Abstract
Background
The aim of this Delphi study was to reach consensus about definition, operationalization and assessment of visual pursuit (VP) and visual fixation (VF).
Methods
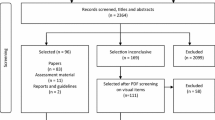
In a three-round international Delphi study, clinical and research experts on disorders of consciousness indicated their level of agreement on 87 statements using a 5-point Likert scale. Consensus for agreement was defined by a median of 5, an interquartile range (IQR) ≤ 1, and ≥ 80% indicating moderate or strong agreement.
Results
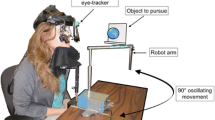
Forty-three experts from three continents participated, 32 completed all three rounds. For VP, the consensus statements with the highest levels of agreement were on the term ‘pursuit of a visual stimulus’, the description ‘ability to follow visually in horizontal and/or vertical plane’, a duration > 2 s, tracking in horizontal and vertical planes, and a frequency of more than 2 times per assessment. For VF, consensus statements with the highest levels of agreement were on the term ‘sustained VF’, the description ‘sustained fixation in response to a salient stimulus’, a duration of > 2 s and a frequency of 2 or more times per assessment. The assessment factors with the highest levels of agreement were personalized stimuli, the use of eye tracking technology, a patient dependent time of assessment, sufficient environmental light, upright posture, and the necessity to exclude ocular/oculomotor problems.
Conclusion
This first international Delphi study on VP and VF in patients with disorders of consciousness provides provisional operational definitions and an overview of the most relevant assessment factors.


Similar content being viewed by others
Data availability
Anonymized data will be shared upon reasonable request.
References
Laureys S, Celesia G, Cohadon F, Lavrijsen J, León-Carrión J, Sannita W, Sazbon L, Schmutzhard E, von Wild K, Zeman A, Dolce G (2010) Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med 8:68. https://doi.org/10.1186/1741-7015-8-68
Giacino JT, Ashwal S, Childs N, Cranford R, Jennett B, Katz DI, Kelly JP, Rosenberg JH, Whyte J, Zafonte RD, Zasler ND (2002) The minimally conscious state: definition and diagnostic criteria. Neurology 58:349–353. https://doi.org/10.1212/wnl.58.3.349
Multi-Society Task Force on PVS (1994) Medical aspects of the persistent vegetative state (1). N Engl J Med 330:1499–1508. https://doi.org/10.1056/NEJM199405263302107
Giacino JT, Kalmar K, Whyte J (2004) The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil 85:2020–2029. https://doi.org/10.1016/j.apmr.2004.02.033
Schnakers C, Vanhaudenhuyse A, Giacino J, Ventura M, Boly M, Majerus S, Moonen G, Laureys S (2009) Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol 9:35. https://doi.org/10.1186/1471-2377-9-35
van Erp WS, Lavrijsen JC, Vos PE, Bor H, Laureys S, Koopmans RT (2015) The vegetative state: prevalence, misdiagnosis, and treatment limitations. J Am Med Dir Assoc 16:85 e89-85 e14. https://doi.org/10.1016/j.jamda.2014.10.014
Luaute J, Maucort-Boulch D, Tell L, Quelard F, Sarraf T, Iwaz J, Boisson D, Fischer C (2010) Long-term outcomes of chronic minimally conscious and vegetative states. Neurology 75:246–252. https://doi.org/10.1212/WNL.0b013e3181e8e8df
Boly M, Faymonville ME, Schnakers C, Peigneux P, Lambermont B, Phillips C, Lancellotti P, Luxen A, Lamy M, Moonen G, Maquet P, Laureys S (2008) Perception of pain in the minimally conscious state with PET activation: an observational study. Lancet Neurol 7:1013–1020. https://doi.org/10.1016/S1474-4422(08)70219-9
Eilander HJ, Wijnen VJ, Scheirs JG, de Kort PL, Prevo AJ (2005) Children and young adults in a prolonged unconscious state due to severe brain injury: outcome after an early intensive neurorehabilitation programme. Brain Inj 19:425–436. https://doi.org/10.1080/02699050400025299
