Abstract
Purpose
To determine whether central corneal thinning and flattening can be achieved by intrastromal photodisruption using a femtosecond (fs) laser.
Setting
Institute of Clinical Neuroanatomy, Goethe-University, Frankfurt am Main, Germany.
Methods
Fourteen horizontal, parallel intrastromal cuts were performed on rabbit eyes using a fs laser. Full-grown rabbits (group 1; ten eyes) received bilateral treatment. Growing rabbits (group 2) received unilateral treatment (four eyes). Slit-lamp examination, pachymetry, and keratometry were performed on day 9, 31 and 86 (group 1) or on day 12, 29, 69, 176 and 318 (group 2) after surgery.
Results
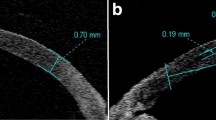
Nine days after treatment, corneal swelling was present and a slight increase of mean corneal thickness (group 1: +4.40 ± 5.56 μm) as well as a steeper mean corneal curvature (group 1: −0.18 ± 0.02 mm) were observed. In contrast, 1 month after tissue photodisruption corneas showed an average decrease of thickness (group 2: −21.0 ± 2.5 μm). By 6 months post-treatment, a further decrease (group 2: −36.3 ± 6.9 μm) was seen that remained stable for the rest of the observation period. At 176 days post-treatment, a decrease of corneal curvature (group 2: −0.21 ± 0.10 mm) was found. Slit-lamp examination revealed a transparent cornea. At the site of intrastromal photodisruption a narrow band of increased reflectivity could be detected.
Conclusions
Corneal thinning can be reliably achieved using intrastromal tissue modeling with a fs laser. Tissue modeling was accompanied by a transient opacity and irregularity of the corneal surface.



Similar content being viewed by others
References
Sakimoto T, Rosenblatt MI, Azar DT (2006) Laser eye surgery for refractive errors. Lancet 367:1432–1447
Lin RT, Maloney RK (1999) Flap complications associated with lamellar refractive surgery. Am J Ophthalmol 127:129–136
Stulting RD, Carr JD, Thompson KP, Waring GO 3rd, Wiley WM, Walker JG (1999) Complications of laser in situ keratomileusis for the correction of myopia. Ophthalmology 106:13–20
Møller-Pedersen T (2003) On the structural origin of refractive instability and corneal haze after excimer laser keratectomy for myopia. Acta Ophthalmol Scand Suppl:1–20
Soong HK, Malta JB (2009) Femtosecond lasers in ophthalmology. Am J Ophthalmol 147:189–197
Lubatschowski H, Maatz G, Heisterkamp A, Hetzel U, Drommer W, Welling H, Ertmer W (2000) Application of ultrashort laser pulses for intrastromal refractive surgery. Graefes Arch Clin Exp Ophthalmol 238:33–39
Meltendorf C, Burbach GJ, Bühren J, Bug R, Ohrloff C, Deller T (2007) Corneal femtosecond laser keratotomy results in isolated stromal injury and favorable wound-healing response. Investig Ophthalmol Vis Sci 48:2068–2075
Habib MS, Speaker MG, McCormick SA, Kaiser R (1995) Wound healing following intrastromal photorefractive keratectomy with the Nd:YLF picosecond laser in the cat. J Refract Surg 11:442–447
Habib MS, Speaker MG, Kaiser R, Juhasz T (1995) Myopic intrastromal photorefractive keratectomy with the neodymium-yttrium lithium fluoride picosecond laser in the cat cornea. Arch Ophthalmol 113:499–505
Sletten KR, Yen KG, Sayegh S, Loesel F, Eckhoff C, Horvath C, Meunier M, Juhasz T, Kurtz RM (1999) An in vivo model of femtosecond laser intrastromal refractive surgery. Ophthalmic Surg Lasers 30:742–749
Ratkay-Traub I, Ferincz IE, Juhasz T, Kurtz RM, Krueger RR (2003) First clinical results with the femtosecond neodymium-glass laser in refractive surgery. J Refract Surg 19:94–103
Vogel A, Gunther T, Asiyo-Vogel M, Birngruber R (1997) Factors determining the refractive effects of intrastromal photorefractive keratectomy with the picosecond laser. J Cataract Refract Surg 23:1301–1310
Vogel A, Gunther T, Asiyo-Vogel M, Birngruber R (1997) Studies of the development of refractive effects in intrastromal refractive corneal surgery with the picosecond laser. Ophthalmologe 94:467–474
Juhasz T, Frieder H, Kurtz RM, Horvath C, Bille JF, Mourou G (1999) Corneal refractive surgery with femtosecond lasers. IEEE J Sel Top Quant 5:902–910
Zhang ZY, Chu RY, Zhou XT, Dai JH, Sun XH, Hoffman MR, Zhang XR (2009) Morphologic and histopathologic changes in the rabbit cornea produced by femtosecond laser-assisted multilayer intrastromal ablation. Investig Ophthalmol Vis Sci 50:2147–2153
Jue B, Maurice DM (1986) The mechanical properties of the rabbit and human cornea. J Biomech 19:847–853
Meltendorf C, Burbach GJ, Ohrloff C, Ghebremedhin E, Deller T (2009) Intrastromal keratotomy with femtosecond laser avoids profibrotic TGF-beta1 induction. Investig Ophthalmol Vis Sci 50:3688–3695
Holzer MP, Mannsfeld A, Ehmer A, Auffarth GU (2009) Early outcomes of INTRACOR femtosecond laser treatment for presbyopia. J Refract Surg 25:855–861
Acknowledgments
The authors thank Tobias Kuhn for invaluable technical assistance and for helpful comments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. von Pape is a former employee of an involved company.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 25.5 kb)
Rights and permissions
About this article
Cite this article
Meltendorf, C., Deller, T., Ackermann, H. et al. Corneal intrastromal tissue modeling with the femtosecond laser. Graefes Arch Clin Exp Ophthalmol 249, 1661–1666 (2011). https://doi.org/10.1007/s00417-011-1701-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-011-1701-1