Abstract
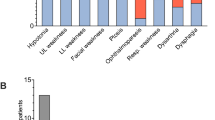
The RASopathies are a group of genetic rare diseases caused by mutations affecting genes involved in the RAS/MAPK (RAS–mitogen activated protein kinase) pathway. Among them, PTPN11 pathogenic variants are responsible for approximately 50% of Noonan syndrome (NS) cases and, albeit to a lesser extent, of Leopard syndrome (LPRD1), which present a few overlapping clinical features, such as facial dysmorphism, developmental delay, cardiac defects, and skeletal deformities. Motor impairment and decreased muscle strength have been recently reported. The etiology of the muscle involvement in these disorders is still not clear but probably multifactorial, considering the role of the RAS/MAPK pathway in skeletal muscle development and Acetylcholine Receptors (AChR) clustering at the neuromuscular junction (NMJ). We report, herein, four unrelated children carrying three different heterozygous mutations in the PTPN11 gene. Intriguingly, their phenotypic features first led to a clinical suspicion of congenital myasthenic syndrome (CMS), due to exercise-induced fatigability with a variable degree of muscle weakness, and serum proteomic profiling compatible with a NMJ defect. Moreover, muscle fatigue improved after treatment with CMS-specific medication. Although the link between PTPN11 gene and neuromuscular transmission is unconfirmed, an increasing number of patients with RASopathies are affected by muscle weakness and fatigability. Hence, NS or LPDR1 should be considered in children with suspected CMS but negative genetic workup for known CMS genes or additional symptoms indicative of NS, such as facial dysmorphism or intellectual disability.


Similar content being viewed by others
Data availability
Genomic and phenotypic data for patients 2, 3 and 4 is available to authorized users of the RD-Connect GPAP in non-identifiable pseudonymized form. Other data is available from the corresponding author upon reasonable request.
References
Tartaglia M, Gelb BD (2005) Noonan syndrome and related disorders: genetics and pathogenesis. Annu Rev Genom Hum Genet 6:45–68
Opitz J, Summitt R, Sarto G (1965) Noonan’s syndrome in girls: a genocopy of the Ullrich-Turner syndrome. J Pediatr 67:968
Noonan J, Ehmke D (1963) Associated noncardiac malformations in children with congenital heart disease. J Pediatr 63:468–470
Mendez HM, Opitz JM (1985) Noonan syndrome: a review. Am J Med Genet 21(3):493-506. https://doi.org/10.1002/ajmg.1320210312
Turner AM (2014) Noonan syndrome. J Paediatr Child Health 50:E14–E20
Burch M, Sharland M, Shinebourne E, et al (1993) Cardiologic abnormalities in noonan syndrome: phenotypic diagnosis and echocardiographic assessment of 118 Patients. J Am Coll Cardiol 22(4):1189-1192. https://doi.org/10.1016/0735-1097(93)90436-5
Linglart L, Gelb BD (2020) Congenital heart defects in Noonan syndrome: diagnosis, management, and treatment. Am J Med Genet C Semin Med Genet 184:73–80. https://doi.org/10.1002/ajmg.c.31765
Romano AA, Allanson JE, Dahlgren J et al (2010) Noonan syndrome: Clinical features, diagnosis, and management guidelines. Pediatrics 126:746–759
Tartaglia M, Gelb BD, Zenker M (2011) Noonan syndrome and clinically related disorders. Best Pract Res Clin Endocrinol Metab 25:161–179
Sarkozy A, Digilio MC, Dallapiccola B (2008) Leopard syndrome. Orphanet J Rare Dis 3:13
Tartaglia M, Mehler EL, Goldberg R et al (2001) Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet 29:465–468. https://doi.org/10.1038/ng772
Kleefstra T, Wortmann SB, Rodenburg RJT et al (2011) Mitochondrial dysfunction and organic aciduria in five patients carrying mutations in the Ras-MAPK pathway. Eur J Hum Genet 19:138–144. https://doi.org/10.1038/ejhg.2010.171
Stevenson DA, Allen S, Tidyman WE et al (2012) Peripheral muscle weakness in RASopathies. Muscle Nerve 46:394–399. https://doi.org/10.1002/mus.23324
