Abstract
Purpose
To investigate retinal sensitivity in eyes with angioid streaks (AS).
Methods
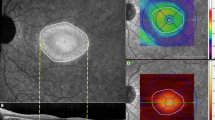
This study was a retrospective observational case series. A total of 13 eyes from 9 patients with AS underwent ophthalmologic examination, including fundus autofluorescence (FAF), spectral domain optical tomography (SD-OCT), and microperimetry. Retinal pigment epithelium (RPE) atrophy was assessed using FAF. Outer retinal atrophy, more specifically, disruption of the ellipsoid zone, was evaluated using SD-OCT images. The association between retinal sensitivity, RPE atrophy or outer retinal atrophy, and patient demographic characteristics or ophthalmologic findings were investigated.
Results
The mean area of outer retinal atrophy was 14.5 ± 12.9 mm2, significantly larger than the mean area of RPE atrophy (9.0 ± 9.0 mm2; P = 0.0028). The average retinal sensitivity in the area of RPE atrophy was 2.4 ± 5.6 dB, that in the area of outer retinal atrophy outside RPE atrophy was 14.6 ± 7.5 dB, and that in the area without any atrophy was 25.6 ± 5.1 dB. Reticular pseudodrusen (RPD) was observed in 5 eyes. Eyes with RPD showed a greater extent of both outer retinal atrophy and RPE atrophy than those without RPD and a greater decrease in mean retinal sensitivity.
Conclusions
In eyes with AS, especially in those with RPD, large areas of outer retinal atrophy and RPE atrophy were observed, and the retinal sensitivity in the areas was correspondingly decreased.





Similar content being viewed by others
References
Chatziralli I, Saitakis G, Dimitriou E, Chatzirallis A, Stoungioti S, Theodossiadis G, Theodossiadis P (2018) Angioid streaks: a comprehensive review from pathophysiology to treatment. Retina. https://doi.org/10.1097/IAE.0000000000002327
Martinez-Serrano MG, Rodriguez-Reyes A, Guerrero-Naranjo JL, Salcedo-Villanueva G, Fromow-Guerra J, Garcia-Aguirre G, Morales-Canton V, Velez-Montoya R (2017) Long-term follow-up of patients with choroidal neovascularization due to angioid streaks. Clin Ophthalmol 11:23–30. https://doi.org/10.2147/OPTH.S118016
Georgalas I, Papaconstantinou D, Koutsandrea C, Kalantzis G, Karagiannis D, Georgopoulos G, Ladas I (2009) Angioid streaks, clinical course, complications, and current therapeutic management. Ther Clin Risk Manag 5:81–89
Chassaing N, Martin L, Calvas P, Le Bert M, Hovnanian A (2005) Pseudoxanthoma elasticum: a clinical, pathophysiological and genetic update including 11 novel ABCC6 mutations. J Med Genet 42:881–892. https://doi.org/10.1136/jmg.2004.030171
Le Saux O, Martin L, Aherrahrou Z, Leftheriotis G, Varadi A, Brampton CN (2012) The molecular and physiological roles of ABCC6: more than meets the eye. Front Genet 3:289. https://doi.org/10.3389/fgene.2012.00289
Sawa M, Ober MD, Freund KB, Spaide RF (2006) Fundus autofluorescence in patients with pseudoxanthoma elasticum. Ophthalmology 113:814–820 e812. https://doi.org/10.1016/j.ophtha.2006.01.037
Schoenberger SD, Agarwal A (2013) Geographic chorioretinal atrophy in pseudoxanthoma elasticum. Am J Ophthalmol 156:715–723. https://doi.org/10.1016/j.ajo.2013.05.034
Finger RP, Charbel Issa P, Ladewig M, Gotting C, Holz FG, Scholl HP (2009) Fundus autofluorescence in pseudoxanthoma elasticum. Retina 29:1496–1505. https://doi.org/10.1097/IAE.0b013e3181aade47
Ueda-Arakawa N, Ooto S, Tsujikawa A, Yamashiro K, Oishi A, Yoshimura N (2013) Sensitivity and specificity of detecting reticular pseudodrusen in multimodal imaging in Japanese patients. Retina 33:490–497. https://doi.org/10.1097/IAE.0b013e318276e0ae
