Abstract
Purpose
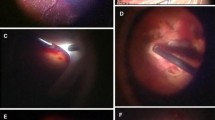
Pneumatic displacement of submacular hemorrhages (SMHs) with intravitreal injection of sulfur hexafluoride (SF6) gas with or without tissue plasminogen activator (tPA) and prone posturing is an effective minimally invasive treatment. We observed some cases in which simultaneous flattening of hemorrhagic pigment epithelial detachments (PEDs) occurred after prone posturing. This study evaluated the impact of pneumatic displacement using tPA to treat PEDs and visual outcomes in eyes with SMHs secondary to neovascular age-related macular degeneration (AMD).
Methods
This retrospective analysis reviewed the medical records of 32 patients (33 eyes) who underwent pneumatic displacement for AMD-associated SMHs. The SMHs were related to polypoidal choroidal vasculopathy (PCV) in 24 eyes and typical AMD in nine eyes and treated with intravitreal injection of SF6 gas with tPA. We assessed the postoperative best-corrected visual acuities (BCVAs), prevalence and flattening rates of the PEDs, and the number of additional treatments.
Results
The mean follow-up period was 35.4 ± 19.8 months. The BCVAs improved significantly in eyes with PCV compared with eyes with typical AMD. Thirty-one (93.9%) of 33 eyes had an accompanying PED. The PEDs flattened in 14 (58.3%) of 24 eyes with PCV but in only one (14.3%) of seven eyes with typical AMD (p = 0.04). A mean of one additional treatment was administered during the first year in 15 eyes with flattened PEDs, which was significantly (p < 0.05) fewer than the 3.6 additional treatments in 16 eyes with persistent PEDs.
Conclusions
PEDs often accompany SMHs secondary to neovascular AMD. Pneumatic displacement of the SMHs using tPA unexpectedly flattened the PEDs, especially in eyes with PCV, and was associated with fewer additional treatments.



Similar content being viewed by others
References
Benner JD, Hay A, Landers MB III, Hjelmeland LM, Morse LS (1994) Fibrinolytic-assisted removal of experimental subretinal hemorrhage within seven days reduces outer retinal degeneration. Ophthalmology 101:672–681
Toth CA, Morse LS, Hjelmeland LM, Landers MB III (1991) Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch Ophthalmol 109:723–729
Ohji M, Saito Y, Hayashi A, Lewis JM, Tano Y (1998) Pneumatic displacement of subretinal hemorrhage without tissue plasminogen activator. Arch Ophthalmol 116:1326–1332
Mizutani T, Yasukawa T, Ito Y, Takase A, Hirano Y, Yoshida M, Ogura Y (2011) Pneumatic displacement of submacular hemorrhage with or without tissue plasminogen activator. Graefes Arch Clin Exp Ophthalmol 249:1153–1157
Schulze SD, Hesse L (2002) Tissue plasminogen activator plus gas injection in patients with subretinal hemorrhage caused by age-related macular degeneration: predictive variables for visual outcome. Graefes Arch Clin Exp Ophthalmol 240:717–720
Chen CY, Hooper C, Chiu D, Chamberlain M, Karia N, Heriot WJ (2007) Management of submacular hemorrhage with intravitreal injection of tissue plasminogen activator and expansile gas. Retina 27:321–328
Tsymanava A, Uhlig CE (2012) Intravitreal recombinant tissue plasminogen activator without and with additional gas injection in patients with submacular haemorrhage associated with age-related macular degeneration. Acta Ophthalmol 90:633–638
Kitahashi M, Baba T, Sakurai M, Yokouchi H, Kubota-Taniai M, Mitamura Y, Yamamoto S (2014) Pneumatic displacement with intravitreal bevacizumab for massive submacular hemorrhage due to polypoidal choroidal vasculopathy. Clin Ophthalmol 8:485–492
Meyer CH, Scholl HP, Eter N, Helb HM, Holz FG (2008) Combined treatment of acute subretinal haemorrhages with intravitreal recombined tissue plasminogen activator, expansile gas and bevacizumab: a retrospective pilot study. Acta Ophthalmol 86:490–494
Matt G, Sacu S, Stifter E, Prunte C, Schmidt-Erfurth U (2010) Combination of intravitreal rTPA, gas and ranibizumab for extensive subfoveal haemorrhages secondary to neovascular age-related macular degeneration. Klin Monatsbl Augenheilkd 227:221–225
Guthoff R, Guthoff T, Meigen T, Goebel W (2011) Intravitreous injection of bevacizumab, tissue plasminogen activator, and gas in the treatment of submacular hemorrhage in age-related macular degeneration. Retina 31:36–40