de Boode WP, Semmekrot BA, ter Laak HJ et al (1996) Myopathology in patients with a Noonan phenotype. Acta Neuropathol 92:597–602. https://doi.org/10.1007/s004010050566
Keesey J (1989) AAEE Minimonograph #33: electrodiagnostic approach to defects of neuromuscular transmission. Muscle Nerve 12:613–626. https://doi.org/10.1002/mus.880120802
Laurie S, Piscia D, Matalonga L et al (2022) The RD-connect genome-phenome analysis platform: accelerating diagnosis, research, and gene discovery for rare diseases. Hum Mutat. https://doi.org/10.1002/humu.24353
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American college of medical genetics and genomics and the association for molecular pathology. Genet Med 17:405–424. https://doi.org/10.1038/gim.2015.30
Burkhart J, Schumbrutzki C, Wortelkamp S et al (2012) Systematic and quantitative comparison of digest efficiency and specificity reveals the impact of trypsin quality on MS-based proteomics. J Proteom 75:1454–1462
Neel BG, Gu H, Pao L (2003) The ’Shp’ing news: SH2 domain-containing tyrosine phosphatases in cell signaling. Trends Biochem Sci 28:284–293
Tang TL, Freeman RM, O’reilly AM et al (1995) The SH2-containing protein-tyrosine phosphatase SH-PTP2 is required upstream of MAP kinase for early Xenopus development. Cell 80(3):473–483. https://doi.org/10.1016/0092-8674(95)90498-0
Perkins LA, Johnson MR, Melnick MB, Perrimon N (1996) The nonreceptor protein tyrosine phosphatase corkscrew functions in multiple receptor tyrosine kinase pathways in Drosophila. Dev Biol 180(1):63–81. https://doi.org/10.1006/dbio.1996.0285
Arrandale JM, Gore-Willse A, Rocks S et al (1996) Insulin signaling in mice expressing reduced levels of Syp. J Biol Chem 271(35):21353–21358. https://doi.org/10.1074/jbc.271.35.21353
Saxton TM, Henkemeyer M, Tonks S et al (1997) Abnormal mesoderm patterning in mouse embryos mutant for the SH2 tyrosine phosphatase Shp-2. EMBO J 16(9):2352–2364. https://doi.org/10.1093/emboj/16.9.2352
Bertola DR, Pereira AC, Albano LMJ et al (2006) PTPN11 gene analysis in 74 Brazilian patients with Noonan syndrome or Noonan-like phenotype. Genet Test 10:186–191. https://doi.org/10.1089/gte.2006.10.186
Papadopoulou A, Issakidis M, Gole E et al (2012) Phenotypic spectrum of 80 Greek patients referred as Noonan syndrome and PTPN11 mutation analysis: the value of initial clinical assessment. Eur J Pediatr 171:51–58
Martinelli S, Nardozza AP, Vigne SD et al (2012) Counteracting effects operating on Src homology 2 domain-containing protein-tyrosine phosphatase 2 (SHP2) function drive selection of the recurrent Y62D and Y63C substitutions in Noonan syndrome. J Biol Chem 287:27066–27077. https://doi.org/10.1074/jbc.M112.350231
Estephan EP, Zambon AA, Thompson R et al (2022) Congenital myasthenic syndrome: correlation between clinical features and molecular diagnosis. Eur J Neurol 29:833–842. https://doi.org/10.1111/ene.15173
Tartaglia M, Kalidas K, Shaw A et al (2002) PTPN11 mutations in noonan syndrome: molecular spectrum, genotype-phenotype correlation, and phenotypic heterogeneity. Am J Hum Genet 70(6):1555-1563. https://doi.org/10.1086/340847
Musante L, Kehl HG, Majewski F et al (2003) Spectrum of mutations in PTPN11 and genotype - phenotype correlation in 96 patients with Noonan syndrome and five patients with cardio-facio-cutaneous syndrome. Eur J Hum Genet 11:201–206. https://doi.org/10.1038/sj.ejhg.5200935
Digilio MC, Conti E, Sarkozy A et al (2002) Grouping of multiple-lentigines/LEOPARD and Noonan syndromes on the PTPN11 gene. Am J Hum Genet 71(2):389–394. https://doi.org/10.1086/341528
Athota JP, Bhat M, Nampoothiri S et al (2020) Molecular and clinical studies in 107 Noonan syndrome affected individuals with PTPN11 mutations. BMC Med Genet. https://doi.org/10.1186/s12881-020-0986-5
