Abstract
Purpose
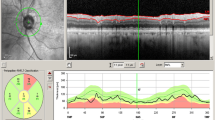
To evaluate the macular and peripapillary morpho-vascular changes in ADOA, using optical coherence tomography (OCT) and OCT angiography (OCTA).
Methods
Prospectively defined, cross-sectional case-control study. Consecutive patients with a genetic or clinical diagnosis of ADOA along with age- and sex-matched controls were included. The radial peripapillary capillary (RPC) density and vessel density (VD) in the parafoveal superficial and deep capillary plexuses (SCP and DCP, respectively) were evaluated with OCTA. The ganglion cell complex (GCC) and retinal nerve fiber layer (RNFL) thickness were determined using structural OCT. We applied a previously validated customized macro (Fiji, SciJava Consortium) to compute RPC density. The remaining parameters were calculated by the built-in software. Non-parametric methods were used for data analysis. The target α level was 0.05, which was adjusted through Bonferroni’s correction when multiple outcomes were tested.
Results
Fifty-eight eyes (n = 29 control; n = 29 ADOA) from 30 subjects (mean age 42.43 ± 15.30 years; 37.93% male) were included. Parafoveal SCP VD, GCC thickness, RPC VD in the temporal quadrant, as well as RNFL thickness in the nasal and temporal quadrants were decreased in ADOA eyes (all p < 0.001). When only patients with genetically confirmed diagnosis were included, capillary dropout in the circumpapillary superior and inferior quadrants also became evident (both p < 0.001). The GCC/parafoveal SCP ratio was increased in ADOA, relatively to matched controls. In contrast, none of the circumpapillary morpho-vascular ratios was significantly different in ADOA eyes.
Conclusions
The microvascular and structural changes found in ADOA suggest that both the macular and peripapillary regions are involved, although the threshold for damage of the structural and vascular components may be different for each region. Larger series with longitudinal follow-up may validate OCTA biomarkers helpful for disease monitoring.



Similar content being viewed by others
References
Pretegiani E, Rosini F, Rufa A, Gallus G, Cardaioli E, Pozzo P, Bianchi S, Serchi V, Collura M, Franceschini R, Marzoli SB, Dotti MT, Federico A (2017) Genotype-phenotype and OCT correlations in autosomal dominant optic atrophy related to OPA1 gene mutations : report of 13 Italian families. J Neurol Sci 382:29–35
Cesareo M, Ciuffoletti E, Martucci A, Sebastiani J, Sorge P, Lamantea E, Garavaglia B, Ricci F, Cusumano A, Nucci C, Brancati F (2017) Assessment of the retinal posterior pole in dominant optic atrophy by spectral-domain optical coherence tomography and microperimetry. PLoS One 30:1–16
Lenaers G, Hamel C, Delettre C, Amati-bonneau P, Procaccio V, Bonneau D, Reynier P, Milea D (2012) Dominant optic atrophy. Orphanet J Rare Dis 7:46
Balducci N, Ciardella A, Gattegna R, Cascavilla ML, Morgia C, Parisi V, Bandello F, Carelli V, Barboni P (2017) Optical coherence tomography angiography of the peripapillary retina and optic nerve head in dominant optic atrophy. Mitochondrion 36:60–65
Corajevic N, Larsen M, Cecilia R (2017) Thickness mapping of individual retinal layers and sectors by Spectralis SD-OCT in autosomal dominant optic atrophy. Acta Ophthalmol 96:251–256
Yu-wai-man P, Griffiths PG, Burke A (2010) The prevalence and natural history of dominant optic atrophy due to OPA1. Ophthalmology 117:1538–1546
