Abstract
Purpose
Descemet membrane endothelial keratoplasty (DMEK) is superior to penetrating keratoplasty (PK) in terms of visual rehabilitation, intraoperative safety and risk of rejection. Therefore, it seems reasonable to perform DMEK in eyes with endothelial failure following PK. We herein report our first clinical results.
Methods
Nineteen eyes with endothelial graft failure following PK were treated with DMEK. The majority of these eyes (12) had limited visual potential. The major indication for DMEK was pain relief in patients with bullous keratopathy. Visual acuity (VA), central corneal thickness (CCT), rate of graft dislocations, graft survival, graft rejections and other complications were extracted from the medical records.
Results
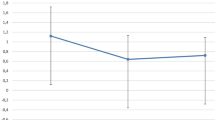
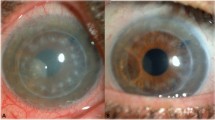
Although comorbidities limiting VA were present in 12 of the 19 eyes, VA increased from 0.05 to 0.1 (median) in 16 eyes. CCT decreased substantially (range 63–363 μm). Rebubbling was necessary in five eyes with incomplete graft adherence. There were two immunologic graft reactions and three graft failures. No major complications like endophthalmitis or expulsive bleeding occurred.
Conclusions
DMEK is feasible to treat endothelial graft failure following PK. This is even true for eyes with limited visual potential.




Similar content being viewed by others
References
Melles GRJ (2006) Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea 25:879–881. doi:10.1097/01.ico.0000243962.60392.4f
Heinzelmann S, Maier P, Reinhard T (2011) Perspectives of posterior lamellar keratoplasty. In search of the perfect lamella. Ophthalmol Z Dtsch Ophthalmol Ges 108:825–832. doi:10.1007/s00347-011-2330-0
Heinzelmann S, Böhringer D, Eberwein P et al (2016) Outcomes of Descemet membrane endothelial keratoplasty, Descemet stripping automated endothelial keratoplasty and penetrating keratoplasty from a single centre study. Graefes Arch Clin Exp Ophthalmol 254:515–522. doi:10.1007/s00417-015-3248-z
Patel SV, Armitage WJ, Claesson M (2014) Keratoplasty outcomes: are we making advances? Ophthalmology 121:977–978. doi:10.1016/j.ophtha.2014.01.029
Hamzaoglu EC, Straiko MD, Mayko ZM et al (2015) The first 100 eyes of standardized Descemet stripping automated endothelial keratoplasty versus standardized Descemet membrane endothelial keratoplasty. Ophthalmology 122:2193–2199. doi:10.1016/j.ophtha.2015.07.003
Maier A-KB, Gundlach E, Gonnermann J et al (2013) Fellow eye comparison of Descemet membrane endothelial keratoplasty and penetrating keratoplasty. Cornea 32:1344–1348. doi:10.1097/ICO.0b013e31829dd816
Pineros O (1996) Long-term results after penetrating keratoplasty for Fuchs’ endothelial dystrophy. Arch Ophthalmol 114:15. doi:10.1001/archopht.1996.01100130013002
Pramanik S, Musch D, Sutphin J, Farjo A (2006) Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology 113:1633–1638. doi:10.1016/j.ophtha.2006.02.058
Borderie VM, Boëlle P-Y, Touzeau O et al (2009) Predicted long-term outcome of corneal transplantation. Ophthalmology 116:2354–2360. doi:10.1016/j.ophtha.2009.05.009
Böhringer D, Reinhard T (2013) Long-term keratoplasty graft survival. Ophthalmology 120:216. doi:10.1016/j.ophtha.2012.07.046
Böhringer D, Reinhard T, Spelsberg H, Sundmacher R (2002) Influencing factors on chronic endothelial cell loss characterised in a homogeneous group of patients. Br J Ophthalmol 86:35–38
Böhringer D, Böhringer S, Poxleitner K et al (2010) Long-term graft survival in penetrating keratoplasty: the biexponential model of chronic endothelial cell loss revisited. Cornea 29:1113–1117. doi:10.1097/ICO.0b013e3181d21d07
Reinhard T, Böhringer D, Hüschen D, Sundmacher R (2002) Chronic endothelial cell loss of the graft after penetrating keratoplasty: influence of endothelial cell migration from graft to host. Klin Monatsbl Augenheilkd 219:410–416. doi:10.1055/s-2002-32876
Patel NP, Kim T, Rapuano CJ et al (2000) Indications for and outcomes of repeat penetrating keratoplasty, 1989-1995. Ophthalmology 107:719–724
Claesson M, Armitage WJ (2013) Clinical outcome of repeat penetrating keratoplasty. Cornea 32:1026–1030. doi:10.1097/ICO.0b013e31828a2810
Kitzmann AS, Wandling GR, Sutphin JE et al (2012) Comparison of outcomes of penetrating keratoplasty versus Descemet’s stripping automated endothelial keratoplasty for penetrating keratoplasty graft failure due to corneal edema. Int Ophthalmol 32:15–23. doi:10.1007/s10792-012-9518-4
Ang M, Ho H, Wong C et al (2014) Endothelial keratoplasty after failed penetrating keratoplasty: an alternative to repeat penetrating keratoplasty. Am J Ophthalmol 158:1221–1227. doi:10.1016/j.ajo.2014.08.024
Anshu A, Price MO, Price FW (2013) Descemet membrane endothelial keratoplasty and hybrid techniques for managing failed penetrating grafts. Cornea 32:1–4. doi:10.1097/ICO.0b013e3182488888
