Abstract
Purpose
Diabetic macular edema (DME) is a major cause of vision loss. Diabetes patients with mild macular edema and good visual acuity are often observed carefully so that treatment can be instituted when central vision is threatened. Optimal frequency of monitoring of these patients is unknown. Our study aimed to gather more information to determine a safe interval for monitoring of patients with eyes that were not undergoing active treatment for DME and to correlate outcomes with clinical risk factors.
Methods
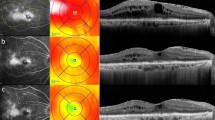
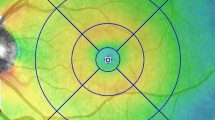
Study population: Ninety-seven eyes with optical coherence tomography (OCT) evidence of DME of 97 patients with diabetes. Study procedures: Retrospective review of medical records and macular OCT scans at a 6–12-month interval. Primary outcomes: Change in visual acuity and change in central subfield thickness (CSFT) between the initial and follow-up OCT scans.
Results
There was no significant change from median baseline visual acuity 6/9 (inter-quartile range 6/6–6/12) or from median baseline CSFT (290 μm, inter-quartile range 270–312 μm) over a median duration of 8 months (inter-quartile range 7–10 months). The numbers of eyes where CSFT had increased ≥ 25 μm, reduced ≥ 25 μm, or remained unchanged were 16 (16%), 6 (6%), and 74 (76%), respectively. Patients with hemoglobin A1c ≥ 8.5% were 5.7 times more likely to develop central subfield thickening (95% CI 1.1–30.1, P = 0.038).
Conclusions
Majority of eyes with DME on OCT had stable CSFT without treatment over a median duration of 8 months. Hemoglobin A1c may be useful for risk stratification.


Similar content being viewed by others
Abbreviations
- CSFT:
-
Central subfield thickness
- CSME:
-
Clinically significant macular edema
- DME:
-
Diabetic macular edema
- DR:
-
Diabetic retinopathy
- DRCR:
-
Diabetic Retinopathy Clinical Research
- ETDRS:
-
Early Treatment Diabetic Retinopathy Study
- HbA1c:
-
Hemoglobin A1c
- LogMAR:
-
Logarithm of the minimum angle of resolution
- OCT:
-
Optical coherence tomography
- VA:
-
Visual acuity
- VEGF:
-
Vascular endothelial growth factor
References
Das A, McGuire PG, Rangasamy S (2015) Diabetic macular edema: pathophysiology and novel therapeutic targets. Ophthalmology. 122(7):1375–1394
Johnson MW (2009) Etiology and treatment of macular edema. Am J Ophthalmol 147(1):11–21.e1
Mitchell P, Wong TY (2014) Management paradigms for diabetic macular edema. Am J Ophthalmol 157(3):505–13.e8
Browning DJ, Fraser CM (2008) The predictive value of patient and eye characteristics on the course of subclinical diabetic macular edema. Am J Ophthalmol 145(1):149–54. e3
Diabetic Retinopathy Clinical Research Network, Bressler NM, Miller KM, Beck RW, Bressler SB, Glassman AR et al (2012) Observational study of subclinical diabetic macular edema. Eye (Lond) 26(6):833–840
Tejerina AN, Vujosevic S, Varano M, Egan C, Sivaprasad S, Menon G et al (2015) One-year progression of diabetic subclinical macular edema in eyes with mild nonproliferative diabetic retinopathy: location of the increase in retinal thickness. Ophthalmic Res 54(3):118–123
Pires I, Santos AR, Nunes S, Lobo C, Cunha-Vaz J (2013) Subclinical macular edema as a predictor of progression to clinically significant macular edema in type 2 diabetes. Ophthalmologica. 230(4):201–206
Fiore T, Androudi S, Iaccheri B, Lupidi M, Fabrizio G, Fruttini D et al (2013) Repeatability and reproducibility of retinal thickness measurements in diabetic patients with spectral domain optical coherence tomography. Curr Eye Res 38(6):674–679
Klein R, Klein BEK, Moss SE, Cruickshanks KJ (1995) The Wisconsin epidemiologic study of diabetic retinopathy XV. Ophthalmology. 102(1):7–16
Klein R, Klein BEK, Moss SE, Davis MD, DeMets DL (1984) The Wisconsin epidemiologic study of diabetic retinopathy. Ophthalmology 91(12):1464–1474
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T et al (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35(3):556–564
Chew EY, Davis MD, Danis RP, Lovato JF, Perdue LH, Greven C et al (2014) The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes. Ophthalmology. 121(12):2443–2451
Hikichi T, Fujio N, Akiba J, Azuma Y, Takahashi M, Yoshida A (1997) Association between the short term natural history of diabetic macular edema and the Vitreomacular relationship in type II diabetes mellitus. Ophthalmology. 104(3):473–478
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the National Statement on Ethical Conduct in Research 2007, The Melbourne Health Quality Assurance/Negligible Risk Research Project, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
No informed consent was sought from patients in this study as only patient records that were accessible to medical professionals were obtained and collected for this study in a non-identifiable manner. In addition, no patient contact was required for this study, and outcomes for patients were not affected by the study due to its retrospective nature.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, H., Tan, M.H., Pomerleau, D. et al. Optical coherence tomography analysis of patients with untreated diabetic macular edema. Graefes Arch Clin Exp Ophthalmol 258, 653–661 (2020). https://doi.org/10.1007/s00417-019-04549-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04549-y