Abstract
Background
Non-obese diabetic (NOD) mice are a commonly used murine model for the study of Sjögren’s syndrome. However, variations in susceptibility to the disease among the mice has often yielded less stable results. Based on the correlation between the pathological changes and the tear tests, we attempt to establish a simple screening procedure to assure the validity of experimental results by excluding those mice with poor susceptibility to dry eyes.
Methods
Seventy male NOD mice were recruited. The tear film break-up test (BUT) and the phenol red cotton thread test (CTT) were implemented while the mice were under anesthesia. The mice were divided into four groups (grades 1 to 4) based on their BUT readings, and four similar groups based on CTT measurements. Tear samples in each grade were collected for IL-1β detection with ELISA. The lacrimal glands and conjunctiva of the mice were used to detect the levels of leucocyte common antigen (LCA). LCA-Positive staining was considered as the “gold standard” in the receiver operating characteristic curve (ROC curve) analysis. C57BL/6 mice were used as wild-type controls.
Results
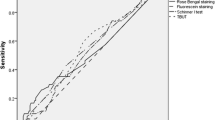
There were 13 (18.57%), 43 (61.43%), 10 (14.29%) and 4 (5.71%) mice in grades 1, 2, 3 and 4 by BUT test, and 34 (48.57%), 15 (21.43%), 14 (20.00%) and 7 (10.00%) in grades 1, 2, 3 and 4 by CTT test respectively. Fifty-one out of the 70 mice (72.86%) were detected LCA-positive, and they were mainly in grades 1 and 2 of both the BUT and CCT grading systems. ELISA showed significant variances of IL-β levels among the four groups (p < 0.01), with much lower IL-β levels in group 3 and 4 when both BUT and CTT were used for grouping. The tear IL-β level in the wild-type mice was similar to those of the grade 4 mice, using either BUT or CTT for grouping. The ROC curve analysis provided optimal cutting lines, which were 2 seconds in BUT readings and 4 mm/min in CTT measurements respectively.
Conclusion
BUT and CTT tests are useful methods in screening high susceptible NOD mice. Cutting lines at BUT ≤2 seconds and CTT ≤4 mm/min provide a good balance between the assurance of susceptibility and the maximization of use of NOD mice for the study of Sjögren’s syndrome.



Similar content being viewed by others
References
Behrman HT, Lee KK (1950) Sjogren’s syndrome. Arch Derm Syphilol 61:63–79
Groom J, Kalled SL, Cutler AH, Olson C, Woodcock SA, Schneider P et al (2002) Association of BAFF/BLyS overexpression and altered B cell differentiation with Sjogren’s syndrome. J Clin Invest 109:59–68
Haneji N, Hamano H, Yanagi K, Hayashi Y (1994) A new animal model for primary Sjogren’s syndrome in NFS/sld mutant mice. J Immunol 153:2769–2777
Humphreys-Beher MG, Brinkley L, Purushotham KR, Wang PL, Nakagawa Y, Dusek D et al (1993) Characterization of antinuclear autoantibodies present in the serum from nonobese diabetic (NOD) mice. Clin Immunol Immunopathol 68:350–356, doi:10.1006/clin.1993.1137
Humphreys-Beher MG, Hu Y, Nakagawa Y, Wang PL, Purushotham KR (1994) Utilization of the non-obese diabetic (NOD) mouse as an animal model for the study of secondary Sjogren’s syndrome. Adv Exp Med Biol 350:631–636
Kikutani H, Makino S (1992) The murine autoimmune diabetes model: NOD and related strains. Adv Immunol 51:285–322, doi:10.1016/S0065–2776(08)60490–3
Li H, Dai M, Zhuang Y (2004) A T cell intrinsic role of Id3 in a mouse model for primary Sjogren’s syndrome. Immunity 21:551–560, doi:10.1016/j.immuni.2004.08.013
