cell retinopathy and maculopathy in a pediatric population with SD-OCT and OCTA. These two retinal complications were more frequent in children with higher hemolytic rates.






Similar content being viewed by others
References
Ribeiro MVMR, Jucá JVO, Alves ALCDS, Ferreira CVO, Barbosa FT, Ribeiro ÊAN (2017) Sickle cell retinopathy: a literature review. Rev Assoc Med Bras 63(12):1100–1103. https://doi.org/10.1590/1806-9282.63.12.1100
Minvielle W, Caillaux V, Cohen SY, Chasset F, Zambrowski O, Miere A, Souied EH (2016) Macular microangiopathy in sickle cell disease using optical coherence tomography angiography. Am J Ophthalmol 164:137–44.e1. https://doi.org/10.1016/j.ajo.2015.12.023
Rees DC, Williams TN, Gladwin MT (2010) Sickle-cell disease. Lancet 376(9757):2018–2031. https://doi.org/10.1016/S0140-6736(10)61029-X
Piel FB, Steinberg MH, Rees DC (2017) Sickle cell disease. N Engl J Med 376(16):1561–1573. https://doi.org/10.1056/NEJMra1510865
Kato GJ, Gladwin MT, Steinberg MH (2007) Deconstructing sickle cell disease: reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Rev 21(1):37–47. https://doi.org/10.1016/j.blre.2006.07.001
Pahl DA, Green NS, Bhatia M, Chen RWS (2017) New ways to detect pediatric sickle cell retinopathy: a comprehensive review. J Pediatr Hematol Oncol 39(8):618–625. https://doi.org/10.1097/MPH.0000000000000919
Emerson GG, Lutty GA (2005) Effects of sickle cell disease on the eye: clinical features and treatment. Hematol Oncol Clin North Am 19(5):957–973. https://doi.org/10.1016/j.hoc.2005.07.005
Grover S, Sambhav K, Chalam KV (2016) Capillary non perfusion by novel technology of OCT angiography in a patient with sickle cell disease with normal fluorescein angiogram. Eur J Ophthalmol 26(5):e121–e123. https://doi.org/10.5301/ejo.5000765
Han IC, Zhang AY, Liu TYA, Linz MO, Scott AW (2019) Utility of ultra-widefield retinal imaging for the staging and management of sickle cell retinopathy. Retina 39(5):836–843. https://doi.org/10.1097/IAE.0000000000002057
Goldberg MF (1971) Classification and pathogenesis of proliferative sickle retinopathy. Am J Ophthalmol 71(3):649–665. https://doi.org/10.1016/0002-9394(71)90429-6
Gill HS, Lam WC (2008) A screening strategy for the detection of sickle cell retinopathy in pediatric patients. Can J Ophthalmol 43(2):188–191. https://doi.org/10.3129/i08-003
Yawn BP, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, James AH, Jordan L, Lanzkron SM, Lottenberg R, Savage WJ, Tanabe PJ, Ware RE, Murad MH, Goldsmith JC, Ortiz E, Fulwood R, Horton A, John-Sowah J (2014) Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA 312(10):1033–1048. https://doi.org/10.1001/jama.2014.10517
Section on Hematology/Oncology Committee on Genetics; American Academy of Pediatrics (2002) Health supervision for children with sickle cell disease. Pediatrics 109(3):526–535. https://doi.org/10.1542/peds.109.3.526
Dell’Arti L, Barteselli G, Riva L, Carini E, Graziadei G, Benatti E, Invernizzi A, Cappellini MD, Viola F (2018) Sickle cell maculopathy: identification of systemic risk factors, and microstructural analysis of individual retinal layers of the macula. PLoS One 13(3):e0193582. https://doi.org/10.1371/journal.pone.0193582
Pahl DA, Green NS, Bhatia M, Lee MT, Chang JS, Licursi M, Briamonte C, Smilow E, Chen RWS (2017) Optical coherence tomography angiography and ultra-widefield fluorescein angiography for early detection of adolescent sickle retinopathy. Am J Ophthalmol 183:91–98. https://doi.org/10.1016/j.ajo.2017.08.010
Chow CC, Genead MA, Anastasakis A, Chau FY, Fishman GA, Lim JI (2011) Structural and functional correlation in sickle cell retinopathy using spectral-domain optical coherence tomography and scanning laser ophthalmoscope microperimetry. Am J Ophthalmol 152(4):704–711.e2. https://doi.org/10.1016/j.ajo.2011.03.035
Associazione Italiana Ematologia Oncologia Pediatrica (2012) Linee-guida per la gestione della malattia drepanocitica in età pediatrica in Italia. http://www.aieop.org/web/wp-content/uploads/2017/05/tutto-giu12.pdf. Accessed 18 February 2020
