Abstract
Background
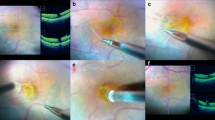
To evaluate demographic, functional, and morphological parameters of idiopathic lamellar macular hole (ILMH).
Methods
Observational longitudinal retrospective study.
Optical coherence tomography examinations and corresponding clinical charts of a series of consecutive patients affected by ILMH, between January 2010 and March 2015, from the database of the Department of Ophthalmology of Trento Hospital, Italy, have been collected and examined.
Demographic and functional parameters were: age (year), gender (male/female), eye (right/left), lens status, best-corrected visual acuity (BCVA) in logarithm of the minimum angle of resolution (LogMAR).
Tomographic parameters were: LMH shape pattern (intraretinal splitting LMH, IR split LMH, and V-shaped LMH, V LMH), posterior vitreous detachment (PVD yes/ PVD no), ERM type (conventional ERM and atypical ERM), integrity of ellipsoid zone (EZ) and external limiting membrane (ELM), residual foveal thickness (RFT) micron (μ), maximal diameter of intraretinal splitting (MDIRS) (μ).
Results
One hundred and eighty-nine eyes of 175 patients were included. The mean age was 72.84 ± 9.6, range 41–96 years. BCVA mean was 0.24 ± 0.25, range 0 –1.3 LogMAR. One hundred and forty-one eyes (74.6 %) were affected by IR split LMH, 48 eyes (25.4 %) were affected by V LMH. Every cases of ILMH were associated with ERM: 117 (61.9 %) conventional ERM, 72 (38.1 %) atypical ERM. A significant prevalence of female gender, phakic condition, and PVD in conventional ERM ILMH subgroup (P = 0.000) was found. BCVA mean was better in the conventional ERM ILMH subgroup (P = 0.000). An association between the interruption of the outer retinal layers (EZ and ELM) and atypical ERM ILMH subgroup was highlighted (P = 0.000). The statistical analysis showed a correlation between BCVA and integrity of ELM (P = 0.000). RFT significantly decreased in atypical ERM ILMH subgroup at 24 months compared to time point 0 (P = 0.027). A progressive increase of MDIRS in both subgroups at 12 months and in atypical ERM ILMH subgroup at 24 months (P = 0.007) was highlighted.
Conclusions
This study demonstrated that ILMH was not a stable condition, showing morphological changes and an involvement of the outer retinal layers during the 2 years of follow-up.








Similar content being viewed by others
References
Witkin AJ, Ko TH, Fujimoto JG et al (2006) Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology 113(3):388–397
Haouchine B, Massin P, Tadayoni R et al (2004) Diagnosis of macular pseudoholes and lamellar macular holes by optical coherence tomography. Am J Ophthalmol 138(5):732–739
Parolini B, Schumann RG, Cereda MG et al (2011) Lamellar macular hole: a clinicopathologic correlation of surgically excised epiretinal membranes. Invest Ophthalmol Vis Sci 25 52(12):9074–9083
Bottoni F, Peroglio Deiro A, Giani A et al (2013) The natural history of lamellar macular holes: a spectral-domain optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 251:467–475
Pang CE, Spaide RF, Freund KB (2014) Epiretinal proliferation seen in association with lamellar macular holes: a distinct clinical entity. Retina 34(8):1513–1523
Pang CE, Spaide RF, Freund KB (2015) Comparing functional and morphological characteristics of lamellar macular hole with and without lamellar macular hole associated epiretinal proliferation. Retina 35(4):720–726
Govetto A, Dacquay Y, Farajzadeh M et al (2016) Lamellar macular hole: two distinct clinical entities? Am J Ophthalmol 164:99–109
Schumann RG, Compera D, Schaumberger MM et al (2015) Epiretinal membrane characteristics correlate with photoreceptor layer defects in lamellar macular holes and macular pseudoholes. Retina 35(4):727–735
Compera D, Entchev E, Haritoglou C et al (2015) Lamellar hole-associated epiretinal proliferation in comparison to epiretinal membranes of macular pseudoholes. Am J Ophthalmol 160(2):373–384
Allen AW Jr, Gass JD (1976) Contraction of a perifoveal epiretinal membrane simulating a macular hole. Am J Ophthalmol 82:684–691
Lujan BJ, Roorda A, Knighton RW (2011) Revealing Henle’s fiber layer using spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci 18 52(3):1486–1492
Otani T, Yamaguchi Y, Kishi S (2011) Improved visualization of Henle fiber layer by changing the measurement beam angle on optical coherence tomography. Retina 31(3):497–501
Staurenghi G, Sadda S, Chakravarthy U (2014) Proposed lexicon for anatomic landmarks in normal posterior segment spectral-domain optical coherence tomography: the IN•OCT consensus. Ophthalmology 121(8):1572–1578
Frisina R, Zampedri E, Marchesoni I (2016) Lamellar macular hole in high myopic eyes with posterior staphyloma; morphological and functional characteristics. Graefes Arch Clin Exp Ophthalmol. doi:10.1007/s00417-016-3383-1
Wakabayashi T, Fujiwara M, Sakaguchi H et al (2010) Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology 117(9):1815–1824
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Formal consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Zampedri, E., Romanelli, F., Semeraro, F. et al. Spectral-domain optical coherence tomography findings in idiopathic lamellar macular hole. Graefes Arch Clin Exp Ophthalmol 255, 699–707 (2017). https://doi.org/10.1007/s00417-016-3545-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3545-1