Abstract
Background
Our aim was to analyze outcomes of idiopathic macular hole surgeries in relation to staging and the use of indocyanine green (ICG) or brilliant blue (BB) for internal limiting membrane (ILM) peel.
Methods
Baseline, surgical, and outcome data for 351 consecutive primary macular hole surgeries was prospectively collected using electronic medical record software between 2001 and 2011. The outcomes for these cases were analysed in relation to staging and the use of ICG (0.5 mg/ml) or BB for ILM peel.
Results
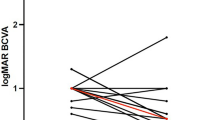
Mean age was 68.9 years (range 39–87) with 66.4 % females and 54.1 % right eyes. Follow-up duration was median 0.55 years. Vision was significantly improved from logMAR 0.97 (SD 0.45) (Snellen equivalent 20/185) preoperatively to 0.65 (SD 0.51) (20/90) at final follow-up. One hundred and eighteen patients had stage 2 macular holes, 185 stage 3, and 48 stage 4. Mean duration of symptoms varied with stage of hole: stage 2 0.53 years (SD 0.43), stage 3 0.79 years (SD 0.68), and stage 4 1.20 years (SD 1.26), p = 0.0002. Closure rates of the holes were significantly different, with stage 2 closing in 95.8 %, stage 3 in 73.0 %, and stage 4 in 56.3 %, p < 0.0001. At final follow-up, mean visual acuity (VA) was 0.42 (SD 0.33) (20/50) for stage 2, 0.75 (SD 0.53) (20/110) for stage 3, and 0.87 (SD 0.60) (20/145) for stage 4 holes, p < 0.0001.
Postoperative VA was 0.71 (SD 0.53) (20/100) for patients in whom ICG was used, and 0.52 (SD 0.43) (20/70) for BB, p = 0.003. The proportion of patients who achieved a closed hole was less for ICG (73.2 %) than BB (89.9 %), p = 0.0005. For those patients with stage 2 hole who achieved hole closure, mean improvement in VA was significantly better for BB (0.47, SD 0.36) than for ICG (0.30, SD 0.31), p = 0.01.
Conclusions
Macular hole stage is a useful measure to help predict the chance of postoperative hole closure and visual outcome. The relationship between duration of symptoms and increasing stage suggests macula hole patients require prompt referral for consideration of early surgery. Better visual outcomes were achieved with BB for ILM peel than with ICG.





Similar content being viewed by others
References
Kelly NE, Wendel RT (1991) Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol 109:654–659
Gass JD (2003) Idiopathic senile macular hole: its early stages and pathogenesis. 1988. Retina 23(6 Suppl):629–639
Gass JD (1995) Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 119:752–759
Jaycock PD, Bunce C, Xing W, Thomas D, Poon W, Gazzard G, Williamson TH, Laidlaw DA (2005) Outcomes of macular hole surgery: implications for surgical management and clinical governance. Eye 19:879–884
Da Mata AP, Burk SE, Riemann CD, Rosa RH Jr, Snyder ME, Petersen MR, Foster RE (2001) Indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for macular hole repair. Ophthalmology 108:1187–1192
Da Mata AP, Burk SE, Foster RE, Riemann CD, Petersen MR, Nehemy M, Augsburger JJ (2004) Long-term follow-up of indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for idiopathic macular hole repair. Ophthalmology 111:2246–2253
Dori D, Thoelen AM, Akalp F, Bernasconi PP, Messmer EP (2003) Anatomic and functional results of vitrectomy and long-term intraocular tamponade for stage 2 macular holes. Retina 23:57–63
Ezra E, Gregor ZJ (2004) Surgery for idiopathic full-thickness macular hole: two-year results of a randomized clinical trial comparing natural history, vitrectomy, and vitrectomy plus autologous serum: Morfields Macular Hole Study Group Report no. 1. Arch Ophthalmol 122:224–236
Gaudric A, Massin P, Paques M, Santiago PY, Guez JE, Le Gargasson JF, Mundler O, Drouet L (1995) Autologous platelet concentrate for the treatment of full-thickness macular holes. Graefes Arch Clin Exp Ophthalmol 233:549–554
Korobelnik JF, Hannouche D, Belayachi N, Branger M, Guez JE, Hoang-Xuan T (1996) Autologous platelet concentrate as an adjunct in macular hole healing: a pilot study. Ophthalmology 103:590–594
