Abstract
Objective
Lumbar punctures (LPs) are important for obtaining CSF in neurology studies but are associated with adverse events and feared by many patients. We determined adverse event rates and pain scores in patients prospectively enrolled in two cohort studies who underwent LPs using a standardized protocol and 25 g needle.
Methods
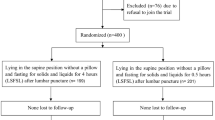
Eight hundred and nine LPs performed in 262 patients age ≥ 60 years in the MADCO-PC and INTUIT studies were analyzed. Medical records were monitored for LP-related adverse events, and patients were queried about subjective complaints. We analyzed adverse event rates, including headaches and pain scores.
Results
There were 22 adverse events among 809 LPs performed, a rate of 2.72% (95% CI 1.71–4.09%). Patient hospital stay did not increase due to adverse events. Four patients (0.49%) developed a post-lumbar puncture headache (PLPH). Twelve patients (1.48%) developed nausea, vasovagal responses, or headaches that did not meet PLPH criteria. Six patients (0.74%) reported lower back pain at the LP site not associated with muscular weakness or paresthesia. The median pain score was 1 [0, 3]; the mode was 0 out of 10.
Conclusions
The LP protocol described herein may reduce adverse event rates and improve patient comfort in future studies.

Similar content being viewed by others
References
Duits FH, Martinez-Lage P, Paquet C, Engelborghs S, Lleo A, Hausner L, Molinuevo JL, Stomrud E, Farotti L, Ramakers I, Tsolaki M, Skarsgard C, Astrand R, Wallin A, Vyhnalek M, Holmber-Clausen M, Forlenza OV, Ghezzi L, Ingelsson M, Hoff EI, Roks G, de Mendonca A, Papma JM, Izagirre A, Taga M, Struyfs H, Alcolea DA, Frolich L, Balasa M, Minthon L, Twisk JWR, Persson S, Zetterberg H, van der Flier WM, Teunissen CE, Scheltens P, Blennow K (2016) Performance and complications of lumbar puncture in memory clinics: results of the multicenter lumbar puncture feasibility study. Alzheimer’s Dement 12(2):154–163. https://doi.org/10.1016/j.jalz.2015.08.003
Monserrate AE, Ryman DC, Ma S, Xiong C, Noble JM, Ringman JM, Morris JC, Danek A, Muller-Sarnowski F, Clifford DB, McDade EM, Brooks WS, Darby DG, Masters CL, Weston PS, Farlow MR, Graff-Radford NR, Salloway SP, Fagan AM, Oliver A, Bateman RJ (2015) Factors associated with the onset and persistence of post-lumbar puncture headache. JAMA Neurol 72(3):325–332. https://doi.org/10.1001/jamaneurol.2014.3974
van Oosterhout WP, van der Plas AA, van Zwet EW, Zielman R, Ferrari MD, Terwindt GM (2013) Postdural puncture headache in migraineurs and nonheadache subjects: a prospective study. Neurology 80(10):941–948. https://doi.org/10.1212/WNL.0b013e3182840bf6
Vidoni ED, Morris JK, Raider K, Burns JM, Alzheimer's Disease Neuroimaging I (2014) Reducing post-lumbar puncture headaches with small bore atraumatic needles. J Clin Neurosci 21(3):536–537. https://doi.org/10.1016/j.jocn.2013.07.001
Connick RM, Connick P, Klotsas AE, Tsagkaraki PA, Gkrania-Klotsas E (2009) Procedural confidence in hospital based practitioners: implications for the training and practice of doctors at all grades. BMC Med Educ 9:2. https://doi.org/10.1186/1472-6920-9-2
Howell JC, Parker MW, Watts KD, Kollhoff A, Tsvetkova DZ, Hu WT (2016) Research lumbar punctures among African Americans and Caucasians: perception predicts experience. Front Aging Neurosci 8:296. https://doi.org/10.3389/fnagi.2016.00296
