Abstract
Background
This study addresses the challenging characterisation and differentiation of CIDP versus CIDP in association with Sjögren’s syndrome to facilitate the process in clinical routine.
Methods
Patients with both CIDP and Sjögren’s syndrome and CIDP without Sjögren’s syndrome were compared concerning relevant differences in clinical, laboratory and electrophysiological findings. 154 patients who fulfilled the diagnostic EFNS/PNS criteria for CIDP were included in the analysis. 54 of these patients additionally fulfilled the ACR/EULAR classification criteria for Sjögren’s syndrome.
Results
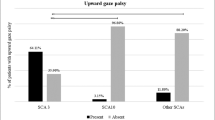
The frequency of female patients was higher in patients with CIDP and Sjögren’s syndrome (52%) versus CIDP patients without Sjögren’s syndrome (28%). Furthermore, the occurrence of cranial nerve impairment was significantly higher in patients with Sjögren’s syndrome (39% versus 14%). There were no significant group differences in the evaluation of initial symptoms, severity of disability judged by INCAT disability scale score, presence or distribution of sensory deficits, limb weakness and the presence of ataxia, pain or dysautonomia, CSF laboratory or electrophysiological findings.
Conclusions
In conclusion, our data indicate that cranial nerve impairment and female gender might represent red flags for an additional Sjögren’s syndrome in patients with CIDP. The patterns of clinical disabilities and electrophysiological findings due to peripheral nerve damage are similar in both CIDP entities.
Similar content being viewed by others
Data availability
Data are available upon reasonable request.
References
Sjögren H (1933) Zur kenntnis der keratoconjunctivitis sicca. Acta Ophthalmol 13:1–39
Seror R, Ravaud P, Bowman SJ et al (2010) EULAR Sjögren’s syndrome disease activity index: development of a consensus systemic disease activity index for primary Sjögren’s syndrome. Ann Rheum Dis 69:1103–1109. https://doi.org/10.1136/ard.2009.110619
Ramos-Casals M, Brito-Zerón P, Seror R et al (2015) Characterization of systemic disease in primary Sjögren’s syndrome: EULAR-SS Task Force recommendations for articular, cutaneous, pulmonary and renal involvements. Rheumatol (Oxf) 54:2230–2238. https://doi.org/10.1093/rheumatology/kev200
Jaskólska M, Chylińska M, Masiak A et al (2020) Neuro-Sjögren: uncommon or underestimated problem? Brain Behav. https://doi.org/10.1002/BRB3.1665
Thiele T, Seeliger T, Witte T et al (2020) Severe polyneuropathy in primary Sjögren’s syndrome: Sjögren’s syndrome should be considered in patients with motor neuropathy. Z Rheumatol 79:707–709
Seeliger T, Prenzler NK, Gingele S et al (2019) Neuro-Sjögren: peripheral neuropathy with limb weakness in Sjögren’s Syndrome. Front Immunol 10:1600. https://doi.org/10.3389/fimmu.2019.01600
Perzyńska-Mazan J, Maślińska M, Gasik R (2020) Neurophysiological features of peripheral nervous system involvement and immunological profile of patients with primary Sjögren Syndrome. J Rheumatol. https://doi.org/10.3899/jrheum.181464 (jrheum.181464)
Delalande S, de Seze J, Fauchais A-L et al (2004) Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Med (Baltim) 83:280–291
Teixeira F, Moreira I, Silva AM et al (2013) Neurological involvement in primary Sjögren syndrome. Acta Reumatol Port 38:29–36
Van den Bergh PYK, Hadden RDM, Bouche P et al (2010) European federation of neurological societies/peripheral nerve society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European federation of neurological societies and the peripheral nerve society: first revision. Eur J Neurol 17:356–363. https://doi.org/10.1111/j.1468-1331.2009.02930.x
Shiboski CH, Shiboski SC, Seror R et al (2017) 2016 American college of rheumatology/European league against rheumatism classification criteria for primary Sjögren’s syndrome. Ann Rheum Dis 76:9–16. https://doi.org/10.1136/annrheumdis-2016-210571
Hughes R, Bensa S, Willison H et al (2001) Randomized controlled trial of intravenous immunoglobulin versus oral prednisolone in chronic inflammatory demyelinating polyradiculoneuropathy. Ann Neurol 50:195–201
Stålberg E, Falck B, Gilai A et al (1999) Standards for quantification of EMG and neurography. The international federation of clinical neurophysiology. Electroencephalogr Clin Neurophysiol Suppl 52:213–220
Schwenkenbecher P, Chacko LP, Wurster U et al (2016) Intrathecal synthesis of anti-Hu antibodies distinguishes patients with paraneoplastic peripheral neuropathy and encephalitis. BMC Neurol 16:136. https://doi.org/10.1186/s12883-016-0657-5