Seel RT, Douglas J, Dennison AC, Heaner S, Farris K, Rogers C (2013) Specialized early treatment for persons with disorders of consciousness: program components and outcomes. Arch Phys Med Rehabil 94:1908–1923. https://doi.org/10.1016/j.apmr.2012.11.052
Giacino JT, Whyte J, Bagiella E, Kalmar K, Childs N, Khademi A, Eifert B, Long D, Katz DI, Cho S, Yablon SA, Luther M, Hammond FM, Nordenbo A, Novak P, Mercer W, Maurer-Karattup P, Sherer M (2012) Placebo-controlled trial of amantadine for severe traumatic brain injury. N Engl J Med 366:819–826. https://doi.org/10.1056/NEJMoa1102609
Singh R, McDonald C, Dawson K, Lewis S, Pringle AM, Smith S, Pentland B (2008) Zolpidem in a minimally conscious state. Brain Inj 22:103–106. https://doi.org/10.1080/02699050701829704
Thibaut A, Bruno MA, Ledoux D, Demertzi A, Laureys S (2014) tDCS in patients with disorders of consciousness: sham-controlled randomized double-blind study. Neurology 82:1112–1118. https://doi.org/10.1212/WNL.0000000000000260
Schiff ND, Giacino JT, Kalmar K, Victor JD, Baker K, Gerber M, Fritz B, Eisenberg B, Biondi T, O’Connor J, Kobylarz EJ, Farris S, Machado A, McCagg C, Plum F, Fins JJ, Rezai AR (2007) Behavioural improvements with thalamic stimulation after severe traumatic brain injury. Nature 448:600–603. https://doi.org/10.1038/nature06041
Wilkinson D, Savulescu J (2013) Is it better to be minimally conscious than vegetative? J Med Ethics 39:557–558. https://doi.org/10.1136/medethics-2012-100954
Cranford RE (1998) The vegetative and minimally conscious states: ethical implications. Geriatrics 53(Suppl 1):S70-73
Fins JJ, Bernat JL (2018) Ethical, palliative, and policy considerations in disorders of consciousness. Neurology 91:471–475. https://doi.org/10.1212/WNL.0000000000005927
Giacino JT, Kalmar K (2005) Diagnostic and prognostic guidelines for the vegetative and minimally conscious states. Neuropsychol Rehabil 15:166–174. https://doi.org/10.1080/09602010443000498
Giacino JT, Kalmar K (1997) The vegetative and minimally conscious states: a comparison of clinical features and functional outcome. J Head Trauma Rehabil 12:36–51. https://doi.org/10.1097/00001199-199708000-00005
Shiel A, Horn SA, Wilson BA, Watson MJ, Campbell MJ, McLellan DL (2000) The Wessex Head Injury Matrix (WHIM) main scale: a preliminary report on a scale to assess and monitor patient recovery after severe head injury. Clin Rehabil 14:408–416. https://doi.org/10.1191/0269215500cr326oa
Ansell BJ, Keenan JE (1989) The Western Neuro Sensory Stimulation Profile: a tool for assessing slow-to-recover head-injured patients. Arch Phys Med Rehabil 70:104–108
Noe E, Olaya J, Navarro MD, Noguera P, Colomer C, Garcia-Panach J, Rivero S, Moliner B, Ferri J (2012) Behavioral recovery in disorders of consciousness: a prospective study with the Spanish version of the Coma Recovery Scale-Revised. Arch Phys Med Rehabil 93(428–433):e412. https://doi.org/10.1016/j.apmr.2011.08.048
Estraneo A, Moretta P, Cardinale V, De Tanti A, Gatta G, Giacino JT, Trojano L (2015) A multicentre study of intentional behavioural responses measured using the Coma Recovery Scale-Revised in patients with minimally conscious state. Clin Rehabil 29:803–808. https://doi.org/10.1177/0269215514556002
Wannez S, Gosseries O, Azzolini D, Martial C, Cassol H, Aubinet C, Annen J, Martens G, Bodart O, Heine L, Charland-Verville V, Thibaut A, Chatelle C, Vanhaudenhuyse A, Demertzi A, Schnakers C, Donneau AF, Laureys S (2018) Prevalence of coma-recovery scale-revised signs of consciousness in patients in minimally conscious state. Neuropsychol Rehabil 28:1350–1359. https://doi.org/10.1080/09602011.2017.1310656
