Abstract
Purpose
The purpose of our study was to investigate morpho-functional features of the preferred retinal location (PRL) and the transition zone (TZ) in a series of patients with recessive Stargardt disease (STGD1).
Methods
Fifty-two STGD1 patients with at least one ABCA4 mutation, atrophy of the central macula (MA) and an eccentric PRL were recruited for the study. Microperimetry, fundus autofluorescence (FAF), spectral-domain optical coherence tomography (SD-OCT) were performed. The location and stability of the PRL along with the associated FAF pattern and visual sensitivities were determined and compared to the underlying retinal structure.
Results
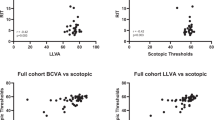
The mean visual sensitivity of the PRLs for the 52 eyes was 10.76 +/- 3.70 dB. For the majority of eyes, PRLs were associated with intact ellipsoid zone (EZ) bands and qualitatively normal FAF patterns. In 17 eyes (32.7%) the eccentric PRL was located at the edge of the MA. In 35 eyes (67.3%) it was located at varying distances from the border of the MA with a TZ between the PRL and the MA. The TZ was associated with decreased sensitivity values (5.92 +/- 4.69 dB) compared to PRLs (p<0.05), with absence/disruption of the EZ band and abnormal FAF patterns (hyper or hypo-autofluorescence).
Conclusions
In STGD1 eccentric PRLs are located away from the border of MA and associated with intact EZ bands and normal FAF. The TZ is characterized by structural and functional abnormalities. The results of multimodal imaging of the PRL and TZ suggest a possible sequence of retinal and functional changes with disease progression that may help in the planning of future therapies; RPE dysfunction appears to be the primary event leading to photoreceptor degeneration and then to RPE loss.






Similar content being viewed by others
References
Fishman GA (1976) Fundus flavimaculatus: a clinical classification. Arch Ophthalmol 94:2061–2067
Gass JDM (1997) Heredodystrophic Disorders Affecting the Pigment Epithelium and Retina. In: Gass JDM. Stereocopic Atlas of Macular Disease. Diagnosis and Treatment. Mosby. St.Louis-London-Phyladelphia-Sidney-Toronto;p.303-435.
Rozet JM, Gerber S, Ducroq D, Hamel C, Dufier JL, Kaplan J (2005) Les dystrophies maculaires héréditaires. J Fr Ophtalmol 28(1):113–124
Glazer LC, Dryja TP (2002) Understanding the etiology of Stargardt’s disease. Ophth Clin North Am 15(1):93–100
Walia S, Fishman GA (2009) Natural History of Phenotypic Changes in Stargardt Macular Dystrophy. Ophthalmic Genetics 30:63–68
Eagle RC Jr, Lucier AC, Bernardino VB Jr, Yanoff M (1980) Retinal pigment epithelial abnormalities in fundus flavimaculatus: a light and electron microscopic study. Ophthalmology. 87(12):1189–1200
Sparrow JR, Marsiglia M, Allikmets R, Tsang SH, Lee W, Duncker T, Zernant J (2015) Flecks in Recessive Stargardt Disease: Short-Wavelength Autofluorescence, Near-Infrared Autofluorescence, and Optical Coherence Tomography. Invest Ophthalmol Vis. Sci. 56:5029–5039
Sunness JS, Applegate CA, Haselwood D, Rubin GS (1996) Fixation Patterns and Reading Rates in Eyes with Central Scotomas from Advanced Atrophic Age-related Macular Degeneration and Stargardt Disease. Ophthalmology 103:1458–1466
Messias A, Reinhard J, Velascoe Cruz AA, Dietz K, MacKeben M, Trauzettel-Klosinski S (2007) Eccentric fixation in Stargardt’s disease assessed by Tubingen perimetry. Invest Ophthalmol Vis Sci. 48(12):5815–5822
Greenstein VC, Santos RAV, Tsang SH, Smith RT, Barile GR, Seiple W (2008) Preferred Retinal Locus in Macular Disease: Characteristics and Clinical Implications. Retina 28(9):1234–1240
Cheung SH, Legge GE (2005) Fuctional and cortical adaptations to central vision loss. Visual Neuroscience 22:187–201
Huxlin KR (2008) Perceptual plasticity in damaged adult visual systems. Vision Research 48:2154–2166
