Abstract
Purpose
To assess the global burden of glaucoma by year, age, sex, regions, socioeconomic development, and mean years of schooling (MYS) by using disability-adjusted life year (DALY), then to explore the health inequality with socioeconomic status in glaucoma.
Methods
Global, national, and regional DALY data of glaucoma by year, age, and sex were extracted from the Global Health Data Exchange. Human development index (HDI) and national MYS in 2015 were obtained from the Human Development Report (HDR) 2016. Mann-Whitney U test was performed to explore the sexual difference in global DALYs. Kruskal-Wallis tests were performed to explore the difference of age-standardized DALY rates across WHO regions and HDI-related country groups. Linear regression analyses were performed to explore the association between age-standardized DALY rates with HDI and MYS. Health-related Gini coefficients and concentration indexes were calculated to evaluate the trends in health inequality of glaucoma since 1990.
Results
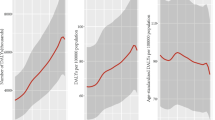
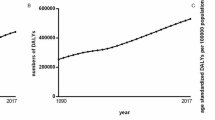
DALY numbers, crude DALY rates, and age-standardized DALY rates increased by 118.0%, 55.22%, and 12.12%, respectively, since 1990. Global DALY numbers and crude DALY rates increased with age, and Mann-Whitney U test revealed no significant sex difference in global DALY numbers (P = 0.807) and global crude DALYs rates (P = 0.976) for each age group in 2016. Africa and Eastern Mediterranean had higher age-standardized DALY rates than the global one in 2016. Kruskal-Wallis test indicated significant difference in age-standardized DALY rates across WHO regions (χ2 = 94.227, P < 0.001). Linear regression analysis indicated that HDI (adjusted R2 = 0.079; F = 16.722, P < 0.001) and MYS (adjusted R2 = 0.108; F = 23.048, P < 0.001) had a significant effect on age-standardized DALY rates. Gini coefficients rose from 0.290 in 1990 to 0.292 in 2015 with a peak value 0.299 in 2005, concentration index declined from 1990 (− 0.099) to 2000 (− 0.077) with reaching a low peak value, then rapidly increased to − 0.097 in 2015.
Conclusions
With population growth and aging, global burden of glaucoma is increasing and older age, lower socioeconomic status, and lower MYS are associated with higher glaucoma burden. Our results help to gain a better understanding of glaucoma and guide future health policies tailored for public.






Similar content being viewed by others
References
Weinreb RN, Aung T, Medeiros FA (2014) The pathophysiology and treatment of glaucoma: a review. JAMA 311(18):1901–1911. https://doi.org/10.1001/jama.2014.3192
Kingman S (2004) Glaucoma is second leading cause of blindness globally. Bull World Health Organ 82:887–888
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90(3):262–267. https://doi.org/10.1136/bjo.2005.081224
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY (2014) Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121(11):2081–2090. https://doi.org/10.1016/j.ophtha.2014.05.013
Hay SI, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, RS A (2017) Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016 a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1260–1344. https://doi.org/10.1016/S0140-6736(17)32130-X
Varma R, Lee PP, Goldberg I, Kotak S (2011) An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol 152(4):515–522. https://doi.org/10.1016/j.ajo.2011.06.004
Rein DB, Zhang P, Wirth KE, Lee PP, Hoerger TJ, McCall N, Klein R, Tielsch JM, Vijan S, Saaddine J (2006) The economic burden of major adult visual disorders in the United States. Arch Ophthalmol 124:1754–1760
Budenz DL, Barton K, Whiteside-de Vos J, Schiffman J, Bandi J, Nolan W, Herndon L, Kim H, Hay-Smith G, Tielsch JM, Tema Eye Survey Study G (2013) Prevalence of glaucoma in an urban West African population: the Tema Eye Survey. JAMA Ophthalmol 131(5):651–658. https://doi.org/10.1001/jamaophthalmol.2013.1686
Leite MT, Sakata LM, FA M (2011) Managing glaucoma in developing countries. Arq Bras Oftalmol 74(2):83–84
Sathyamangalam RV, Paul PG, George R, Baskaran M, Hemamalini A, Madan RV, Augustian J, Prema R, Lingam V (2009) Determinants of glaucoma awareness and knowledge in urban Chennai. Indian J Ophthalmol 57(5):355–360. https://doi.org/10.4103/0301-4738.55073
Ono K, Hiratsuka Y, A. M (2010) Global inequality in eye health country-level analysis from the Global Burden of Disease Study. Am J Public Health 100:1784–1788. https://doi.org/10.2105/AJPH.2009
Javitt JC (1995) Preventing blindness in Americans the need for eye health education. Surv Ophthalmol 40:41–44
United Nations Development Programme (2016) Human development report. Human Development for Everyone http://hdr.undp.org/en/2015-report/download. Accessed 20 May 2018
Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, RS A (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016 a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
Murray C (1994) Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ 72:429–445
Global Health Data Exchange. GBD results tool. http://ghdx.healthdata.org/gbd-results-tool. Accessed 20 May 2018
Global Health Data Exchange. Terms Defined http://www.healthdata.org/terms-defined. Accessed 20 May 2018