Do BK, Rodger DC (2017) Sickle cell disease and the eye. Curr Opin Ophthalmol 28(6):623–628. https://doi.org/10.1097/ICU.0000000000000423
Rosenberg JB, Hutcheson KA (2011) Pediatric sickle cell retinopathy: correlation with clinical factors. J AAPOS 15(1):49–53. https://doi.org/10.1016/j.jaapos.2010.11.014
Eruchalu UV, Pam VA, Akuse RM (2006) Ocular findings in children with severe clinical symptoms of homozygous sickle cell anaemia in Kaduna, Nigeria. West Afr J Med 25(2):88–91 Retrieved from https://www.canadianjournalofophthalmology.ca/. Accessed 5 September 2019
Tantawy AA, Andrawes NG, Adly AA, El Kady BA, Shalash AS (2013) Retinal changes in children and adolescents with sickle cell disease attending a paediatric hospital in Cairo, Egypt: risk factors and relation to ophthalmic and cerebral blood flow. Trans R Soc Trop Med Hyg 107(4):205–211. https://doi.org/10.1093/trstmh/trt008
Akinsola FB, Kehinde MO (2004) Ocular findings in sickle cell disease patients in Lagos. Niger Postgrad Med J 11(3):203–206 Retrieved from http://www.npmj.org/. Accessed 5 September 2019
Cho M, Kiss S (2011) Detection and monitoring of sickle cell retinopathy using ultra wide-field color photography and fluorescein angiography. Retina 31(4):738–747. https://doi.org/10.1097/IAE.0b013e3181f049ec
Leitão Guerra RL, Leitão Guerra CL, Bastos MG, de Oliveira AHP, Salles C (2019) Sickle cell retinopathy: what we now understand using optical coherence tomography angiography. a systematic review. Blood Rev 35:32–42. https://doi.org/10.1016/j.blre.2019.03.001
Han IC, Tadarati M, Scott AW (2015) Macular vascular abnormalities identified by optical coherence tomographic angiography in patients with sickle cell disease. JAMA Ophthalmol 133(11):1337–1340. https://doi.org/10.1001/jamaophthalmol.2015.2824
Han IC, Tadarati M, Pacheco KD, Scott AW (2017) Evaluation of macular vascular abnormalities identified by optical coherence tomography angiography in sickle cell disease. Am J Ophthalmol 177:90–99. https://doi.org/10.1016/j.ajo.2017.02.007
Jung JJ, Chen MH, Frambach CR, Rofagha S, Lee SS (2018) Spectral domain versus swept source optical coherence tomography angiography of the retinal capillary plexuses in sickle cell maculopathy. Retin Cases Brief Rep 12(2):87–92. https://doi.org/10.1097/ICB.0000000000000448
Fadugbagbe AO, Gurgel RQ, Mendonça CQ, Cipolotti R, dos Santos AM, Cuevas LE (2010) Ocular manifestations of sickle cell disease. Ann Trop Paediatr 30(1):19–26. https://doi.org/10.1179/146532810X12637745451870
Fox PD, Dunn DT, Morris JS, Serjeant GR (1990) Risk factors for proliferative sickle retinopathy. Br J Ophthalmol 74(3):172–176. https://doi.org/10.1136/bjo.74.3.172
Kato GJ, Steinberg MH, Gladwin MT (2017) Intravascular hemolysis and the pathophysiology of sickle cell disease. J Clin Invest 127(3):750–760. https://doi.org/10.1172/JCI89741
Author information
Authors and Affiliations
Contributions
Study conception and design were performed by S. Pignatto, M. Arigliani, and L. Grego. All authors contribute to material preparation and data collection and analysis. The first draft of the manuscript was written by L. Grego, and all authors commented and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
PL is a consultant for Bayer, CenterVue, Novartis Pharma AG, outside the submitted work. All authors, except PL, certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the regional ethics committee (CEUR) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from parents and tutors of all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grego, L., Pignatto, S., Alfier, F. et al. Optical coherence tomography (OCT) and OCT angiography allow early identification of sickle cell maculopathy in children and correlate it with systemic risk factors. Graefes Arch Clin Exp Ophthalmol 258, 2551–2561 (2020). https://doi.org/10.1007/s00417-020-04764-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04764-y