Abstract
Background
Endovascular therapy (EVT) has been proven beneficial for treating acute ischemic strokes (AIS) with large vessel occlusion (LVO). Recent trials of DAWN and DEFUSE-3 have extended the treatment window to 6–24 h, sparking investigations into EVT outcomes for patients not eligible for DAWN/DEFUSE-3 criteria.
Purpose
To assess the outcomes of endovascular therapy (EVT) for late-window anterior circulation large vessel occlusion (LVO) in acute ischemic stroke patients, comparing DAWN/DEFUSE-3 eligible (DD) and ineligible (NDND) groups.
Methods
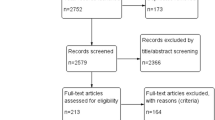
This systematic review and meta-analysis examined EVT outcomes for patients with late-window anterior circulation LVO beyond 6 h. We categorized patients as DAWN/DEFUSE-3 eligible (DD) and ineligible (NDND). Our search covered PubMed, Embase, Web of Science, and Scopus. A total of 464 records were initially identified. After duplicate removal, 298 studies were screened. Nine studies were included and analyzed. Our analysis focused on study characteristics, baseline comparisons, risk of bias, and outcomes.
Results
Baseline characteristics showed comparable age, gender, most comorbidities, NIHSS score, and ASPECTS between DAWN/DEFUSE-3 eligible (DD) and ineligible (NDND) patients. NDND patients’ history showed a higher rate of atrial fibrillation and larger infarct volumes on baseline imaging. Successful reperfusion rates (TICI 2b-3) were similar between DD and NDND with 354 out of 469 in the DD group and 364 out of 459 in the NDND group (OR = 0.86; 95% CI 0.40, 1.84; p = 0.689), though with significant heterogeneity (I2 = 73%; P = 0.002). The proportion of patients with distal occlusions was significantly higher in the NDND group as compared to the DD group (137 (39.4%) of 347 patients versus 47 (11%) of 428 patients, respectively), with significant heterogeneity across studies (I2 = 85%, p = 0.023). Functional independence at 90 days (mRS 0–2) showed no significant difference between groups with 259 out of 802 in the DD group and 197 out of 668 in the NDND group (OR = 1.12; 95% CI 0.77, 1.63; p = 0.552) but also exhibited notable heterogeneity (I2 = 46%, p = 0.063). Symptomatic intracranial hemorrhage (sICH) rates were lower in DD with 14 out of 309 in the DD group and 47 out of 400 in NDND group (OR = 0.49; 95% CI 0.25, 0.93; p = 0.029) as compared to the NDND patients, showing no heterogeneity (I2 = 0%, p = 0.552). 90-day mortality was lower in DD with 43 out of 304 in the DD group and 107 out of 399 in the NDND group (OR = 0.55; 95% CI 0.37, 0.82; p = 0.004) as compared to NDND patients, with no significant heterogeneity (I2 = 0%, p = 0.536).
Conclusion
This meta-analysis demonstrates equivalent rates of functional independence between DD and NDND patients. However, the high proportion of distal occlusions and higher rates of sICH and mortality in NDND patients suggest caution in offering mechanical thrombectomy to DAWN/DEFUSE-3 ineligible patients. A more flexible approach to EVT eligibility criteria could benefit select patients in real-world practice. Nonetheless, further research is needed to identify which patients would benefit from expanded EVT eligibility criteria.