Bleichrodt H, van Doorslaer E (2006) A welfare economics foundation for health inequality measurement. J Health Econ 25(5):945–957. https://doi.org/10.1016/j.jhealeco.2006.01.002
Jin J, Wang JX, Ma XY, Wang YD, RY L (2015) Equality of medical health resource allocation in China based on the Gini coefficient method. Iran J Public Health 44(4):445–457
Wagstaff A (2002) Inequality aversion, health inequalities and health achievement. J Health Econ 21:627–641
Costa-Font J, Hernandez-Quevedo C (2012) Measuring inequalities in health: what do we know? What do we need to know? Health Policy 106(2):195–206. https://doi.org/10.1016/j.healthpol.2012.04.007
Wagstaff A, Doorslaer EV (1994) Measuring inequalities in health in the presence of multiple-category morbidity indicators. Health Econ 3:281–291
Nachar N (2008) The Mann-Whitney U a test for assessing whether two independent samples come from the same distribution. Tutor Quant Methods Psychol 4:13–20
Chan Y, RP. W (1997) Learning and understanding the Kruskal-Wallis one-way analysis-of-variance-by-ranks test for differences among three or more independent groups. Phys Ther 77:1755–1762
Schneider A, Hommel G, Blettner M (2010) Linear regression analysis: part 14 of a series on evaluation of scientific publications. Dtsch Arztebl Int 107(44):776–782. https://doi.org/10.3238/arztebl.2010.0776
Jolliffe D, Krushelnytskyy B (1999) Bootstrap standard errors for indices of inequality INEQERR. Stata Tech Bull 51(1):28–32
Chen Z, Roy K (2009) Calculating concentration index with repetitive values of indicators of economic welfare. J Health Econ 28(1):169–175. https://doi.org/10.1016/j.jhealeco.2008.09.004
Kakwani N, Wagstaff A, vD E (1997) Socioeconomic inequalities inhealth: measurement, computation, and statistical inference. J Econ 77:87–103
World Health Organization. Working with the regions. http://www.who.int/chp/about/regions/en/. Accessed 20 May 2018
Potancokova M, Samir K, Goujon A (2014) Global estimates of mean years of schooling a new methodology. IIASA Interim Report. http://pure.iiasa.ac.at/11261/. Accessed 20 May 2018
Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Resnikoff S, Taylor HR, Vision Loss Expert G (2013) Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health 1(6):e339–e349. https://doi.org/10.1016/S2214-109X(13)70113-X
Stevens GA, White RA, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Resnikoff S, Taylor H, Bourne RR, Vision Loss Expert G (2013) Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990-2010. Ophthalmology 120(12):2377–2384. https://doi.org/10.1016/j.ophtha.2013.05.025
Boyers LN, Karimkhani C, Hilton J, Richheimer W, Dellavalle RP (2015) Global burden of eye and vision disease as reflected in the Cochrane Database of Systematic Reviews. JAMA Ophthalmol 133(1):25–31. https://doi.org/10.1001/jamaophthalmol.2014.3527
Hatef E, Mohammadi S-F, Alinia C, Ashrafi E, S-Mehrdad Mohammadi LA, Sadeghi-Tari A (2016) National Burden of Eye Diseases in Iran, 1990–2010; findings from the Global Burden of Diseases Study 2010. Middle East Afr J Ophthalmol 23(1):89–95
Wang B, Congdon N, Bourne R, Li Y, Cao K, Zhao A, Yusufu M, Dong W, Zhou M, Wang N (2018) Burden of vision loss associated with eye disease in China 1990-2020: findings from the Global Burden of Disease Study 2015. Br J Ophthalmol 102(2):220–224. https://doi.org/10.1136/bjophthalmol-2017-310333
Freeman EE, Roy-Gagnon MH, Samson E, Haddad S, Aubin MJ, Vela C, Zunzunegui MV (2013) The global burden of visual difficulty in low, middle, and high income countries. PLoS One 8(5):e63315. https://doi.org/10.1371/journal.pone.0063315
Shweikh Y, Ko F, Chan MP, Patel PJ, Muthy Z, Khaw PT, Yip J, Strouthidis N, Foster PJ, Eye UKB, Vision C (2015) Measures of socioeconomic status and self-reported glaucoma in the U.K. Biobank cohort. Eye (Lond) 29(10):1360–1367. https://doi.org/10.1038/eye.2015.157
Pascolini D, Mariotti SP (2012) Global estimates of visual impairment: 2010. Br J Ophthalmol 96(5):614–618. https://doi.org/10.1136/bjophthalmol-2011-300539
Klimko PG, Sharif NA (2018) Discovery, characterization and clinical utility of prostaglandin agonists for the treatment of glaucoma. Br J Pharmacol. https://doi.org/10.1111/bph.14327
Li F, Huang W, Zhang X (2018) Efficacy and safety of different regimens for primary open-angle glaucoma or ocular hypertension: a systematic review and network meta-analysis. Acta Ophthalmol 96(3):e277–e284. https://doi.org/10.1111/aos.13568
Momont AC, Mills RP (2013) Glaucoma screening: current perspectives and future directions. Semin Ophthalmol 28(3):185–190. https://doi.org/10.3109/08820538.2013.771200
Saw S-M, Gazzard G, Friedman D, Foster PJ, Devereux JG, Wong ML (2003) Awareness of glaucoma, and health beliefs of patients suffering primary acute angle closure. Br J Ophthalmol 87:446–449
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, J., Yu, X., Ping, X. et al. Socioeconomic disparities in the global burden of glaucoma: an analysis of trends from 1990 to 2016. Graefes Arch Clin Exp Ophthalmol 258, 587–594 (2020). https://doi.org/10.1007/s00417-019-04484-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04484-y