Lodde BM, Mineshiba F, Kok MR, Wang J, Zheng C, Schmidt M et al (2006) NOD mouse model for Sjogren’s syndrome: lack of longitudinal stability. Oral Dis 12:566–572, doi:10.1111/j.1601–0825.2006.01241.x
Miyagawa J, Hanafusa T, Miyazaki A, Yamada K, Fujino-Kurihara H, Nakajima H et al (1986) Ultrastructural and immunocytochemical aspects of lymphocytic submandibulitis in the non-obese diabetic (NOD) mouse. Virchows Arch B Cell Pathol Incl Mol Pathol 51:215–225, doi:10.1007/BF02899031
Moyes DL, Martin A, Sawcer S, Temperton N, Worthington J, Griffiths DJ et al (2005) The distribution of the endogenous retroviruses HERV-K113 and HERV-K115 in health and disease. Genomics 86:337–341, doi:10.1016/j.ygeno.2005.06.004
Robinson CP, Cornelius J, Bounous DE, Yamamoto H, Humphreys-Beher MG, Peck AB (1998) Characterization of the changing lymphocyte populations and cytokine expression in the exocrine tissues of autoimmune NOD mice. Autoimmunity 27:29–44, doi:10.3109/08916939809008035
Robinson CP, Yamachika S, Bounous DI, Brayer J, Jonsson R, Holmdahl R et al (1998) A novel NOD-derived murine model of primary Sjogren’s syndrome. Arthritis Rheum 41:150–156, doi:10.1002/1529–0131(199801)41:1<150::AID-ART18>3.0.CO;2-T
Saegusa J, Kubota H (1997) Sialadenitis in IQI/Jic mice: a new animal model of Sjogren’s syndrome. J Vet Med Sci 59:897–903, doi:10.1292/jvms.59.897
Skarstein K, Wahren M, Zaura E, Hattori M, Jonsson R (1995) Characterization of T cell receptor repertoire and anti-Ro/SSA autoantibodies in relation to sialadenitis of NOD mice. Autoimmunity 22:9–16, doi:10.3109/08916939508995294
Song XJ, Li DQ, Farley W, Luo LH, Heuckeroth RO, Milbrandt J et al (2003) Neurturin-deficient mice develop dry eye and keratoconjunctivitis sicca. Invest Ophthalmol Vis Sci 44:4223–4229, doi:10.1167/iovs.02–1319
Soyfoo MS, Steinfeld S, Delporte C (2007) Usefulness of mouse models to study the pathogenesis of Sjogren’s syndrome. Oral Dis 13:366–375, doi:10.1111/j.1601–0825.2007.01376.x
Takahashi M, Ishimaru N, Yanagi K, Haneji N, Saito I, Hayashi Y (1997) High incidence of autoimmune dacryoadenitis in male non-obese diabetic (NOD) mice depending on sex steroid. Clin Exp Immunol 109:555–561, doi:10.1046/j.1365–2249.1997.4691368.x
Toda I, Sullivan BD, Rocha EM, Da Silveira LA, Wickham LA, Sullivan DA (1999) Impact of gender on exocrine gland inflammation in mouse models of Sjogren’s syndrome. Exp Eye Res 69:355–366, doi:10.1006/exer.1999.0715
Van Blokland SC, Versnel MA (2002) Pathogenesis of Sjogren’s syndrome: characteristics of different mouse models for autoimmune exocrinopathy. Clin Immunol 103:111–124, doi:10.1006/clim.2002.5189
Venables PJ, Rigby SP (1997) Viruses in the etiopathogenesis of Sjogren’s syndrome. J Rheumatol Suppl 50:3–5
Wicker LS, Todd JA, Peterson LB (1995) Genetic control of autoimmune diabetes in the NOD mouse. Annu Rev Immunol 13:179–200, doi:10.1146/annurev.iy.13.040195.001143
Willoughby CE, Baker K, Kaye SB, Carey P, O’Donnell N, Field A et al (2002) Epstein-Barr virus (types 1 and 2) in the tear film in Sjogren’s syndrome and HIV infection. J Med Virol 68:378–383, doi:10.1002/jmv.10214
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Xiao, W., Wu, Y., Zhang, J. et al. Selecting highly sensitive non-obese diabetic mice for improving the study of Sjögren’s syndrome. Graefes Arch Clin Exp Ophthalmol 247, 59–66 (2009). https://doi.org/10.1007/s00417-008-0941-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-0941-1