Chang W, Garg SJ, Maturi R, Hsu J, Sivalingam A, Gupta SA, Regillo CD, Ho AC (2014) Management of thick submacular hemorrhage with subretinal tissue plasminogen activator and pneumatic displacement for age-related macular degeneration. Am J Ophthalmol 157:1250–1257
Arias L, Mones J (2010) Transconjunctival sutureless vitrectomy with tissue plasminogen activator, gas and intravitreal bevacizumab in the management of predominantly hemorrhagic age-related macular degeneration. Clin Ophthalmol 4:67–72
Kamei M, Tano Y, Maeno T, Ikuno Y, Mitsuda H, Yuasa T (1996) Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol 121:267–275
Moisseiev E, Ben Ami T, Barak A (2014) Vitrectomy and subretinal injection of tissue plasminogen activator for large submacular hemorrhage secondary to AMD. Eur J Ophthalmol 24:925–931
Kimura S, Morizane Y, Hosokawa M, Shiode Y, Kawata T, Doi S, Matoba R, Hosogi M, Fujiwara A, Inoue Y, Shiraga F (2015) Submacular hemorrhage in polypoidal choroidal vasculopathy treated by vitrectomy and subretinal tissue plasminogen activator. Am J Ophthalmol 159:683–689
Kadonosono K, Arakawa A, Yamane S, Inoue M, Yamakawa T, Uchio E, Yanagi Y (2015) Displacement of submacular hemorrhages in age-related macular degeneration with subretinal tissue plasminogen activator and air. Ophthalmology 122:123–128
Heriot WJ (1996) Intravitreal gas and TPA: an outpatient procedure for submacular hemorrhage. American Academy of Ophthalmology Annual Vitreoretinal Update, Chicago, IL
Heriot WJ (1997) Further experience in management of submacular hemorrhage with intravitreal tPA. In: Proceedings of the 1997 update on macular surgery. American Academy of Ophthalmology, San Francisco, CA, pp 82–84
Treumer F, Roider J, Hillenkamp J (2012) Long-term outcome of subretinal coapplication of rtPA and bevacizumab followed by repeated intravitreal anti-VEGF injections for neovascular AMD with submacular haemorrhage. Br J Ophthalmol 96:708–713
Kunavisarut P, Thithuan T, Patikulsila D, Choovuthayakorn J, Watanachai N, Chaikitmongkol V, Pathanapitoon K, Rothova A (2017) Submacular hemorrhage: visual outcomes and prognostic factors. Asia Pac J Ophthalmol https://doi.org/10.22608/APO.2017389
Yanyali A, Aytug B, Horozoglu F, Nohutcu AF (2007) Bevacizumab (Avastin) for diabetic macular edema in previously vitrectomized eyes. Am J Ophthalmol 144:124–126
Treumer F, Wienand S, Purtskhvanidze K, Roider J, Hillenkamp J (2017) The role of pigment epithelial detachment in AMD with submacular hemorrhage treated with vitrectomy and subretinal co-application of rtPA and anti-VEGF. Graefes Arch Clin Exp Ophthalmol 255:1115–1123
Hrach CJ, Johnson MW, Hassan AS, Lei B, Sieving PA, Elner VM (2000) Retinal toxicity of commercial intravitreal tissue plasminogen activator solution in cat eyes. Arch Ophthalmol 118:659–663
Johnson MW, Olsen KR, Hernandez E, Irvine WD, Johnson RN (1990) Retinal toxicity of recombinant tissue plasminogen activator in the rabbit. Arch Ophthalmol 108:259–263
Irvine WD, Johnson MW, Hernandez E, Olsen KR (1991) Retinal toxicity of human tissue plasminogen activator in vitrectomized rabbit eyes. Arch Ophthalmol 109:718–722
Hesse L, Schmidt J, Kroll P (1999) Management of acute submacular hemorrhage using recombinant tissue plasminogen activator and gas. Graefes Arch Clin Exp Ophthalmol 237:273–277
Chen SN, Yang TC, Ho CL, Kuo YH, Yip Y, Chao AN (2003) Retinal toxicity of intravitreal tissue plasminogen activator: case report and literature review. Ophthalmology 110:704–708
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Informed consent
Opt-out consent method was chosen, approved by the institutional review board of Nagoya City University Graduate School of Medical Sciences because no information identifying individual participants was involved in this article.
Additional information
The authors have no proprietary interest in any aspect of this report.
Rights and permissions
About this article
Cite this article
Kimura, M., Yasukawa, T., Shibata, Y. et al. Flattening of retinal pigment epithelial detachments after pneumatic displacement of submacular hemorrhages secondary to age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 256, 1823–1829 (2018). https://doi.org/10.1007/s00417-018-4059-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4059-9