Spatola M, Wider C, Kuntzer T, Croquelois A (2015) PTPN11 mutation manifesting as LEOPARD syndrome associated with hypertrophic plexi and neuropathic pain. BMC Neurol 15:55. https://doi.org/10.1186/s12883-015-0310-8
Lin I-S, Wang J-N, Chao S-C et al (2009) PTPN11 mutations in LEOPARD syndrome: report of four cases in Taiwan. J Formos Med Assoc 108:803–807. https://doi.org/10.1016/S0929-6646(09)60408-3
Writzl K, Hoovers J, Sistermans EA, Hennekam RCM (2007) LEOPARD syndrome with partly normal skin and sex chromosome mosaicism. Am J Med Genet A 143A:2612–2615. https://doi.org/10.1002/ajmg.a.31991
Keren B, Hadchouel A, Saba S et al (2004) PTPN11 mutations in patients with LEOPARD syndrome: a French multicentric experience. J Med Genet 41:e117–e117. https://doi.org/10.1136/jmg.2004.021451
Hanna N, Montagner A, Lee WH et al (2006) Reduced phosphatase activity of SHP-2 in LEOPARD syndrome: consequences for PI3K binding on Gab1. FEBS Lett 580:2477–2482. https://doi.org/10.1016/j.febslet.2006.03.088
Martinelli S, Torreri P, Tinti M et al (2008) Diverse driving forces underlie the invariant occurrence of the T42A, E139D, I282V and T468M SHP2 amino acid substitutions causing Noonan and LEOPARD syndromes. Hum Mol Genet 17:2018–2029. https://doi.org/10.1093/hmg/ddn099
Oishi K, Zhang H, Gault WJ et al (2009) Phosphatase-defective LEOPARD syndrome mutations in PTPN11 gene have gain-of-function effects during Drosophila development. Hum Mol Genet 18:193–201. https://doi.org/10.1093/hmg/ddn336
Yu Z-H, Zhang R-Y, Walls CD et al (2014) Molecular basis of gain-of-function LEOPARD syndrome-associated SHP2 mutations. Biochemistry 53:4136–4151. https://doi.org/10.1021/bi5002695
Stevenson DA, Yang FC (2011) The musculoskeletal phenotype of the RASopathies. Am J Med Genet C Semin Med Genet 157:90–103. https://doi.org/10.1002/ajmg.c.30296
Kossler N, Stricker S, Rödelsperger C et al (2011) Neurofibromin (Nf1) is required for skeletal muscle development. Hum Mol Genet 20:2697–2709. https://doi.org/10.1093/hmg/ddr149
Stassou S, Nadroo A, Schubert R et al (2005) A new syndrome of myopathy with muscle spindle excess. J Perinat Med 33:179–182
Tidyman WE, Lee HS, Rauen KA (2011) Skeletal muscle pathology in Costello and cardio-facio-cutaneous syndromes: developmental consequences of germline Ras/MAPK activation on myogenesis. Am J Med Genet C Semin Med Genet 157:104–114. https://doi.org/10.1002/ajmg.c.30298
Sinico M, Bassez G, Touboul C et al (2011) Excess of neuromuscular spindles in a fetus with Costello syndrome: a clinicopathological report. Pediatr Dev Pathol 14:218–223. https://doi.org/10.2350/09-06-0664-CR.1
Lee I, Pecinova A, Pecina P et al (2010) A suggested role for mitochondria in Noonan syndrome. Biochim Biophys Acta Mol Basis Dis 1802:275–283. https://doi.org/10.1016/j.bbadis.2009.10.005
Santoro C, Pacileo G, Limongelli G et al (2014) LEOPARD syndrome: clinical dilemmas in differential diagnosis of RASopathies. BMC Med Genet 15:44. https://doi.org/10.1186/1471-2350-15-44
Qian YK, Chan AW, Madhavan R, Peng HB (2008) The function of Shp2 tyrosine phosphatase in the dispersal of acetylcholine receptor clusters. BMC Neurosci 9:70. https://doi.org/10.1186/1471-2202-9-70
Huda S, Cao M, De Rosa A et al (2020) SHP2 inhibitor protects AChRs from effects of myasthenia gravis MuSK antibody. Neurol Neuroimmunol Neuroinflamm 7:e645. https://doi.org/10.1212/NXI.0000000000000645
McMacken G, Cox D, Roos A et al (2018) The beta-adrenergic agonist salbutamol modulates neuromuscular junction formation in zebrafish models of human myasthenic syndromes. Hum Mol Genet 27:1556–1564. https://doi.org/10.1093/hmg/ddy062
Roos A, Thompson R, Horvath R et al (2018) Intersection of proteomics and genomics to “solve the unsolved” in Rare disorders such as neurodegenerative and neuromuscular diseases. Proteom Clin Appl 12:1700073. https://doi.org/10.1002/prca.201700073