Alexander C, Votruba M, Pesch UE, Thiselton DL, Mayer S, Rodriguez M, Kellner U, Leo-kottler B, Auburger G, Bhattacharya SS, Wissinger B (2000) OPA1, encoding a dynamin-related GTPase, is mutated in autosomal dominant optic atrophy linked to chromosome 3q28. Nat Genet 26:211–215
Delettre C, Lenaers G, Griffoin J, Gigarel N, Lorenzo C, Belenguer P, Pelloquin L, Grosgeorge J, Turc-carel C, Perret E, Astarie-dequeker C, Lasquellec L, Arnaud B, Ducommun B, Kaplan J, Hamel CP (2000) Nuclear gene OPA1, encoding a mitochondrial dynamin- related protein, is mutated in dominant optic atrophy. Nat Genet 26:207–210
Barboni P, Savini G, Parisi V, Carbonelli M, Morgia C, Maresca A, Sadun F, Negri AM, Carta A, Sadun AA, Carelli V (2011) Retinal nerve Fiber layer thickness in dominant optic atrophy. Ophthalmology 118:2076–2080
Kim T, Hwang J (2007) Stratus OCT in dominant optic atrophy. J Glaucoma 16:655–658
Mo S, Phillips E, Krawitz BD, Garg R, Salim S, Chui P (2017) Visualization of radial Peripapillary capillaries using optical coherence tomography angiography: the effect of image averaging. PLoS One 12:1–17
Kousal B, Kolarova H, Meliska M, Bydzovsky J, Diblik P, Kulhanek J, Votruba M, Honzik T, Liskova P (2018) Peripapillary microcirculation in Leber hereditary optic neuropathy. Acta Ophthalmol
Balducci N, Cascavilla ML, Ciardella A, Morgia C, Triolo G, Parisi V, Bandello F, Sadun A, Carelli V, Barboni P (2018) Peripapillary vessel density changes in Leber’s hereditary optic neuropathy: a new biomarker. Clin Exp Ophthalmol 46:1055–1062
Liu L, Jia Y, Takusagawa HL, Pechauer AD, Edmunds B, Lombardi L, Davis E, Morrison JC, Huang D (2015) Optical coherence tomography angiography of the Peripapillary retina in Glaucoma. JAMA Ophthalmol 133:1045–1052
Wang X, Jiang C, Ko T, Yu X, Min W, Shi G, Sun X (2015) Correlation between optic disc perfusion and glaucomatous severity in patients with open-angle glaucoma : an optical coherence tomography angiography study. Graefe’s Arch. Clin Exp Ophthalmol 253:1557–1564
Holló G (2016) Vessel density calculated from OCT angiography in 3 peripapillary sectors in normal, ocular hypertensive, and glaucoma eyes. Eur J Ophthalmol 26:42–45
Yarmohammadi A, Zangwill LM, Diniz-filho SA, Youse S, Saunders LJ, Belghith A, Manalastas PIC, Medeiros FA, Weinreb RN (2016) Relationship between optical coherence tomography angiography vessel density and severity of visual field loss in Glaucoma. Am Acad Ophthalmol 123:2498–2508
Wang X, Jia Y, Potsaid B, Liu JJ, Baumann B, Hornegger J, Fujimoto JG, Wu Q, Huang D (2014) Optical coherence tomography angiography of optic nerve head and parafovea in multiple sclerosis. Br J Ophthalmol 98:1368–1373
Tokayer J, Jia Y, Dhalla AH, Huang D (2013) Blood flow velocity quantification using split- spectrum amplitude-decorrelation angiography with optical coherence tomography. Biomed Opt Express 4:1909–1924
Kraus MF, Potsaid B, Mayer MA, Bock R, Baumann B, Liu JJ, Hornegger J, Fujimoto JG (2012) Motion correction in optical coherence tomography volumes on a per A-scan basis using orthogonal scan patterns. Biomed Opt Express 3:457–463
Jia Y, Tan O, Tokayer J, Potsaid B, Wang Y, Jonathan J, Kraus MF, Subhash H, Fujimoto JG, Hornegger J, Huang D (2012) Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express 20:4710–4725
Jia Y, Morrison J, Tokayer J, Tan O, Lombardi L, Baumann B, Lu CD, Choi W, Fujimoto JG, Huang D (2012) Quantitative OCT angiography of optic nerve head blood flow. Biomed Opt Expree 3:3127–3137
Wei E, Jia Y, Tan O, Potsaid B, Liu J, Choi W, Fujimoto J, Huang D (2013) Parafoveal retinal vascular response to pattern visual stimulation assessed with OCT angiography. PLoS One 8:1–7
