Abstract
Purpose
To investigate the dissociation of the Bruch’s membrane opening (BMO) from the scleral canal opening (SO) of the optic disc.
Methods
In this prospective, cross-sectional, observational study, 101 eyes from 101 patients or suspected subjects of primary open angle glaucoma were included. Enhanced depth imaging spectral domain optical coherence tomography images along the long axis of the optic disc were used to visualize better the deep structures around the optic disc on both the temporal and nasal sides. The distances between the BMO and SO were measured at the temporal and nasal sides of the optic disc, and their correlations with age, axial length, intraocular pressure, disc size, disc ovality index, disc torsion degree, and visual field mean deviation were investigated.
Results
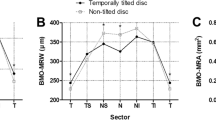
The temporal and nasal distances of BMO from SO correlated significantly with each other (R = 0.632, P < 0.0001). By multiple linear regression analysis, significant correlations were found for disc ovality index (temporal: β = −0.691, P < 0.0001; nasal: β = −0.420, P < 0.0001) and axial length (temporal: β = 0.224, P = 0.002; nasal: β = 0.310, P = 0.001). The other factors did not show any significant correlation.
Conclusion
Locations of the SO at not only the temporal, but also the nasal side of the optic disc are nasally shifted from the BMO with optic disc tilting and axial length elongation in glaucomatous eyes, and are significantly correlated to each other. The nasal shift of the deep structures of the optic disc should be considered especially when assessing myopic eyes with optic disc tilt.



Similar content being viewed by others
References
Ramrattan RS, Wolfs RC, Jonas JB, Hofman A, de Jong PT (1999) Determinants of optic disc characteristics in a general population: the Rotterdam study. Ophthalmology 106:1588–1596
Yang H, Downs JC, Burgoyne CF (2009) Physiologic intereye differences in monkey optic nerve head architecture and their relation to changes in early experimental glaucoma. Investig Ophthalmol Vis Sci 50:224–234
Strouthidis NG, Yang H, Reynaud JF, Grimm JL, Gardiner SK, Fortune B, Burgoyne CF (2009) Comparison of clinical and spectral domain optical coherence tomography optic disc margin anatomy. Investig Ophthalmol Vis Sci 50:4709–4718
Reis AS, Sharpe GP, Yang H, Nicolela MT, Burgoyne CF, Chauhan BC (2012) Optic disc margin anatomy in patients with glaucoma and normal controls with spectral domain optical coherence tomography. Ophthalmology 119:738–747
Apple DJ, Rabb MF, Walsh PM (1982) Congenital anomalies of the optic disc. Surv Ophthalmol 27:3–41
Witmer MT, Margo CE, Drucker M (2010) Tilted optic disks. Surv Ophthalmol 55:403–428
Dorrell D (1978) The tilted disc. Br J Ophthalmol 62:16–20
Kim TW, Kim M, Weinreb RN, Woo SJ, Park KH, Hwang JM (2012) Optic disc change with incipient myopia of childhood. Ophthalmology 119:21–26.e1–3
Nonaka A, Hangai M, Akagi T, Mori S, Nukada M, Nakano N, Yoshimura N (2011) Biometric features of peripapillary atrophy beta in eyes with high myopia. Investig Ophthalmol Vis Sci 52:6706–6713
Kim M, Kim TW, Weinreb RN, Lee EJ (2013) Differentiation of parapapillary atrophy using spectral-domain optical coherence tomography. Ophthalmology 120:1790–1797
Kimura Y, Akagi T, Hangai M, Takayama K, Hasegawa T, Suda K, Yoshikawa M, Yamada H, Nakanishi H, Unoki N, Ikeda HO, Yoshimura N (2014) Lamina cribrosa defects and optic disc morphology in primary open angle glaucoma with high myopia. PLoS One 9, e115313
Takayama K, Hangai M, Kimura Y, Morooka S, Nukada M, Akagi T, Ikeda HO, Matsumoto A, Yoshimura N (2013) Three-dimensional imaging of lamina cribrosa defects in glaucoma using swept-source optical coherence tomography. Investig Ophthalmol Vis Sci 54:4798–4807