Kollipara L, Buchkremer S, Coraspe JAG et al (2017) In-depth phenotyping of lymphoblastoid cells suggests selective cellular vulnerability in Marinesco-Sjögren syndrome. Oncotarget 8:68493–68516. https://doi.org/10.18632/oncotarget.19663
Gangfuß A, Hentschel A, Rademacher N et al (2022) Identification of a novel homozygous synthesis of cytochrome c oxidase 2 variant in siblings with early-onset axonal Charcot-Marie-Tooth disease. Hum Mutat 43:477–486. https://doi.org/10.1002/humu.24338
Van Horn MR, Strasser A, Miraucourt LS et al (2017) The gliotransmitter d-serine promotes synapse maturation and axonal stabilization in vivo. J Neurosci 37:6277–6288. https://doi.org/10.1523/JNEUROSCI.3158-16.2017
Hathazi D, Cox D, D’Amico A et al (2021) INPP5K and SIL1 associated pathologies with overlapping clinical phenotypes converge through dysregulation of PHGDH. Brain 144:2427–2442. https://doi.org/10.1093/brain/awab133
Dulewicz M, Kulczyńska-Przybik A, Słowik A et al (2021) Neurogranin and neuronal pentraxin receptor as synaptic dysfunction biomarkers in Alzheimer’s disease. J Clin Med 10:4575. https://doi.org/10.3390/jcm10194575
Askanas V, Engel WK, Alvarez RB et al (2000) Novel Immunolocalization of α-synuclein in human muscle of inclusion-body myositis, regenerating and necrotic muscle fibers, and at neuromuscular junctions. J Neuropathol Exp Neurol 59:592–598. https://doi.org/10.1093/jnen/59.7.592
Stam M, Wijngaarde CA, Bartels B et al (2022) Randomized double-blind placebo-controlled crossover trial with pyridostigmine in spinal muscular atrophy types 2–4. Brain Commun. https://doi.org/10.1093/braincomms/fcac324
Graf ER, Heerssen HM, Wright CM et al (2011) Stathmin is required for stability of the drosophila neuromuscular junction. J Neurosci 31:15026–15034. https://doi.org/10.1523/JNEUROSCI.2024-11.2011
Villalón E, Kline RA, Smith CE et al (2019) AAV9-Stathmin1 gene delivery improves disease phenotype in an intermediate mouse model of spinal muscular atrophy. Hum Mol Genet 28:3742–3754. https://doi.org/10.1093/hmg/ddz188
Acknowledgements
HL receives support from the Canadian Institutes of Health Research (Foundation Grant FDN-167281), the Canadian Institutes of Health Research and Muscular Dystrophy Canada (Network Catalyst Grant for NMD4C), the Canada Foundation for Innovation (CFI-JELF 38412), and the Canada Research Chairs program (Canada Research Chair in Neuromuscular Genomics and Health, 950-232279). RT and KP are recipients of CIHR Postdoctoral fellowships. This research was also partly funded by the European Regional Development Fund (ERDF; project NME-GPS; grant to AR and USS) as well as the German Society for Muscular Diseases (DGM; grant to AR and USS). Moreover, the study was supported by the “Ministerium für Kultur und Wissenschaft des Landes Nordrhein-Westfalen,” the “Regierenden Bürgermeister von Berlin—Senatskanzlei Wissenschaft und Forschung,” and the “Bundesministerium für Bildung und Forschung”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval statement
All patients provided their informed consent for the original genetic analysis that is now retrospectively summarized in this paper, and informed consent was obtained for the publication of patient images. Patient 1 was diagnosed within a standard clinical diagnostics process for which research ethics approval was not required. The RD-Connect GPAP, which was used for analysis of patients 2, 3 and 4, has received ethics approval from the Parc de Salut MAR Clinical Research Ethics Committee on 27 October 2015 under ref. no. 2015/6456/I.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pugliese, A., Della Marina, A., de Paula Estephan, E. et al. Mutations in PTPN11 could lead to a congenital myasthenic syndrome phenotype: a Noonan syndrome case series. J Neurol 271, 1331–1341 (2024). https://doi.org/10.1007/s00415-023-12070-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-12070-w