Tarita-Nistor L, Gonzalez EG, Markowitz SN, Steinbach MJ (2009) Plasticity of fixation in patients with central vision loss. Visual Neuroscience 26:487–494
Macedo AF, Cardoso Nascimento SM, Silva Gomes AO, Teixeira Puga A (2007) Fixation in patients with juvenile macular disease. Optometry and Vision Science 84(9):852–858
Schuchard RA (2005) Preferred retinal loci and macular scotoma characteristics in patients with age-related macular degeneration. Canadian Journal of Ophthalmology 40:303–312
Lazow MA, Hood DC, Ramachandran R, Burke TR et al (2011) Transition Zones Between Healthy and Diseased Retina in Choideremia (CHM) and Stargardt Disease (STGD) as Compared to Retinitis Pigmentosa (RP). Invest Ophthalmol Vis Sci 52(13):9581–9590
Fishman GA, Stone EM, Grover S et al (1999) Variation of clinical expression in patients with Stargardt dystrophy and sequence variations in the ABCR gene. Arch Ophthalmol. 17(4):504–510
Crossland MD, Dunbar HMP, Rubin GS (2009) Fixation stability measurement with MP1microperimeter. Retina. 29:651–656
Gomez NL, Greenstein VC, Carlson AN, Tsang SH, Smith RT, Carr RE, Hood DC, Chang S (2009) A comparison of Fundus Autofluorescence and Retinal Structure in Patients with Stargardt Disease. Invest Ophthalmol Vis Sci. 50:3953–3959
Reinhard J, Messias A, Dietz K et al (2007) Quantifying fixation in patients with Stargardt disease. Vision Res 47(15):2076–2085
Testa F, Rossi S, Sodi A, Passerini I, Di Iorio V, Della Corte M, Banfi S, Surace EM, Menchini U, Auricchio A, Simonelli F (2012) Correlation between photoreceptor layer integrity and visual function in patients with Stargardt disease: implications for gene therapy. Invest Ophthalmol Vis Sci 53(8):4409–4415
Ergun E, Hermann B, Wirtitsch M, Unterhuber A, Ko TH et al (2005) Assessment of central visual function in Stargardt’s disease/fundus flavimaculatus with ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci. 46(1):310–316
Testa F, Melillo P, Di Iorio V et al (2014) Macular Function and Morphologic features in Juvenile Stargardt Disease. Ophthalmol 121:2399–2405
Burke TR, Duncker T, Woods RL et al (2014) Quantitative fundus autofluorescence in recessive stargardt disease. Invest Ophthalmol Vis Sci. 55:2841–2852
Ritter M, Zotter S, Schmidt WM et al (2013) Characterization of Stargardt disease using polarization-sensitive optical coherence tomography and fundus autofluorescence imaging. Invest Ophthalmol Vis Sci. 54:6416–6425
Greenstein VC, Schuman AD, Lee W et al (2015) Near-infrared autofluorescence: its relationship to short-wavelength autofluorescence and optical coherence tomography in recessive stargardt disease. Invest Ophthalmol Vis Sci. 56(5):3226–3234
Lois N, Holder GE, Bunce C et al (2001) Phenotypic subtypes of Stargardt macular dystrophy-fundus flavimaculatus. Arch Ophthalmol. 119(3):359–369
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The National Eye Institute/NIH EY09076, Foundation Fighting Blindness and Research to Prevent Blindness of the Department of Ophthalmology, Columbia University provided financial support in the form of grants. S.H.T., a member of the RD-CURE Consortium, is supported by the Tistou and Charlotte Kerstan Foundation, the Schneeweiss Stem Cell Fund, New York State [C029572], the Foundation Fighting Blindness New York Regional Research Center Grant [C-NY05-0705-0312], and the Joel Hoffman Fund. The sponsors had no role in the design or conduct of this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Verdina, T., Greenstein, V.C., Sodi, A. et al. Multimodal analysis of the Preferred Retinal Location and the Transition Zone in patients with Stargardt Disease. Graefes Arch Clin Exp Ophthalmol 255, 1307–1317 (2017). https://doi.org/10.1007/s00417-017-3637-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3637-6