Abstract
Background
When performing ultra-thin Descemet's stripping automated endothelial keratoplasty (UT-DSAEK), the quality of the stromal interface and stromal thickness seem to be critical for visual outcome. The aim of this study was to investigate whether additional osmotic deswelling prior to UT-DSAEK improves the quality of the cut surface and leads to a more reliable and deeper cut in UT-DSAEK (“OSMO-UT-DSAEK”).
Methods
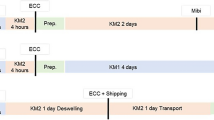
Seventeen human donor corneas not usable for transplantation were used in this experiment. After standard deswelling with culture Medium II, ten corneas were randomly assigned to be additionally deswollen within THIN-C medium. The other remaining seven corneas were put back into culture Medium II. All corneas were placed in an artificial anterior chamber system (Moria); a double path cutting procedure using a microkeratome (Moria) was then performed. Corneal thickness was measured by ultrasound biomicroscopy and in paraffin-embedded slides, followed by histological grading of the cut surface.
Results
Stromal interface smoothness significantly improved after preconditioning in THIN-C medium (Pearson P = 0.019). The correlation of the corneal thickness obtained by UBM (mean 706 ± SD 208 μm) and histology (mean 530 ± SD 159 μm) was not significant (Pearson r = 0.11, P > 0.05, mean difference 247, 95 % CI [+50;+304]). We found no significant correlation between the microkeratome setting and the actual thickness of the lenticule measured in histological analysis in both media as well as for the first and second cut (first cut: Pearson r = 0.9, P = 0.1, 95 % CI [−10;+96], second cut: Pearson r = 0.9, P = 0.4, 95 % CI [−10;+22]).
Conclusion
Preconditioning of corneas with THIN-C medium significantly improved the quality of the graft interface in UT-DSAEK, but did not significantly improve the cut precision of the microkeratome.




Similar content being viewed by others
References
Bahar I, Kaiserman I, McAllum P, Slomovic A, Rootman D (2008) Comparison of posterior lamellar keratoplasty techniques to penetrating keratoplasty. Ophthalmology 115:1525–1533
Dapena I, Ham L, Melles GR (2009) Endothelial keratoplasty: DSEK/DSAEK or DMEK—the thinner the better? Curr Opin Ophthalmol 20:299–307
Terry MA, Straiko MD, Goshe JM, Li JY, Davis-Boozer D (2012) Descemet’s stripping automated endothelial keratoplasty: the tenuous relationship between donor thickness and postoperative vision. Ophthalmology 119:1988–1996
Heindl LM, Riss S, Adler W, Bucher F, Hos D, Cursiefen C (2013) Split cornea transplantation: Relationship between storage time of split donor tissue and outcome. Ophthalmology 120(5):899–907. doi:10.1016/j.ophtha.2012.11.012
Tourtas T, Laaser K, Bachmann BO, Cursiefen C, Kruse FE (2012) Descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty. Am J Ophthalmol 153(1082–1090):e1082
Hjortdal J, Ehlers N (2009) Descemet’s stripping automated endothelial keratoplasty and penetrating keratoplasty for Fuchs’ endothelial dystrophy. Acta Ophthalmol 87:310–314
Happ DM, Lewis DA, Eng KH, Potter HA, Neekhra A, Croasdale CR, Hardten DR, Nehls S, Eide M, Rowe J, Khedr S, Albert DM (2012) Postoperative visual acuity in patients with Fuchs dystrophy undergoing Descemet membrane-stripping automated endothelial keratoplasty: correlation with the severity of histologic changes. Arch Ophthalmol 130:33–38
Cursiefen C, Kruse FE (2009) Descemet’s stripping automated endothelial keratoplasty (DSAEK). Ophthalmologe 106:939–952, quiz 953
Cursiefen C (2013) Descemet membrane endothelial keratoplasty: the taming of the shrew. JAMA Ophthalmol 131:88–89
