Abstract
Objective
The objective of this study was to investigate the factors influencing relapse and prognosis in patients with primary autoimmune cerebellar ataxia (PACA), an area previously not well understood.
Methods
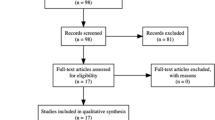
This prospective cohort study included patients who satisfied the modified diagnostic criteria of PACA. A modified Rankin scale score ≤ 2 at the last follow-up was defined as a favorable prognosis. Cox and Logistic regression were utilized to identify relapsing and prognostic factors, respectively.
Results
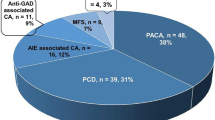
A total of 68 patients were included and 35.3% were male. The median onset age was 42.9 years (IQR 22.1–54.0). Neuronal autoantibodies were detected in 33 (50.8%) patients. Of the 65 patients who received first-line immunotherapy, 55 (84.6%) were responsive and 10 (15.4%) were not. Responsiveness to first-line immunotherapy emerged as an independent factor for favorable prognosis (HR 16.762; 95% CI 2.877–97.655; p = 0.002), as did the absence of peripheral neuropathy/radiculopathy (HR 14.286; 95% CI 2.41–83.333; p = 0.003). Relapses occurred in 19 (27.9%) patients. Onset age ≤ 43 years (HR 5.245; 95% CI 1.499–18.35; p = 0.009), presence of peripheral neuropathy/radiculopathy (HR 4.280; 95% CI 1.622–11.298; p = 0.003) and elevated cerebrospinal fluid (CSF) protein concentration (HR 3.443; 95% CI 1.083–10.951; p = 0.036) were statistically significant relapsing factors.
Conclusion
This study identified younger onset age, presence of peripheral neuropathy/radiculopathy and elevated CSF protein concentration as relapsing factors, and absence of peripheral neuropathy/radiculopathy and responsiveness to first-line immunotherapy as independent factors for favorable prognosis in PACA patients. These findings may guide individualized treatment strategies and potentially improve patient outcomes.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Hadjivassiliou M, Graus F, Honnorat J, Jarius S, Titulaer M, Manto M, Hoggard N, Sarrigiannis P, Mitoma H (2020) Diagnostic criteria for primary autoimmune cerebellar ataxia-guidelines from an international task force on immune-mediated cerebellar ataxias. Cerebellum 19:605–610. https://doi.org/10.1007/s12311-020-01132-8
Muñiz-Castrillo S, Vogrig A, Ciano-Petersen NL, Villagrán-García M, Joubert B, Honnorat J (2022) Novelties in autoimmune and paraneoplastic cerebellar ataxias: twenty years of progresses. The Cerebellum. https://doi.org/10.1007/s12311-021-01363-3
Kudo A, Yaguchi H, Tanaka K, Kimura A, Yabe I (2023) A retrospective study of autoimmune cerebellar ataxia over a 20-year period in a single institution. J Neurol. https://doi.org/10.1007/s00415-023-11946-1
Damato V, Papi C, Spagni G, Evoli A, Silvestri G, Masi G, Sabatelli E, Campetella L, McKeon A, Andreetta F, Riso V, Monte G, Luigetti M, Primiano G, Calabresi P, Iorio R (2021) Clinical features and outcome of patients with autoimmune cerebellar ataxia evaluated with the scale for the assessment and rating of ataxia. Eur J Neurol. https://doi.org/10.1111/ene.15161
Jarius S, Wildemann B (2015) ‘Medusa-head ataxia’: the expanding spectrum of Purkinje cell antibodies in autoimmune cerebellar ataxia. Part 1: Anti-mGluR1, anti-Homer-3, anti-Sj/ITPR1 and anti-CARP VIII. J Neuroinflammation 12:166. https://doi.org/10.1186/s12974-015-0356-y
Jarius S, Wildemann B (2015) ‘Medusa head ataxia’: the expanding spectrum of Purkinje cell antibodies in autoimmune cerebellar ataxia. Part 2: Anti-PKC-gamma, anti-GluR-delta2, anti-Ca/ARHGAP26 and anti-VGCC. J Neuroinflammation 12:167. https://doi.org/10.1186/s12974-015-0357-x
Jarius S, Wildemann B (2015) ‘Medusa head ataxia’: the expanding spectrum of Purkinje cell antibodies in autoimmune cerebellar ataxia. Part 3: Anti-Yo/CDR2, anti-Nb/AP3B2, PCA-2, anti-Tr/DNER, other antibodies, diagnostic pitfalls, summary and outlook. J Neuroinflammation 12:168. https://doi.org/10.1186/s12974-015-0358-9
Hadjivassiliou M, Grunewald RA, Shanmugarajah PD, Sarrigiannis PG, Zis P, Skarlatou V, Hoggard N (2020) Treatment of primary autoimmune cerebellar ataxia with mycophenolate. Cerebellum. https://doi.org/10.1007/s12311-020-01152-4
