Abstract
Background
To compare visual outcome and ocular complications of transscleral local resection (TSR) with those of iodine-125 plaque brachytherapy (IBT) for uveal melanomas categorised as large because of tumour height.
Methods
Retrospective study of 87 patients with a uveal melanoma ≤16 mm by largest basal diameter (median, 12.6 vs 14.0 mm for TSR and IBT, respectively) and large by height (median, 11.0 vs 10.6 mm) by the Collaborative Ocular Melanoma Study (COMS) criteria. Thirty-three patients underwent TSR in the United Kingdom and 54 underwent IBT in Finland. Loss of 20/65 and 20/400 vision, local tumour recurrence, cataract, iris neovascularization, glaucoma, maculopathy, optic neuropathy, persistent retinal detachment, and vitreous haemorrhage were analysed using competing risks and logistic regression to control for confounders.
Results
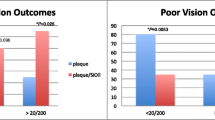
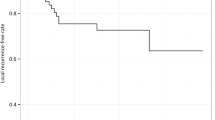
All patients save one managed with TSR lost 20/70 vision within 3 years. The 2-year cumulative incidence of losing 20/400 vision was 60% (95% CI, 35–75) for TSR and 75% (95% CI, 59–86) for IBT. The 5-year incidence of local tumour recurrence was 41% (95% CI, 17–63) after TSR and 7% (95% CI, 2–17) after IBT. Glaucoma and optic neuropathy were rare after TSR. Cataract, maculopathy, retinal detachment, and vitreous haemorrhage were common after either treatment. The number of patients needed to treat with TSR instead of IBT was four for one additional patient to benefit by avoiding loss of visual acuity 20/400 for at least 2 years, and the corresponding number was three for one additional patient to experience a local recurrence from TSR.
Conclusions
If TSR is further evaluated as an alternative to IBT in avoiding blindness of an eye with a ciliochoroidal melanoma categorised as large by COMS criteria because of its height, special emphasis must be given to increased risk of local tumour recurrence.






Similar content being viewed by others
References
Altman DG (1998) Confidence intervals for the number needed to treat. BMJ 317:1309–1312
Bechrakis NE, Bornfeld N, Zoller I, Foerster MH (2002) Iodine 125 plaque brachytherapy versus transscleral tumor resection in the treatment of large uveal melanomas. Ophthalmology 109:1855–1861
Bender R (2001) Calculating confidence intervals for the number needed to treat. Control Clin Trials 22:102–110
Char DH, Bove R, Phillips TL (2003) Laser and proton radiation to reduce uveal melanoma-associated exudative retinal detachments. Am J Ophthalmol 136:180–182
Char DH, Miller T, Crawford JB (2004) Analysis of melanoma cell type in uveal melanoma following treatment failure. Am J Ophthalmol 138:543–546
Collaborative Ocular Melanoma Study Group (1998) The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma I: characteristics of patients enrolled and not enrolled. COMS report no. 9. Am J Ophthalmol 125:767–778
Damato B (1997) Adjunctive plaque radiotherapy after local resection of uveal melanoma. Front Radiat Ther Oncol 30:123–132
Damato B, Groenewald CP, McGalliard JN, Wong D (2002) Rhegmatogenous retinal detachment after transscleral local resection of choroidal melanoma. Ophthalmology 109:2137–2143
Damato B, Lecuona K (2004) Conservation of eyes with choroidal melanoma by a multimodality approach to treatment: an audit of 1632 patients. Ophthalmology 111:977–983
Damato BE, Paul J, Foulds WS (1993) Predictive factors of visual outcome after local resection of choroidal melanoma. Br J Ophthalmol 77:616–623
Damato BE, Paul J, Foulds WS (1996) Risk factors for residual and recurrent uveal melanoma after trans-scleral local resection. Br J Ophthalmol 80:102–108
De Potter P, Shields CL, Shields JA, Cater JR, Brady LW (1996) Plaque radiotherapy for juxtapapillary choroidal melanoma. Visual acuity and survival outcome. Arch Ophthalmol 114:1357–1365
Detorakis ET, Engstrom RE Jr, Wallace R, Straatsma BR (2005) Iris and anterior chamber angle neovascularization after iodine 125 brachytherapy for uveal melanoma. Ophthalmology 112:505–510
Diener-West M, Earle JD, Fine SL, Hawkins BS, Moy CS, Reynolds SM, Schachat AP, Straatsma BR, The Collaborative Ocular Melanoma Study Group. (2001) The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, III: initial mortality findings. COMS report no. 18. Arch Ophthalmol 119:969–982