Liarakos VS, Satué M, Livny E et al (2015) Descemet membrane endothelial keratoplasty for a decompensated penetrating keratoplasty graft in the presence of a long glaucoma tube. Cornea 34:1613–1616. doi:10.1097/ICO.0000000000000631
Gundlach E, Maier A-KB, Riechardt AI et al (2015) Descemet membrane endothelial keratoplasty as a secondary approach after failure of penetrating keratoplasty. Exp Clin Transplant 13:350–354
Melles GRJ, Ong TS, Ververs B, van der Wees J (2006) Descemet membrane endothelial keratoplasty (DMEK). Cornea 25:987–990. doi:10.1097/01.ico.0000248385.16896.34
Heinzelmann S, Hüther S, Böhringer D et al (2014) Influence of donor characteristics on descemet membrane endothelial keratoplasty. Cornea 33:644–648. doi:10.1097/ICO.0000000000000106
Kruse FE, Laaser K, Cursiefen C et al (2011) A stepwise approach to donor preparation and insertion increases safety and outcome of Descemet membrane endothelial keratoplasty. Cornea 30:580–587
Lange C, Feltgen N, Junker B et al (2009) Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol 247:137–142. doi:10.1007/s00417-008-0926-0
Röck T, Bramkamp M, Bartz-Schmidt KU et al (2015) Causes that influence the detachment rate after Descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol 253:2217–2222. doi:10.1007/s00417-015-3103-2
Tourtas T, Schlomberg J, Wessel JM et al (2014) Graft adhesion in descemet membrane endothelial keratoplasty dependent on size of removal of host’s descemet membrane. JAMA Ophthalmol 132:155–161. doi:10.1001/jamaophthalmol.2013.6222
Brockmann T, Brockmann C, Maier A-K et al (2014) Clinicopathology of graft detachment after Descemet’s membrane endothelial keratoplasty. Acta Ophthalmol (Copenh) 92:e556–e561. doi:10.1111/aos.12419
Price FW, Price MO, Arundhati A (2011) Descemet stripping automated endothelial keratoplasty under failed penetrating keratoplasty: how to avoid complications. Am J Ophthalmol 151:187.e2–188.e2. doi:10.1016/j.ajo.2010.09.033
Straiko MD, Terry MA, Shamie N (2011) Descemet stripping automated endothelial keratoplasty under failed penetrating keratoplasty: a surgical strategy to minimize complications. Am J Ophthalmol 151:233.e2–237.e2. doi:10.1016/j.ajo.2010.08.017
Clements JL, Bouchard CS, Lee WB et al (2011) Retrospective review of graft dislocation rate associated with descemet stripping automated endothelial keratoplasty after primary failed penetrating keratoplasty. Cornea 30:414–418. doi:10.1097/ICO.0b013e3181f7f163
Verdier DD, Sugar A, Baratz K et al (2013) Corneal thickness as a predictor of corneal transplant outcome. Cornea 32:729–736. doi:10.1097/ICO.0b013e31827b14c7
Bourne WM (1983) Morphologic and functional evaluation of the endothelium of transplanted human corneas. Trans Am Ophthalmol Soc 81:403–450
Writing Committee for the Cornea Donor Study Research Group, Sugar A, Gal RL et al (2015) Factors associated with corneal graft survival in the cornea donor study. JAMA Ophthalmol 133:246–254. doi:10.1001/jamaophthalmol.2014.3923
Visby E, Hjortdal J, Nielsen K (2014) Evaluation of grafted patients with donor corneas that today are more than 100 years old. Acta Ophthalmol (Copenh) 92:478–481. doi:10.1111/aos.12231
Price MO, Scanameo A, Feng MT, Price FW (2016) Descemet’s membrane endothelial keratoplasty: risk of immunologic rejection episodes after discontinuing topical corticosteroids. Ophthalmology 123:1232–1236. doi:10.1016/j.ophtha.2016.02.001
Mitry D, Bhogal M, Patel AK et al (2014) Descemet stripping automated endothelial keratoplasty after failed penetrating keratoplasty: survival, rejection risk, and visual outcome. JAMA Ophthalmol 132:742–749. doi:10.1001/jamaophthalmol.2014.352
Anshu A, Price MO, Price FW (2011) Descemet’s stripping endothelial keratoplasty under failed penetrating keratoplasty: visual rehabilitation and graft survival rate. Ophthalmology 118:2155–2160. doi:10.1016/j.ophtha.2011.04.032
Keane MC, Galettis RA, Mills RAD et al (2016) A comparison of endothelial and penetrating keratoplasty outcomes following failed penetrating keratoplasty: a registry study. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-307792
Monnereau C, Quilendrino R, Dapena I et al (2014) Multicenter study of descemet membrane endothelial keratoplasty: first case series of 18 surgeons. JAMA Ophthalmol 132:1192–1198. doi:10.1001/jamaophthalmol.2014.1710
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethical board Freiburg, AZ 88/12) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Heinzelmann, S., Böhringer, D., Eberwein, P. et al. Descemet membrane endothelial keratoplasty for graft failure following penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol 255, 979–985 (2017). https://doi.org/10.1007/s00417-017-3600-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3600-6