Sigal IA, Wang B, Strouthidis NG, Akagi T, Girard MJ (2014) Recent advances in OCT imaging of the lamina cribrosa. Br J Ophthalmol 98(Suppl 2):ii34–9
Park HY, Lee K, Park CK (2012) Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology 119:1844–1851
Spaide RF, Koizumi H, Pozzoni MC (2008) Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 146:496–500
Jonas JB, Martus P, Budde WM, Junemann A, Hayler J (2002) Small neuroretinal rim and large parapapillary atrophy as predictive factors for progression of glaucomatous optic neuropathy. Ophthalmology 109:1561–1567
Teng CC, De Moraes CG, Prata TS, Tello C, Ritch R, Liebmann JM (2010) Beta-Zone parapapillary atrophy and the velocity of glaucoma progression. Ophthalmology 117:909–915
Lee EJ, Kim TW, Weinreb RN, Park KH, Kim SH, Kim DM (2011) β-Zone parapapillary atrophy and the rate of retinal nerve fiber layer thinning in glaucoma. Investig Ophthalmol Vis Sci 52:4422–4427
Jonas JB, Jonas SB, Jonas RA, Holbach L, Dai Y, Sun X, Panda-Jonas S (2012) Parapapillary atrophy: histological gamma zone and delta zone. PLoS One 7:e47237
Kim YW, Lee EJ, Kim TW, Kim M, Kim H (2014) Microstructure of beta-zone parapapillary atrophy and rate of retinal nerve fiber layer thinning in primary open-angle glaucoma. Ophthalmology 121:1341–1349
Dai Y, Jonas JB, Huang H, Wang M, Sun X (2013) Microstructure of parapapillary atrophy: beta zone and gamma zone. Invest Ophthalmol Vis Sci 54:2013–2018
Furlanetto RL, Park SC, Damle UJ, Sieminski SF, Kung Y, Siegal N, Liebmann JM, Ritch R (2013) Posterior displacement of the lamina cribrosa in glaucoma: in vivo interindividual and intereye comparisons. Investig Ophthalmol Vis Sci 54:4836–4842
Lee KM, Kim TW, Weinreb RN, Lee EJ, Girard MJ, Mari JM (2014) Anterior lamina cribrosa insertion in primary open-angle glaucoma patients and healthy subjects. PLoS One 9:e114935
Lee EJ, Kim TW, Weinreb RN, Park KH, Kim SH, Kim DM (2011) Visualization of the lamina cribrosa using enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 152:87–95
Lopilly Park HY, Lee NY, Choi JA, Park CK (2014) Measurement of scleral thickness using swept-source optical coherence tomography in patients with open-angle glaucoma and myopia. Am J Ophthalmol 157:876–884
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Ministry of Education, Culture, Sports, Science, and Technology (MEXT) in Japan provided financial support in the form of Innovative Techno-Hub for Integrated Medical Bio-Imaging of the Project for Developing Innovation Systems. The Japan Society for the Promotion of Science (JSPS) also provided financial support in the form of Grant-in-Aid for Scientific Research (25462713). The sponsors had no role in the design or conduct of this research. No funding was received for this research.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study adhered to the tenets of the 1964 Declaration of Helsinki its later amendments, and the study was approved by the Institutional Review Board and the Ethics Committee of Kyoto University Graduate School of Medicine.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1
Correlations between the temporal and nasal Bruch’s membrane opening (BMO)-scleral canal opening (SO) distances and the visual field mean deviation (MD) values. Both the temporal (a) and nasal (b) BMO-SO distances did not correlate with the MD values (a: R = −0.063, P = 0.542; b: R = −0.013, P = 0.901) (GIF 28 kb)
ESM 2
(WMV 1684 kb)
Rights and permissions
About this article
Cite this article
Hasegawa, T., Akagi, T., Hangai, M. et al. Structural dissociation of optic disc margin components with optic disc tilting: a spectral domain optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 254, 343–349 (2016). https://doi.org/10.1007/s00417-015-3210-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3210-0