Heindl LM, Hofmann-Rummelt C, Schlotzer-Schrehardt U, Kruse FE, Cursiefen C (2008) Histologic analysis of Descemet stripping in posterior lamellar keratoplasty. Arch Ophthalmol 126:461–464
Guerra FP, Anshu A, Price MO, Price FW (2011) Endothelial keratoplasty: fellow eyes comparison of Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty. Cornea 30:1382–1386
Van Cleynenbreugel H, Remeijer L, Hillenaar T (2011) Descemet stripping automated endothelial keratoplasty: effect of intraoperative lenticule thickness on visual outcome and endothelial cell density. Cornea 30:1195–1200
Uchino Y, Shimmura S, Yamaguchi T, Kawakita T, Matsumoto Y, Negishi K, Tsubota K (2011) Comparison of corneal thickness and haze in DSAEK and penetrating keratoplasty. Cornea 30:287–290
Jun B, Kuo AN, Afshari NA, Carlson AN, Kim T (2009) Refractive change after descemet stripping automated endothelial keratoplasty surgery and its correlation with graft thickness and diameter. Cornea 28:19–23
Pocobelli R, Amici C, D’Amato Tothova J, Macaluso C (2012) Monitoring of endothelial cell density during simulation of DSAEK Phases in vitro using THIN-C deswelling medium and two different glides for endothelium insertion. EEBA, Rotterdam
Tehrani M, Schafer S, Dick HB (2004) Evaluation of cut quality using the Amadeus microkeratome with different settings. J Cataract Refract Surg 30:2415–2419
Vinciguerra P, Azzolini M, Radice P, Sborgia M, De Molfetta V (1998) A method for examining surface and interface irregularities after photorefractive keratectomy and laser in situ keratomileusis: predictor of optical and functional outcomes. J Refract Surg 14:S204–206
Wirbelauer C, Winkler J, Bastian GO, Haberle H, Pham DT (2002) Histopathological correlation of corneal diseases with optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 240:727–734
Ehlers JP, McNutt SA, Kaiser PK, Srivastava SK (2013) Contrast-enhanced intraoperative optical coherence tomography. Br J Ophthalmol. doi:10.1136/bjophthalmol-2012-303048
Steven C, Velten K, Lankenau E, Krug M, Oelckers S, Heindl L, Gehlsen U, Huettmann G, Cursiefen C (2013) Optimizing Descemet’s membrane endothelial keratoplasty using intraoperative optical coherence tomography. Arch Ophthalmol [in press]
Amato D, Lombardo M, Oddone F, Nubile M, Colabelli Gisoldi RA, Villani CM, Yoo S, Parel JM, Pocobelli A (2011) Evaluation of a new method for the measurement of corneal thickness in eye bank posterior corneal lenticules using anterior segment optical coherence tomography. Br J Ophthalmol 95:580–584
Wolf A, von Jagow B, Kook D, Messmer EM, Lackerbauer CA, Kampik A, Kohnen T, Grueterich M (2012) Evaluation of interface quality in organ-cultured lamellar corneal transplants. Clin Ophthalmol 6:967–972
Wolf AH, Welge-Lussen UC, Priglinger S, Kook D, Grueterich M, Hartmann K, Kampik A, Neubauer AS (2009) Optimizing the deswelling process of organ-cultured corneas. Cornea 28:524–529
Acknowledgments
Martina Becker, MTA, and H. Simons, Department of Ophthalmology, University of Cologne, provided excellent technical support.
Financial support
DFG (Cu 47/-1), DFG (Cu 47/6-1), DFG (HE 6743/2-1), GEROK Programm Universität Köln, Köln Fortune, Ruth und Helmut Lingen Stiftung Köln
Conflict of interest
None of the authors has a financial or proprietary interest in any material or method mentioned in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bucher, F., Roters, S., Mellein, A. et al. “OSMO-UT-DSAEK” using THIN-C medium. Graefes Arch Clin Exp Ophthalmol 251, 2181–2185 (2013). https://doi.org/10.1007/s00417-013-2434-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2434-0