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Gooley TA, Leisenring W, Crowley J, Storer BE (2001) Why Kaplan-Meier fails and cumulative incidence succeeds when estimating failure probabilities in the presence of competing risks. In: Crowley J (eds) Handbook of statistics in clinical oncology. Marcel Dekker, New York, pp 513–523
Gragoudas ES, Li W, Lane AM, Munzenrider J, Egan KM (1999) Risk factors for radiation maculopathy and papillopathy after intraocular irradiation. Ophthalmology 106:1571–1578
Gunduz K, Shields CL, Shields JA, Cater J, Freire JE, Brady LW (1999) Plaque radiotherapy of uveal melanoma with predominant ciliary body involvement. Arch Ophthalmol 117:170–177
Gunduz K, Shields CL, Shields JA, Cater J, Freire JE, Brady LW (1999) Radiation complications and tumor control after plaque radiotherapy of choroidal melanoma with macular involvement. Am J Ophthalmol 127:579–589
Gunduz K, Shields CL, Shields JA, Cater J, Freire JE, Brady LW (1999) Radiation retinopathy following plaque radiotherapy for posterior uveal melanoma. Arch Ophthalmol 117:609–614
Hair JF Jr, Tatham RL, Anderson RE, Black WC (1998) Multivariate data analysis, 5th. Prentice-Hall, Upper Saddle River
Harbour JW, Char DH, Kroll S, Quivey JM, Castro J (1997) Metastatic risk for distinct patterns of postirradiation local recurrence of posterior uveal melanoma. Ophthalmology 104:1785–1792
Kivelä T, Puusaari I, Damato B (2003) Transscleral resection vs. iodine brachytherapy for choroidal malignant melanomas 6 millimeters or more in thickness: a matched case-control study. Ophthalmology 110:2235–2244
Kivelä T, Eskelin S, Mäkitie T, Summanen P (2001) Exudative retinal detachment from malignant uveal melanoma: predictors and prognostic significance. Invest Ophthalmol Vis Sci 42:2085–2093
Melia BM, Abramson DH, Albert DM, Boldt HC, Earle JD, Hanson WF, Montague P, Moy CS, Schachat AP, Simpson ER, Straatsma BR, Vine AK, Weingeist TA, Collaborative Ocular Melanoma Study Group (2001) Collaborative Ocular Melanoma Study (COMS) randomized trial of I-125 brachytherapy for medium choroidal melanoma. I. Visual acuity after 3 years. COMS report no. 16. Ophthalmology 108:348–366
Packer S, Stoller S, Lesser ML, Mandel FS, Finger PT (1992) Long-term results of iodine 125 irradiation of uveal melanoma. Ophthalmology 99:767–773
Parmar MKB, Machin D (1995) Survival analysis. A practical approach. Wiley, Chichester
Puusaari I, Heikkonen J, Kivela T (2004) Effect of radiation dose on ocular complications after iodine brachytherapy for large uveal melanoma: empirical data and simulation of collimating plaques. Invest Ophthalmol Vis Sci 45:3425–3434
Puusaari I, Heikkonen J, Kivela T (2004) Ocular complications after iodine brachytherapy for large uveal melanomas. Ophthalmology 111:1768–1777
Puusaari I, Heikkonen J, Summanen P, Tarkkanen A, Kivelä T (2003) Iodine brachytherapy as an alternative to enucleation for large uveal melanomas. Ophthalmology 110:2223–2234
Shields CL, Naseripour M, Cater J, Shields JA, Demirci H, Youseff A, Freire J (2002) Plaque radiotherapy for large posterior uveal melanomas (> or=8-mm thick) in 354 consecutive patients. Ophthalmology 109:1838–1849
Shields CL, Shields JA, Cater J, Gunduz K, Miyamoto C, Micaily B, Brady LW (2000) Plaque radiotherapy for uveal melanoma: long-term visual outcome in 1106 consecutive patients. Arch Ophthalmol 118:1219–1228
Therneau TM, Grambsch PM (2000) Modeling survival data: extending the Cox model. Springer, New York
Acknowledgements
This work was supported by The Finnish Eye Foundation, The Eye and Tissue Bank Foundation, Sigrid Jusélius Foundation, Finnish Cultural Foundation, The Paulo Foundation, The Friends of the Blind, The Finnish Medical Foundation, Biopattern, and The Helsinki University Central Hospital Research Fund (TYH3203, TYH5210), Helsinki, Finland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puusaari, I., Damato, B. & Kivelä, T. Transscleral local resection versus iodine brachytherapy for uveal melanomas that are large because of tumour height. Graefe's Arch Clin Exp Ophthalmol 245, 522–533 (2007). https://doi.org/10.1007/s00417-006-0461-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-006-0461-9