Abstract
Background
To present the surgical technique and clinical outcomes of transplantation of autologous internal limiting membrane (ILM) for large macular holes (MHs) after failed surgeries with ILM removal.
Methods
Thirteen eyes of 13 consecutive patients with MHs larger than 500 μm after failed surgeries with ILM removal underwent vitrectomy with transplantation of autologous ILM. In the ILM transplantation technique, a small piece of the ILM was peeled off and transplanted inside the macular hole. Fluid–air exchange was then performed. The air was then replaced with 10 % perfluoropropane (C3F8) gas. Comprehensive ophthalmologic examinations and spectral-domain optical coherence tomography were performed preoperatively and postoperatively. The main outcome measures were best-corrected Snellen visual acuity (BCVA) and MH closure rate.
Results
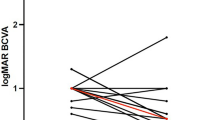
The preoperative mean base diameter of the MHs was 1637.6 + 412.7 μm (range, 814–2092 μm). The preoperative mean minimum diameter was 814.4 + 255.0 μm (range, 546 μm–1485 μm). Complete MH sealing was achieved in 12 eyes after transplantation of the ILM flap. The mean BCVA was 1.15 + 0.21 (range, 1.0–1.6) before surgery and 0.99 + 0.17 (range, 0.7–1.3) at 12 months postoperatively. There was a significant difference in BCVA before versus after the surgery (t = 3.825, P = 0.0002, paired t- test).
Conclusions
Transplantation of autologous ILM is an effective addition to the surgical options for large macular holes after failed surgeries with ILM removal.


Similar content being viewed by others
References
Kelly NE, Wendel RT (1991) Vitreous surgery for idiopathic macular holes. results of a pilot study. Arch Ophthalmol 109(5):654–659
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J (1999) Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology 106(7):1392–1397. doi:10.1016/S0161-6420(99)00730-7, discussion 1397-1398
Fabian ID, Moisseiev J (2011) Sutureless vitrectomy: evolution and current practices. Br J Ophthalmol 95(3):318–324. doi:10.1136/bjo.2009.176495
Spiteri Cornish K, Lois N, Scott NW, Burr J, Cook J, Boachie C, Tadayoni R, la Cour M, Christensen U, Kwok AK (2014) Vitrectomy with internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole. Ophthalmology 121(3):649–655. doi:10.1016/j.ophtha.2013.10.020
Jackson TL, Donachie PH, Sparrow JM, Johnston RL (2013) United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology 120(3):629–634. doi:10.1016/j.ophtha.2012.09.003
D’Souza MJ, Chaudhary V, Devenyi R, Kertes PJ, Lam WC (2011) Re-operation of idiopathic full-thickness macular holes after initial surgery with internal limiting membrane peel. Br J Ophthalmol 95(11):1564–1567. doi:10.1136/bjo.2010.195826
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J (2010) Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 117(10):2018–2025. doi:10.1016/j.ophtha.2010.02.011
Wakely L, Rahman R, Stephenson J (2012) A comparison of several methods of macular hole measurement using optical coherence tomography, and their value in predicting anatomical and visual outcomes. Br J Ophthalmol 96(7):1003–1007. doi:10.1136/bjophthalmol-2011-301287
Kang SW, Ahn K, Ham DI (2003) Types of macular hole closure and their clinical implications. Br J Ophthalmol 87(8):1015–1019
Chen SN, Yang CM (2016) Lens capsular flap transplantation in the management of refractory macular hole from multiple etiologies. Retina 36(1):163–170. doi:10.1097/IAE.0000000000000674
Morizane Y, Shiraga F, Kimura S, Hosokawa M, Shiode Y, Kawata T, Hosogi M, Shirakata Y, Okanouchi T (2014) Autologous transplantation of the internal limiting membrane for refractory macular holes. Am J Ophthalmol 157(4):861–869. doi:10.1016/j.ajo.2013.12.028, e861
Haritoglou C, Schumann R, Reiniger I, Rohleder M, Priglinger SG, Kampik A, Gandorfer A (2006) Evaluation of the internal limiting membrane after conventional peeling during macular hole surgery. Retina 26(1):21–24
Wolf S, Schnurbusch U, Wiedemann P, Grosche J, Reichenbach A, Wolburg H (2004) Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology 111(2):238–243. doi:10.1016/j.ophtha.2003.05.022
Tokuda K, Zorumski CF, Izumi Y (2009) Involvement of illumination in indocyanine green toxicity after its washout in the ex vivo rat retina. Retina 29(3):371–379. doi:10.1097/IAE.0b013e318195cb00
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(BMP 4814 kb)
Rights and permissions
About this article
Cite this article
Dai, Y., Dong, F., Zhang, X. et al. Internal limiting membrane transplantation for unclosed and large macular holes. Graefes Arch Clin Exp Ophthalmol 254, 2095–2099 (2016). https://doi.org/10.1007/s00417-016-3461-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3461-4