Jones AL, Flanagan EP, Pittock SJ, Mandrekar JN, Eggers SD, Ahlskog JE, McKeon A (2015) Responses to and outcomes of treatment of autoimmune cerebellar ataxia in adults. JAMA Neurol 72:1304–1312. https://doi.org/10.1001/jamaneurol.2015.2378
Weihua Z, Haitao R, Fang F, Xunzhe Y, Jing W, Hongzhi G (2019) Neurochondrin antibody serum positivity in three cases of autoimmune cerebellar ataxia. Cerebellum 18:1137–1142. https://doi.org/10.1007/s12311-019-01048-y
Liu M, Ren H, Zhu Y, Fan S, Bai L, Wang J, Cui L, Guan H (2022) Autoimmune cerebellar ataxia: etiology and clinical characteristics of a case series from China. Cerebellum. https://doi.org/10.1007/s12311-022-01412-5
Xu X, Lu Q, Huang Y, Fan S, Zhou L, Yuan J, Yang X, Ren H, Sun D, Dai Y, Zhu H, Jiang Y, Zhu Y, Peng B, Cui L, Guan H (2020) Anti-NMDAR encephalitis: a single-center, longitudinal study in China. Neurol Neuroimmunol Neuroinflamm. https://doi.org/10.1212/NXI.0000000000000633
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, Honig LS, Benseler SM, Kawachi I, Martinez-Hernandez E, Aguilar E, Gresa-Arribas N, Ryan-Florance N, Torrents A, Saiz A, Rosenfeld MR, Balice-Gordon R, Graus F, Dalmau J (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165. https://doi.org/10.1016/S1474-4422(12)70310-1
Guo K, Liu X, Lin J, Gong X, Li A, Liu Y, Zhou D, Hong Z (2022) Clinical characteristics, long-term functional outcomes and relapse of anti-LGI1/Caspr2 encephalitis: a prospective cohort study in Western China. Ther Adv Neurol Disord 15:17562864211073204. https://doi.org/10.1177/17562864211073203
Graus F, Dalmau J (2022) Autoimmune Encephalitis and Related Disorders of the Nervous System. In: Graus F, Dalmau J (eds) Autoimmune Encephalitis and Related Disorders of the Nervous System. Cambridge University Press, Cambridge, pp iii–iii
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, Honig LS, Benseler SM, Kawachi I, Martinez-Hernandez E, Aguilar E, Gresa-Arribas N, Ryan-Florance N, Torrents A, Saiz A, Rosenfeld MR, Balice-Gordon R, Graus F, Dalmau J (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165. https://doi.org/10.1016/S1474-4422(12)70310-1
Mehdiyeva A, Hietaharju A, Sipilä J (2022) SEZ6L2 antibody-associated cerebellar ataxia responsive to sequential immunotherapy. Neurol Neuroimmunol Neuroinflamm. https://doi.org/10.1212/NXI.0000000000001131
Thaler FS, Zimmermann L, Kammermeier S, Strippel C, Ringelstein M, Kraft A, Sühs K-W, Wickel J, Geis C, Markewitz R, Urbanek C, Sommer C, Doppler K, Penner L, Lewerenz J, Rößling R, Finke C, Prüss H, Melzer N, Wandinger K-P, Leypoldt F, Kümpfel T (2021) Rituximab treatment and long-term outcome of patients with autoimmune encephalitis: real-world evidence from the GENERATE registry. Neurol Neuroimmunol Neuroinflamm. https://doi.org/10.1212/NXI.0000000000001088
Nosadini M, Eyre M, Molteni E, Thomas T, Irani SR, Dalmau J, Dale RC, Lim M, Anlar B, Armangue T, Benseler S, Cellucci T, Deiva K, Gallentine W, Gombolay G, Gorman MP, Hacohen Y, Jiang Y, Lim BC, Muscal E, Ndondo A, Neuteboom R, Rostásy K, Sakuma H, Sartori S, Sharma S, Tenembaum SN, Van Mater HA, Wells E, Wickstrom R, Yeshokumar AK (2021) Use and safety of immunotherapeutic management of N-methyl-d-aspartate receptor antibody encephalitis: a meta-analysis. JAMA Neurol 78:1333–1344. https://doi.org/10.1001/jamaneurol.2021.3188
Liu M, Xu X, Fan S, Ren H, Zhao Y, Guan H (2023) Mycophenolate mofetil reduces the risk of relapse in anti-leucine-rich glioma-inactivated protein 1 encephalitis: a prospective observational cohort study. Neurol Sci. https://doi.org/10.1007/s10072-023-06968-6
Funding
This study is funded by National High-Level Hospital Clinical Research Funding (2022-PUMCH-B-120).
Author information
Authors and Affiliations
Contributions
LM and GH designed the study. LM, WL and BL recorded the clinical data. LM, BL and FS carried out the data analysis. LM wrote the first draft of the manuscript. RH was responsible for neuronal antibody testing. Important data analysis suggestions were made by RH, FS and GH. Manuscript revisions were made by GH.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, M., Ren, H., Wang, L. et al. Prognostic and relapsing factors of primary autoimmune cerebellar ataxia: a prospective cohort study. J Neurol 271, 1072–1079 (2024). https://doi.org/10.1007/s00415-023-12128-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-12128-9