Abstract
Purpose
To determine the incidence of spontaneous regression of congenital corneal opacity (CCO) and identify clinical factors associated with the regression.
Methods
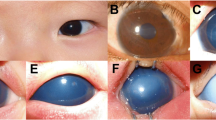
Medical records and anterior segment photographs were reviewed of 57 eyes in 35 patients with CCO that were not related to congenital glaucoma, tumors, infection, trauma, or metabolic disorders and were followed up without corneal transplantation for longer than one year at Seoul National University Hospital. Spontaneous regression of corneal opacity was defined as a decrease in corneal opacity significant enough for visual axis clearance. Data on demographics, systemic, and ocular characteristics were collected and compared between patients who had spontaneous regression of CCO and those who did not.
Results
Spontaneous regression of corneal opacity developed in 32 eyes (22 patients, 56.1%) out of 57 CCO eyes (35 patients) at the mean 8.2 ± 5.4 months of age (the median 6.7 months). Absence of combined ocular anomalies such as iris anomaly, lens opacity, and peripheral corneal vascularization was significantly associated with the regression of opacity.
Conclusions
Corneal opacity can spontaneously regress in 56.1% of eyes with CCO during the first year of life. Careful follow-up with amblyopia management can be one of treatment options for CCO.



Similar content being viewed by others
References
Bermejo E, Martinez-Frias ML (1998) Congenital eye malformations: clinical-epidemiological analysis of 1,124,654 consecutive births in Spain. Am J Med Genet 75:497–504
Kurilec JM, Zaidman GW (2014) Incidence of Peters anomaly and congenital corneal opacities interfering with vision in the United States. Cornea 33:848–850. https://doi.org/10.1097/ICO.0000000000000182
Vanathi M, Panda A, Vengayil S, Chaudhuri Z, Dada T (2009) Pediatric keratoplasty. Surv Ophthalmol 54:245–271. https://doi.org/10.1016/j.survophthal.2008.12.011
Huang C, O'Hara M, Mannis MJ (2009) Primary pediatric keratoplasty: indications and outcomes. Cornea 28:1003–1008. https://doi.org/10.1097/ICO.0b013e3181a186c0
Lowe MT, Keane MC, Coster DJ, Williams KA (2011) The outcome of corneal transplantation in infants, children, and adolescents. Ophthalmology 118:492–497. https://doi.org/10.1016/j.ophtha.2010.07.006
AlArrayedh H, Collum L, Murphy CC (2018) Outcomes of penetrating keratoplasty in congenital hereditary endothelial dystrophy. Br J Ophthalmol 102:19–25. https://doi.org/10.1136/bjophthalmol-2016-309565
Al-Ghamdi A, Al-Rajhi A, Wagoner MD (2007) Primary pediatric keratoplasty: indications, graft survival, and visual outcome. J AAPOS 11:41–47. https://doi.org/10.1016/j.jaapos.2006.09.012
Rao KV, Fernandes M, Gangopadhyay N, Vemuganti GK, Krishnaiah S, Sangwan VS (2008) Outcome of penetrating keratoplasty for Peters anomaly. Cornea 27:749–753. https://doi.org/10.1097/ICO.0b013e31816fe9a7
Yang LL, Lambert SR, Drews-Botsch C, Stulting RD (2009) Long-term visual outcome of penetrating keratoplasty in infants and children with Peters anomaly. J AAPOS 13:175–180. https://doi.org/10.1016/j.jaapos.2008.10.007
Lee HK, Kim MK, Oh JY (2018) Corneal abnormalities in congenital aniridia: congenital central corneal opacity verus aniridia-associated keratopathy. Am J Ophthalmol 185:75–80. https://doi.org/10.1016/j.ajo.2017.10.017
Kim YW, Choi HJ, Kim MK, Wee WR, Yu YS, Oh JY (2013) Clinical outcome of penetrating keratoplasty in patients 5 years or younger: peters anomaly versus sclerocornea. Cornea 32:1432–1436. https://doi.org/10.1097/ICO.0b013e31829dd836
Spierer O, Cavuoto KM, Suwannaraj S, McKeown CA, Chang TC (2018) Outcome of optical iridectomy in Peters anomaly. Graefes Arch Clin Exp Ophthalmol 256:1679–1683. https://doi.org/10.1007/s00417-018-4000-2
Yoshikawa H, Sotozono C, Ikeda Y, Mori K, Ueno M, Kinoshita S (2017) Long-term clinical course in eyes with Peters anomaly. Cornea 36:448–451. https://doi.org/10.1097/ICO.0000000000001161
Krachmer JH, Mannis MJ, Edward J (eds) (2017) Cornea. Elsevier Mosby, Philadelphia
Gupta N, Kalaivani M, Tandon R (2011) Comparison of prognostic value of Roper Hall and Dua classification systems in acute ocular burns. Br J Ophthalmol 95:194–198. https://doi.org/10.1136/bjo.2009.173724
Kim YJ, Jeoung JW, Kim MK, Park KH, Yu YS, Oh JY (2018) Clinical features and outcome of corneal opacity associated with congenital glaucoma. BMC Ophthalmol 18:190. https://doi.org/10.1186/s12886-018-0865-4
Jullienne R, Manoli P, Tiffet T, He Z, Rannou K, Thuret G, Gain P (2015) Corneal endothelium self-healing mathematical model after inadvertent descemetorhexis. J Cataract Refract Surg 41:2313–2318. https://doi.org/10.1016/j.jcrs.2015.10.043
Soh YQ, Peh G, George BL, Seah XY, Primalani NK, Adnan K, Mehta JS (2016) Predicative factors for corneal endothelial cell migration. Invest Ophthalmol Vis Sci 57:338–348. https://doi.org/10.1167/iovs.15-18300
Harwerth RS, Smith EL 3rd, Duncan GC, Crawford ML, von Noorden GK (1986) Multiple sensitive periods in the development of the primate visual system. Science 232:235–238. https://doi.org/10.1126/science.3952507
Zhu AY, Marquezan MC, Kraus CL, Prescott CR (2018) Pediatric corneal transplants: review of current practice patterns. Cornea 37:973–980. https://doi.org/10.1097/ICO.0000000000001613
Cowden JW (1990) Penetrating keratoplasty in infants and children. Ophthalmology 97:324–328. https://doi.org/10.1016/s0161-6420(90)32586-1
Nischal KK (2012) A new approach to the classification of neonatal corneal opacities. Curr Opin Ophthalmol 23:344–354. https://doi.org/10.1097/ICU.0b013e328356893d
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Seoul National University Hospital (IRB No. H-1810-029-977) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from guardians of all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Choe, S., Yoon, C.H., Kim, M.K. et al. Spontaneous regression of congenital corneal opacity. Graefes Arch Clin Exp Ophthalmol 258, 359–366 (2020). https://doi.org/10.1007/s00417-019-04526-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04526-5