Minihan M, Goggin M, Cleary PE (1997) Surgical management of macular holes: results using gas tamponade alone, or in combination with autologous platelet concentrate, or transforming growth factor beta 2. Br J Ophthalmol 81:1073–1079
Paques M, Chastang C, Mathis A, Sahel J, Massin P, Dosquet C, Korobelnik JF, Le Gargasson JF, Gaudric A (1999) Effect of autologous platelet concentrate in surgery for idiopathic macular hole: results of a multicenter, double-masked, randomized trial. Platelets in Macular Hole Surgery Group. Ophthalmology 106:932–938
Banker AS, Freeman WR, Azen SP, Lai MY (1999) A multicentered clinical study of serum as adjuvant therapy for surgical treatment of macular holes. Vitrectomy for Macular Hole Study Group. Arch Ophthalmol 117:1499–1502
Wachtlin J, Jandeck C, Potthöfer S, Kellner U, Foerster MH (2003) Long-term results following pars plana vitrectomy with platelet concentrate in pediatric patients with traumatic macular hole. Am J Ophthalmol 136: 197–199
Lansing MB, Glaser BM, Liss H, Hanham A, Thompson JT, Sjaarda RN, Gordon AJ (1993) The effect of pars plana vitrectomy and transforming growth factor-beta 2 without epiretinal membrane peeling on full-thickness macular holes. Ophthalmology 100:868–871
Rosa RH Jr, Glaser BM, de la Cruz Z, Green WR (1996) Clinicopathologic correlation of an untreated macular hole and a macular hole treated by vitrectomy, transforming growth factor-beta 2, and gas tamponade. Am J Ophthalmol 122:853–863
Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R, Ravalico G, Macular Hole Surgery Study Group (2006) Internal limiting membrane removal during macular hole surgery: results of a multicenter retrospective study. Ophthalmology 113:1401–1410
Sheidow TG, Blinder KJ, Holekamp N, Joseph D, Shah G, Grand MG, Thomas MA, Bakal J, Sharma S (2003) Outcome results in macular hole surgery: an evaluation of internal limiting membrane peeling with and without indocyanine green. Ophthalmology 110:1697–1701
Lois N, Burr J, Norrie J, Vale L, Cook J, McDonald A, Boachie C, Ternent L, McPherson G, Full-thickness Macular Hole and Internal Limiting Membrane Peeling Study (FILMS) Group (2011) Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial. Invest Ophthalmol Vis Sci 52:1586–1589
Kadonosono K, Itoh N, Uchio E, Nakamura S, Ohno S (2000) Staining of internal limiting membrane in macular hole surgery. Arch Ophthalmol 118:1116–1118
Christensen UC, Krøyer K, Sander B, Larsen M, Henning V, Villumsen J, la Cour M (2009) Value of internal limiting membrane peeling in surgery for idiopathic macular hole stage 2 and 3: a randomised clinical trial. Br J Ophthalmol 93:1005–1015
Kwok AK, Lai TY, Man-Chan W, Woo DC (2003) Indocyanine green assisted retinal internal limiting membrane removal in stage 3 or 4 macular hole surgery. Br J Ophthalmol 87:71–74
Lee KL, Dean S, Guest S (2005) A comparison of outcomes after indocyanine green and trypan blue assisted internal limiting membrane peeling during macular hole surgery. Br J Ophthalmol 89:420–424
Engelbrecht NE, Freeman J, Sternberg P Jr, Aaberg TM Sr, Aaberg TM Jr, Martin DF, Sippy BD (2002) Retinal pigment epithelial changes after macular hole surgery with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 133:89–94
Ho JD, Tsai RJ, Chen SN, Chen HC (2003) Cytotoxicity of indocyanine green on retinal pigment epithelium: implications for macular hole surgery. Arch Ophthalmol 121:1423–1429
Ho JD, Tsai RJ, Chen SN, Chen HC (2004) Removal of sodium from the solvent reduces retinal pigment epithelium toxicity caused by indocyanine green: implications for macular hole surgery. Br J Ophthalmol 88:556–559
Ando F, Sasano K, Ohba N, Hirose H, Yasui O (2004) Anatomic and visual outcomes after indocyanine green-assisted peeling of the retinal internal limiting membrane in idiopathic macular hole surgery. Am J Ophthalmol 137:609–614
Gass CA, Haritoglou C, Schaumberger M, Kampik A (2003) Functional outcome of macular hole surgery with and without indocyanine green-assisted peeling of the internal limiting membrane. Graefes Arch Clin Exp Ophthalmol 241:716–720