Pumariega NM, Smith RT, Sohrab MA, Letien V, Souied EH (2011) A prospective study of reticular macular disease. Ophthalmology 118:1619–1625. https://doi.org/10.1016/j.ophtha.2011.01.029
Schmitz-Valckenberg S, Alten F, Steinberg JS, Jaffe GJ, Fleckenstein M, Mukesh BN, Hohman TC, Holz FG Geographic Atrophy Progression Study G(2011) Reticular drusen associated with geographic atrophy in age-related macular degeneration. Invest Ophthalmol Vis Sci 52:5009–5015. https://doi.org/10.1167/iovs.11-7235
Spaide RF (2018) Improving the age-related macular degeneration construct: a new classification system. Retina 38:891–899. https://doi.org/10.1097/IAE.0000000000001732
Spaide RF (2013) Outer retinal atrophy after regression of subretinal drusenoid deposits as a newly recognized form of late age-related macular degeneration. Retina 33:1800–1808. https://doi.org/10.1097/IAE.0b013e31829c3765
Gliem M, Hendig D, Finger RP, Holz FG, Charbel Issa P (2015) Reticular pseudodrusen associated with a diseased Bruch membrane in pseudoxanthoma elasticum. JAMA Ophthalmol 133:581–588. https://doi.org/10.1001/jamaophthalmol.2015.117
Zweifel SA, Imamura Y, Spaide TC, Fujiwara T, Spaide RF (2010) Prevalence and significance of subretinal drusenoid deposits (reticular pseudodrusen) in age-related macular degeneration. Ophthalmology 117:1775–1781. https://doi.org/10.1016/j.ophtha.2010.01.027
Kumar V (2018) Reticular pseudodrusen and thin choroid are associated with angioid streaks. Ophthalmic Surg Lasers Imaging Retina 49:402–408. https://doi.org/10.3928/23258160-20180601-04
Smith RT, Sohrab MA, Busuioc M, Barile G (2009) Reticular macular disease. Am J Ophthalmol 148:733–743 e732. https://doi.org/10.1016/j.ajo.2009.06.028
Smith RT, Chan JK, Busuoic M, Sivagnanavel V, Bird AC, Chong NV (2006) Autofluorescence characteristics of early, atrophic, and high-risk fellow eyes in age-related macular degeneration. Invest Ophthalmol Vis Sci 47:5495–5504. https://doi.org/10.1167/iovs.05-1318
Igarashi N, Matsuura M, Hashimoto Y, Hirasawa K, Murata H, Inoue T, Ryo O, Aihara M, Asaoka R (2016) Assessing visual fields in patients with retinitis pigmentosa using a novel microperimeter with eye tracking: the MP-3. PLoS One 11:e0166666. https://doi.org/10.1371/journal.pone.0166666
Asahina Y, Kitano M, Hashimoto Y, Yanagisawa M, Murata H, Inoue T, Obata R, Asaoka R (2017) The structure-function relationship measured with optical coherence tomography and a microperimeter with auto-tracking: the MP-3, in patients with retinitis pigmentosa. Sci Rep 7:15766. https://doi.org/10.1038/s41598-017-16143-5
Takahashi A, Ooto S, Yamashiro K, Oishi A, Tamura H, Nakanishi H, Ueda-Arakawa N, Tsujikawa A, Yoshimura N (2016) Photoreceptor damage and reduction of retinal sensitivity surrounding geographic atrophy in age-related macular degeneration. Am J Ophthalmol 168:260–268. https://doi.org/10.1016/j.ajo.2016.06.006
Burnham KP, Anderson DR (2014) P values are only an index to evidence: 20th- vs. 21st-century statistical science. Ecology 95:627–630
Gliem M, Muller PL, Birtel J, Hendig D, Holz FG, Charbel Issa P (2016) Frequency, phenotypic characteristics and progression of atrophy associated with a diseased Bruch’s membrane in pseudoxanthoma elasticum. Invest Ophthalmol Vis Sci 57:3323–3330. https://doi.org/10.1167/iovs.16-19388
Molina-Martin A, Perez-Cambrodi RJ, Pinero DP (2018) Current clinical application of microperimetry: a review. Semin Ophthalmol 33:620–628. https://doi.org/10.1080/08820538.2017.1375125