Bagnato S, Boccagni C, Sant’Angelo A, Fingelkurts AA, Fingelkurts AA, Galardi G (2017) Longitudinal assessment of clinical signs of recovery in patients with unresponsive wakefulness syndrome after traumatic or nontraumatic brain injury. J Neurotrauma 34:535–539. https://doi.org/10.1089/neu.2016.4418
Martens G, Bodien Y, Sheau K, Christoforou A, Giacino JT (2020) Which behaviours are first to emerge during recovery of consciousness after severe brain injury? Ann Phys Rehabil Med 63:263–269. https://doi.org/10.1016/j.rehab.2019.10.004
American Congress of Rehabilitation Medicine BI-ISIGDoCTF, Seel RT, Sherer M, Whyte J, Katz DI, Giacino JT, Rosenbaum AM, Hammond FM, Kalmar K, Pape TL, Zafonte R, Biester RC, Kaelin D, Kean J, Zasler N (2010) Assessment scales for disorders of consciousness: evidence-based recommendations for clinical practice and research. Arch Phys Med Rehabil 91:1795–1813. https://doi.org/10.1016/j.apmr.2010.07.218
Kondziella D, Bender A, Diserens K, van Erp W, Estraneo A, Formisano R, Laureys S, Naccache L, Ozturk S, Rohaut B, Sitt JD, Stender J, Tiainen M, Rossetti AO, Gosseries O, Chatelle C, Ean Panel on Coma DoC (2020) European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur J Neurol 27:741–756. https://doi.org/10.1111/ene.14151
Giacino JT, Katz DI, Schiff ND, Whyte J, Ashman EJ, Ashwal S, Barbano R, Hammond FM, Laureys S, Ling GSF, Nakase-Richardson R, Seel RT, Yablon S, Getchius TSD, Gronseth GS, Armstrong MJ (2018) Practice guideline update recommendations summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 91:450–460. https://doi.org/10.1212/WNL.0000000000005926
Overbeek BUH, Eilander HJ, Lavrijsen JCM, Koopmans R (2018) Are visual functions diagnostic signs of the minimally conscious state? an integrative review. J Neurol 265:1957–1975. https://doi.org/10.1007/s00415-018-8788-9
Keeney S, Hasson F, McKenna HP (2011) The Delphi technique in nursing and health research. Wiley-Blackwell, Oxford
Junger S, Payne SA, Brine J, Radbruch L, Brearley SG (2017) Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 31:684–706. https://doi.org/10.1177/0269216317690685
Giacino JT, Whyte J, Nakase-Richardson R, Katz DI, Arciniegas DB, Blum S, Day K, Greenwald BD, Hammond FM, Pape TB, Rosenbaum A, Seel RT, Weintraub A, Yablon S, Zafonte RD, Zasler N (2020) Minimum competency recommendations for programs that provide rehabilitation services for persons with disorders of consciousness: a position statement of the american congress of rehabilitation medicine and the national institute on disability, independent living and rehabilitation research traumatic brain injury model systems. Arch Phys Med Rehabil 101:1072–1089. https://doi.org/10.1016/j.apmr.2020.01.013
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67:401–409. https://doi.org/10.1016/j.jclinepi.2013.12.002
Koopmans RT, Lavrijsen JC, Hoek F (2013) Concrete steps toward academic medicine in long term care. J Am Med Dir Assoc 14:781–783. https://doi.org/10.1016/j.jamda.2013.08.004
Leigh RJ, Zee DS (2015) The neurology of eye movements. Oxford University Press, New York
Giacino JT (1997) Disorders of consciousness: differential diagnosis and neuropathologic features. Semin Neurol 17:105–111. https://doi.org/10.1055/s-2008-1040919
Magliacano A, De Bellis F, Galvao-Carmona A, Estraneo A, Trojano L (2019) Can salient stimuli enhance responses in disorders of consciousness? A systematic review. Curr Neurol Neurosci Rep 19:98. https://doi.org/10.1007/s11910-019-1018-8
Blume C, Lechinger J, Santhi N, del Giudice R, Gnjezda MT, Pichler G, Scarpatetti M, Donis J, Michitsch G, Schabus M (2017) Significance of circadian rhythms in severely brain-injured patients: a clue to consciousness? Neurology 88:1933–1941. https://doi.org/10.1212/WNL.0000000000003942