Weinberger AW, Kirchhof B, Mazinani BE, Schrage NF (2001) Persistent indocyanine green (ICG) fluorescence 6 weeks after intraocular ICG administration for macular hole surgery. Graefes Arch Clin Exp Ophthalmol 239:388–390
Ciardella AP, Schiff W, Barile G, Vidne O, Sparrow J, Langton K, Chang S (2003) Persistent indocyanine green fluorescence after vitrectomy for macular hole. Am J Ophthalmol 136:174–177
Haritoglou C, Gandorfer A, Gass CA, Schaumberger M, Ulbig MW, Kampik A (2002) Indocyanine green-assisted peeling of the internal limiting membrane in macular hole surgery affects visual outcome: a clinicopathologic correlation. Am J Ophthalmol 134:836–841
Horio N, Horiguchi M (2004) Effect on visual outcome after macular hole surgery when staining the internal limiting membrane with indocyanine green dye. Arch Ophthalmol 122:992–996
Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T, Kubota T, Ishibashi T (2006) Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G-assisted membrane peeling. Retina 26:631–636
Enaida H, Hisatomi T, Goto Y, Hata Y, Ueno A, Miura M, Kubota T, Ishibashi T (2006) Preclinical investigation of internal limiting membrane staining and peeling using intravitreal brilliant blue G. Retina 26:623–630
Ueno A, Hisatomi T, Enaida H, Kagimoto T, Mochizuki Y, Goto Y, Kubota T, Hata Y, Ishibashi T (2007) Biocompatibility of brilliant blue G in a rat model of subretinal injection. Retina 27:499–504
Remy M, Thaler S, Schumann RG, May CA, Fiedorowicz M, Schuettauf F, Grüterich M, Priglinger SG, Nentwich MM, Kampik A, Haritoglou C (2008) An in vivo evaluation of Brilliant Blue G in animals and humans. Br J Ophthalmol 92:1142–1147
Schumann RG, Remy M, Grueterich M, Gandorfer A, Haritoglou C (2008) How it appears: electron microscopic evaluation of internal limiting membrane specimens obtained during brilliant blue G assisted macular hole surgery. Br J Ophthalmol 92:330–331
Schumann RG, Gandorfer A, Priglinger SG, Kampik A, Haritoglou C (2009) Vital dyes for macular surgery: a comparative electron microscopy study of the internal limiting membrane. Retina 29:669–676
Baba T, Hagiwara A, Sato E, Arai M, Oshitari T, Yamamoto S (2012) Comparison of vitrectomy with brilliant blue G or indocyanine green on retinal microstructure and function of eyes with macular hole. Ophthalmology 119:2609–2615
Williamson TH (2008) Vitreoretinal surgery. Springer, Berlin Heidelberg New York
Holladay JT (1997) Proper method for calculating average visual acuity. J Refract Surg 13:388–391
Ruby AJ, Williams DF, Grand MG, Thomas MA, Meredith TA, Boniuk I, Olk RJ (1994) Pars plana vitrectomy for treatment of stage 2 macular holes. Arch Ophthalmol 112:359–364
Freeman WR, Azen SP, Kim JW, El-Haig W, Mishell DR III, Bailey I (1997) Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol 115:11–21
Leonard RE 2nd, Smiddy WE, Flynn HW Jr, Feuer W (1997) Long-term visual outcomes in patients with successful macular hole surgery. Ophthalmology 104:1648–1652
Stec LA, Ross RD, Williams GA, Trese MT, Margherio RR, Cox MS Jr (2004) Vitrectomy for chronic macular holes. Retina 24:341–347
Gupta B, Laidlaw DA, Williamson TH, Shah SP, Wong R, Wren S (2009) Predicting visual success in macular hole surgery. Br J Ophthalmol 93:1488–1491
Conflict of interest
There are no financial interests to declare or funding bodies for this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have full control of all primary data, and agree to allow Graefe's Archive for Clinical and Experimental Ophthalmology to review data upon request.
Rights and permissions
About this article
Cite this article
Williamson, T.H., Lee, E. Idiopathic macular hole: analysis of visual outcomes and the use of indocyanine green or brilliant blue for internal limiting membrane peel. Graefes Arch Clin Exp Ophthalmol 252, 395–400 (2014). https://doi.org/10.1007/s00417-013-2477-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2477-2