Similar content being viewed by others
References
Jovin TG, Li C, Wu L, Wu C, Chen J, Jiang C et al (2022) Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med 387(15):1373–1384
Tao C, Nogueira RG, Zhu Y, Sun J, Han H, Yuan G et al (2022) Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med 387(15):1361–1372
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372(11):1009–1018
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372(24):2296–2306
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372(11):1019–1030
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372(24):2285–2295
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372(1):11–20
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378(8):708–718
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378(1):11–21
Dittrich TD, Sporns PB, Kriemler LF, Rudin S, Nguyen A, Zietz A et al (2023) Mechanical thrombectomy for large vessel occlusion between 6 and 24 h: outcome comparison of DEFUSE-3/DAWN eligible versus non-eligible patients. Int J Stroke 18(6):697–703
Virtanen P, Tomppo L, Martinez-Majander N, Kokkonen T, Sillanpaa M, Lappalainen K et al (2022) Thrombectomy in acute ischemic stroke in the extended time window: real-life experience in a high-volume center. J Stroke Cerebrovasc Dis 31(8):106603
Siegler JE, Messe SR, Sucharew H, Kasner SE, Mehta T, Arora N et al (2020) Thrombectomy in DAWN- and DEFUSE-3-ineligible patients: a subgroup analysis from the best prospective cohort study. Neurosurgery 86(2):E156–E163
Desai SM, Rocha M, Molyneaux BJ, Starr M, Kenmuir CL, Gross BA et al (2018) Thrombectomy 6–24 hours after stroke in trial ineligible patients. J Neurointerv Surg 10(11):1033–1037
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al (2019) Cochrane handbook for systematic reviews of interventions. Wiley, New York
Herzberg M, Scherling K, Stahl R, Tiedt S, Wollenweber FA, Kupper C et al (2021) Late Thrombectomy in clinical practice : retrospective application of DAWN/DEFUSE3 criteria within the German stroke registry. Clin Neuroradiol 31(3):799–810
Morsi RZ, Elfil M, Ghaith HS, Aladawi M, Elmashad A, Kothari S et al (2023) endovascular thrombectomy for large ischemic strokes: a living systematic review and meta-analysis of randomized trials. J Stroke 25(2):214–222
Ducroux C, Khoury N, Lecler A, Blanc R, Chetrit A, Redjem H et al (2018) Application of the DAWN clinical imaging mismatch and DEFUSE 3 selection criteria: benefit seems similar but restrictive volume cut-offs might omit potential responders. Eur J Neurol 25(8):1093–1099
de Havenon A, Mickolio K, O’Donnell S, Stoddard G, McNally JS, Alexander M et al (2021) Predicting neuroimaging eligibility for extended-window endovascular thrombectomy. J Neurosurg 135(4):1100–1104
Nannoni S, Strambo D, Sirimarco G, Amiguet M, Vanacker P, Eskandari A et al (2020) Eligibility for late endovascular treatment using DAWN, DEFUSE-3, and more liberal selection criteria in a stroke center. J Neurointerv Surg 12(9):842–847
Gao L, Bivard A, Parsons M, Spratt NJ, Levi C, Butcher K et al (2021) Real-world cost-effectiveness of late time window thrombectomy for patients with ischemic stroke. Front Neurol 12:780894
Charbonnier G, Bonnet L, Biondi A, Moulin T (2020) Intracranial bleeding after reperfusion therapy in acute ischemic stroke. Front Neurol 11:629920
Hao Y, Zhang Z, Zhang H, Xu L, Ye Z, Dai Q et al (2017) Risk of intracranial hemorrhage after endovascular treatment for acute ischemic stroke: systematic review and meta-analysis. Interv Neurol 6(1–2):57–64
Ni H, Lu GD, Hang Y, Jia ZY, Cao YZ, Shi HB et al (2023) Association between infarct location and hemorrhagic transformation of acute ischemic stroke following successful recanalization after mechanical thrombectomy. AJNR Am J Neuroradiol 44(1):54–59
Meinel TR, Kniepert JU, Seiffge DJ, Gralla J, Jung S, Auer E et al (2020) Endovascular stroke treatment and risk of intracranial hemorrhage in anticoagulated patients. Stroke 51(3):892–898
Kobeissi H, Ghozy S, Seymour T, Gupta R, Bilgin C, Kadirvel R et al (2023) Outcomes of patients with atrial fibrillation following thrombectomy for stroke: a systematic review and meta-analysis. JAMA Netw Open 6(1):e2249993
Funding
The authors declare that they have no financial interests, funding that could influence the research or its interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
The authors declare that they have no financial interests, funding, or conflicts of interest that could influence the research or its interpretation.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morsi, S., Ghozy, S., Elfil, M. et al. Endovascular thrombectomy for DAWN- and DEFUSE-3 ineligible acute ischemic stroke patients: a systematic review and meta-analysis. J Neurol 271, 2230–2237 (2024). https://doi.org/10.1007/s00415-024-12198-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-024-12198-3