Wilson BA, Dhamapurkar S, Tunnard C, Watson P, Florschutz G (2013) The effect of positioning on the level of arousal and awareness in patients in the vegetative state or the minimally conscious state: a replication and extension of a previous finding. Brain Impairment 14:475–479. https://doi.org/10.1017/BrImp.2013.34
Chatelle C, Bodien YG, Carlowicz C, Wannez S, Charland-Verville V, Gosseries O, Laureys S, Seel RT, Giacino JT (2016) Detection and interpretation of impossible and improbable coma recovery scale-revised scores. Arch Phys Med Rehabil 97(1295–1300):e1294. https://doi.org/10.1016/j.apmr.2016.02.009
Trojano L, Moretta P, Masotta O, Loreto V, Estraneo A (2018) Visual pursuit of one’s own face in disorders of consciousness: a quantitative analysis. Brain Inj 32:1549–1555. https://doi.org/10.1080/02699052.2018.1504117
Ting WK, Perez Velazquez JL, Cusimano MD (2014) Eye movement measurement in diagnostic assessment of disorders of consciousness. Front Neurol 5:137. https://doi.org/10.3389/fneur.2014.00137
Spering M, Carrasco M (2015) Acting without seeing: eye movements reveal visual processing without awareness. Trends Neurosci 38:247–258. https://doi.org/10.1016/j.tins.2015.02.002
Schnakers C (2020) Update on diagnosis in disorders of consciousness. Expert Rev Neurother 20:997–1004. https://doi.org/10.1080/14737175.2020.1796641
Royal College of Physicians (2020) Prolonged disorders of consciousness following sudden onset brain injury: National clinical guidelines. RCP, London
Giacino JT, Kalmar K (2004) Coma Recovery Scale-Revised. Administration and Scoring Guidelines. In: Injuries CfH (ed), Edison, New Jersey. http://www.tbims.org/combi/crs/CRS%20Syllabus.pdf
Fitzpatrick-DeSalme E, Long A, Patel F, Whyte J (2021) Behavioral assessment of patients with disorders of consciousness. J Clin Neurophysiol. https://doi.org/10.1097/WNP.0000000000000666
Acknowledgements
We thank all the experts for participating in this study. We thank the IBIA special interest group on diagnosis/prognosis of DoC for their help in recuitment of experts and discussing the study. We thank ‘Stichting St. Joannes de Deo’ and ‘Het Coma-Hospitium’ for funding this study. We thank Anita Oude Bos, research assistant of the Radboud University Medical Center for developing and processing the online survey and calculating the results. We thank Camille Chatelle PhD and Theresa Bender-Pape PhD for reviewing the survey.
Funding
This study was funded by ‘Het Coma-Hospitium’ and ‘Stichting St. Joannes de Deo’.
Author information
Authors and Affiliations
Contributions
BO contributed to the design of the study protocol, acquisition and analysis of the data and drafted the manuscript. JL contributed to the design of the study protocol, analysis of the data and drafted a significant proportion of the manuscript. SvG contributed to the review of the study protocol, interpretatation of the data and revision of the manuscript. DK contributed to the review of the study protocol, interpretatation of the data and revision of the manuscript. HE contributed to the design of the study protocol, analysis of the data and drafted a significant proportion of the manuscript. RK contributed to the design of the study protocol, analysis of the data and drafted a significant proportion of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendsments or comparable ethical standards.
Informed consent
Informed consent was obtained from the participating experts prior to the start of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Overbeek, B.U.H., Lavrijsen, J.C.M., van Gaal, S. et al. Towards consensus on visual pursuit and visual fixation in patients with disorders of consciousness. A Delphi study. J Neurol 269, 3204–3215 (2022). https://doi.org/10.1007/s00415-021-10905-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10905-y