Sugiura A, Fujino R, Takemiya N, Shimizu K, Matsuura M, Murata H, Inoue T, Obata R, Asaoka R (2017) The association between visual function and retinal structure in chronic central serous chorioretinopathy. Sci Rep 7:16288. https://doi.org/10.1038/s41598-017-16339-9
Ueda-Arakawa N, Ooto S, Nakata I, Yamashiro K, Tsujikawa A, Oishi A, Yoshimura N (2013) Prevalence and genomic association of reticular pseudodrusen in age-related macular degeneration. Am J Ophthalmol 155:260–269 e262. https://doi.org/10.1016/j.ajo.2012.08.011
Klein R, Meuer SM, Knudtson MD, Iyengar SK, Klein BE (2008) The epidemiology of retinal reticular drusen. Am J Ophthalmol 145:317–326. https://doi.org/10.1016/j.ajo.2007.09.008
Greferath U, Guymer RH, Vessey KA, Brassington K, Fletcher EL (2016) Correlation of histologic features with in vivo imaging of reticular pseudodrusen. Ophthalmology 123:1320–1331. https://doi.org/10.1016/j.ophtha.2016.02.009
Curcio CA, Presley JB, Millican CL, Medeiros NE (2005) Basal deposits and drusen in eyes with age-related maculopathy: evidence for solid lipid particles. Exp Eye Res 80:761–775. https://doi.org/10.1016/j.exer.2004.09.017
Sivaprasad S, Bird A, Nitiahpapand R, Nicholson L, Hykin P, Chatziralli I, Moorfields UCLAMDC (2016) Perspectives on reticular pseudodrusen in age-related macular degeneration. Surv Ophthalmol 61:521–537. https://doi.org/10.1016/j.survophthal.2016.02.005
Querques G, Massamba N, Srour M, Boulanger E, Georges A, Souied EH (2014) Impact of reticular pseudodrusen on macular function. Retina 34:321–329. https://doi.org/10.1097/IAE.0b013e3182993df1
Wu Z, Ayton LN, Makeyeva G, Guymer RH, Luu CD (2015) Impact of reticular pseudodrusen on microperimetry and multifocal electroretinography in intermediate age-related macular degeneration. Invest Ophthalmol Vis Sci 56:2100–2106. https://doi.org/10.1167/iovs.14-16210
Ooto S, Ellabban AA, Ueda-Arakawa N, Oishi A, Tamura H, Yamashiro K, Tsujikawa A, Yoshimura N (2013) Reduction of retinal sensitivity in eyes with reticular pseudodrusen. Am J Ophthalmol 156:1184–1191 e1182. https://doi.org/10.1016/j.ajo.2013.06.036
Sulzbacher F, Kiss C, Kaider A, Eisenkoelbl S, Munk M, Roberts P, Sacu S, Schmidt-Erfuth U (2012) Correlation of SD-OCT features and retinal sensitivity in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 53:6448–6455. https://doi.org/10.1167/iovs.11-9162
Hautamäki A, Oikkonen J, Onkamo P, Immonen I (2014) Correlation between components of newly diagnosed exudative age-related macular degeneration lesion and focal retinal sensitivity. Acta Ophthalmol 92:51–58. https://doi.org/10.1111/j.1755-3768.2012.02556.x
Ogino K, Tsujikawa A, Yamashiro K, Ooto S, Oishi A, Nalata I, Miyake M, Takahashi A, Ellabban AA, Yoshimura N (2014) Multimodal evaluation of macular function in age-related macular degeneration. Jpn J Ophthalmol 58:155–165. https://doi.org/10.1007/s10384-013-0295-z
Funding
This study was done under JSPS KAKENHI Grant Number JP16K11260. The organization had no role in study design, in the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was not required by the IRB, but participants who did not grant authorization to use their medical records for the research were excluded from analyses.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nomura, Y., Inoue, T., Asano, S. et al. Retinal sensitivity in angioid streaks. Graefes Arch Clin Exp Ophthalmol 257, 1591–1599 (2019). https://doi.org/10.1007/s00417-019-04332-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04332-z