Martins A, Farinha C, Raimundo M, Lopes M, Santos AR, Melo P, Marques M, Marques JP, Barreto P, Cachulo ML, Neves C, Cunha-Vaz J (2018) Multimodal evaluation of the fellow eye of patients with retinal angiomatous. Ophthalmic Res 59:88–97
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, Tinevez J, White DJ, Hartenstein V, Eliceiri K, Tomancak P, Cardona A (2012) Fiji: an open-source platform for biological-image analysis. Nat Methods 9:676–682
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675
Rodrigues TM, Marques JP, Soares M, Dolan MJ, Melo P, Simão S, Teles J, Figueira J, Murta JN (2018) Peripapillary neuro-vascular coupling in the early stages of diabetic retinopathy. Retina. https://doi.org/10.1097/IAE.0000000000002328
Wickham H (2009) A layered grammar of graphics. J Comput Graph Stat:37–41
Kjer P, Jensen OA, Klinken L (1983) Histopathology of eye, optic nerve and brain in a case of dominant optic atrophy. Acta Ophthalmol 61:300–312
Inoue M, Himori KH, Takeshita T, Aizawa N, Shiga Y, Omodaka K, Nishiguchi KM, Takahashi H, Nakazawa T (2016) The reduction of temporal optic nerve head microcirculation in autosomal dominant optic atrophy. Acta Ophthalmol 94:580–585
Himori N, Kunikata H, Inoue M, Takeshita T, Nishiguchi KM, Takeshita T (2017) Optic nerve head microcirculation in autosomal dominant optic atrophy and normaltension glaucoma. Acta Ophthalmol 95:799–800
Yu-Wai-Man P, Stewart JD, Hudson G, Andrews RM, Griffiths PG, Birch MK, Chinnery PF (2010) OPA1 increases the risk of normal but not high tension glaucoma. J Med Genet 47:120–125
Aung T, Ocaka L, Ebenezer ND, Morris AG, Krawczak M, Thiselton DL, Alexander C, Votruba M, Brice G, Child AH, Francis PJ, Hitchings RA (2002) A major marker for normal tension glaucoma: association with polymorphisms in the OPA1 gene. Hum Genet 1:52–56
Mabuchi F, Tang S, Kashiwagi K, Yamagata Z, Iijima H, Tsukahara S (2007) The OPA1 gene polymorphism is associated with Normal tension and high tension Glaucoma. Am J Ophthalmol 143:125–130
Powell BL, Toomes C, Scott S, Yeung A, Marchbank NJ, Spry PG, Lumb R, Inglehearn CF, Churchill AJ (2003) Polymorphisms in OPA1 are associated with normal tension glaucoma. Mol Vis 9:460–464
Gränse L, Bergstrand I, Thiselton D, Ponjavic V, Heijl A, Votruba M, Andréasson S (2003) Electrophysiology and ocular blood flow in a family with dominant optic nerve atrophy and a mutation in the OPA1 gene. Ophthalmic Genet 24:233–246
Funding
This was an academic research project, with no specific funding available.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.P.M. performs consulting services for Bayer. J.N.M. is a member of the scientific Advisory Board of Alcon. R.S. is a member of the Advisory Board for Bayer, Allergan, Novartis, Alcon, THEA and Alimera. The remaining authors have no conflict of interest to disclose. None of the authors has any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments and this research project was approved by the institutional research committee of Centro Hospitalar e Universitário de Coimbra (CHUC).
Informed consent
Oral and written informed consent was obtained from all individual participants included in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martins, A., Rodrigues, T.M., Soares, M. et al. Peripapillary and macular morpho-vascular changes in patients with genetic or clinical diagnosis of autosomal dominant optic atrophy: a case-control study. Graefes Arch Clin Exp Ophthalmol 257, 1019–1027 (2019). https://doi.org/10.1007/s00417-019-04267-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04267-5