Seror R, Theander E, Brun JG et al (2015) Validation of EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient indexes (ESSPRI). Ann Rheum Dis 74:859–866. https://doi.org/10.1136/annrheumdis-2013-204615
Seeliger T, Bönig L, Witte T et al (2020) Hearing dysfunction in patients with Neuro-Sjögren: a cross-sectional study. Ann Transl Med 8:1069–1069. https://doi.org/10.21037/atm-20-1856
Mori K, Iijima M, Koike H et al (2005) The wide spectrum of clinical manifestations in Sjögren’s syndrome-associated neuropathy. Brain 128:2518–2534. https://doi.org/10.1093/brain/awh605
Carvajal Alegria G, Guellec D, Mariette X et al (2016) Epidemiology of neurological manifestations in Sjögren’s syndrome: data from the French ASSESS Cohort. RMD open 2:e000179. https://doi.org/10.1136/rmdopen-2015-000179
Phuljhele S, Pujari A, Obedulla H et al (2019) Atypical presentation of primary Sjögren’s syndrome as optic neuritis. Can J Ophthalmol 54:e30–e32
Pars K, Pul R, Schwenkenbecher P et al (2017) Cerebrospinal fluid findings in neurological diseases associated with Sjögren’s syndrome. Eur Neurol 77:91–102. https://doi.org/10.1159/000454765
Hughes RAC, Bouche P, Cornblath DR et al (2006) European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European federation of neurological societies and the peripher. Eur J Neurol 13:326–332. https://doi.org/10.1111/j.1468-1331.2006.01278.x
Beeson PB (1994) Age and sex associations of 40 autoimmune diseases. Am J Med 96:457–462
Alamanos Y, Tsifetaki N, Voulgari PV et al (2006) Epidemiology of primary Sjögren’s syndrome in north-west Greece, 1982–2003. Rheumatology 45:187–191. https://doi.org/10.1093/rheumatology/kei107
Izmirly PM, Buyon JP, Wan I et al (2018) The incidence and prevalence of adult primary Sjögren’s syndrome in New York county. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.23707
Lunn MP, Manji H, Choudhary PP et al (1999) Chronic inflammatory demyelinating polyradiculoneuropathy: a prevalence study in south east England. J Neurol Neurosurg Psychiatry 66:677–680
Chio A, Cocito D, Bottacchi E et al (2007) Idiopathic chronic inflammatory demyelinating polyneuropathy: an epidemiological study in Italy. J Neurol Neurosurg Psychiatry 78:1349–1353. https://doi.org/10.1136/jnnp.2007.114868
Laughlin RS, Dyck PJ, Melton LJ et al (2009) Incidence and prevalence of CIDP and the association of diabetes mellitus. Neurology 73:39–45. https://doi.org/10.1212/WNL.0b013e3181aaea47
Sivadasan A, Muthusamy K, Patel B et al (2017) Clinical spectrum, therapeutic outcomes, and prognostic predictors in Sjogren’s syndrome-associated neuropathy. Ann Indian Acad Neurol 20:278–283. https://doi.org/10.4103/aian.AIAN_116_17
Rajabally YA, Attarian S, Delmont E (2020) Evolving immunologic perspectives in chronic inflammatory demyelinating polyneuropathy. J Inflamm Res 13:543–549
Author information
Authors and Affiliations
Contributions
Substantial contributions were made by TSk, TW, MS, DE, TT, NP and SK to conception and design of the work, by FK, LB, SG, NP and TSe to data acquisition, by TSe, SG, TT, DE and LB to data analysis and by TSe, TSk, TW, MS, SK to data interpretation.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest or competing interests regarding the publication of this paper.
Ethics approval
The local Ethics Committee of the Hannover Medical School approved of this study 8172_BO_K_2018. The study was undertaken according to the Declaration of Helsinki.
Consent to participate
All patients gave their informed consent to participate.
Consent for publication
All patients gave their informed consent for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
415_2021_10459_MOESM1_ESM.tif
Supplementary file1 (TIF 725 KB) Supplementary Figure 1 Initial symptoms reported by CIDP patients with (A) and without Sjögren’s syndrome (B).
415_2021_10459_MOESM2_ESM.xlsx
Supplementary file2 (XLSX 14 KB) Supplementary Table 1 Nerve conduction studies in absolute values and significance levels for CIDP patients with and without Sjögren’s syndrome.
415_2021_10459_MOESM3_ESM.xlsx
Supplementary file3 (XLSX 11 KB) Supplementary Table 2 Cerebrospinal fluid (CSF) analysis compared in patients with and without Sjögren’s syndrome.
Rights and permissions
About this article
Cite this article
Seeliger, T., Gingele, S., Bönig, L. et al. CIDP associated with Sjögren’s syndrome. J Neurol 268, 2908–2912 (2021). https://doi.org/10.1007/s00415-021-10459-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10459-z