Giattino CM, Gardner JE, Sbahi FM, Roberts KC, Cooter M, Moretti E, Browndyke JN, Mathew JP, Woldorff MG, Berger M, Investigators M-P (2017) Intraoperative frontal alpha-band power correlates with preoperative neurocognitive function in older adults. Front Syst Neurosci 11:24. https://doi.org/10.3389/fnsys.2017.00024
Berger M, Oyeyemi D, Olurinde MO, Whitson HE, Weinhold KJ, Woldorff MG, Lipsitz LA, Moretti E, Giattino CM, Roberts KC, Zhou J, Bunning T, Ferrandino M, Scheri RP, Cooter M, Chan C, Cabeza R, Browndyke JN, Murdoch DM, Devinney MJ, Shaw LM, Cohen HJ, Mathew JP (2019) The INTUIT study: investigating neuroinflammation underlying postoperative cognitive dysfunction. J Am Geriatr Soc 67(4):794–798. https://doi.org/10.1111/jgs.15770
Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp SL, Benzon HT, Brown DL, Heit JA, Mulroy MF, Rosenquist RW, Tryba M, Yuan CS (2010) Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines. Reg Anesth Pain Med 35(1):64–101
Shaikh F, Brzezinski J, Alexander S, Arzola C, Carvalho JC, Beyene J, Sung L (2013) Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta-analysis. BMJ (Clin Res Ed) 346:f1720. https://doi.org/10.1136/bmj.f1720
Tawfik MM, Atallah MM, Elkharboutly WS, Allakkany NS, Abdelkhalek M (2017) Does preprocedural ultrasound increase the first-pass success rate of epidural catheterization before cesarean delivery? A randomized controlled trial. Anesth Analg 124(3):851–856. https://doi.org/10.1213/ane.0000000000001325
Rembach A, Evered LA, Li QX, Nash T, Vidaurre L, Fowler CJ, Pertile KK, Rumble RL, Trounson BO, Maher S, Mooney F, Farrow M, Taddei K, Rainey-Smith S, Laws SM, Macaulay SL, Wilson W, Darby DG, Martins RN, Ames D, Collins S, Silbert B, Masters CL, Doecke JD (2015) Alzheimer’s disease cerebrospinal fluid biomarkers are not influenced by gravity drip or aspiration extraction methodology. Alzheimer’s Res Ther 7(1):71. https://doi.org/10.1186/s13195-015-0157-7
Jabbari A, Alijanpour E, Mir M, Bani Hashem N, Rabiea SM, Rupani MA (2013) Post spinal puncture headache, an old problem and new concepts: review of articles about predisposing factors. Casp J Intern Med 4(1):595–602
Hatfield MK, Handrich SJ, Willis JA, Beres RA, Zaleski GX (2008) Blood patch rates after lumbar puncture with Whitacre versus Quincke 22- and 20-gauge spinal needles. Am J Roentgenol 190(6):1686–1689. https://doi.org/10.2214/AJR.07.3351
Barreras P, Benavides DR, Barreras JF, Pardo CA, Jani A, Faigle R, Bahouth MN (2017) A dedicated lumbar puncture clinic: performance and short-term patient outcomes. J Neurol 264(10):2075–2080. https://doi.org/10.1007/s00415-017-8597-6
Fredrickson MJ, Ball CM, Dalgleish AJ, Stewart AW, Short TG (2009) A prospective randomized comparison of ultrasound and neurostimulation as needle end points for interscalene catheter placement. Anesth Analg 108(5):1695–1700. https://doi.org/10.1213/ane.0b013e31819c29b8
Costantino TG, Parikh AK, Satz WA, Fojtik JP (2005) Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med 46(5):456–461. https://doi.org/10.1016/j.annemergmed.2004.12.026
Grau T, Leipold RW, Conradi R, Martin E (2001) Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand 45(6):766–771. https://doi.org/10.1034/j.1399-6576.2001.045006766.x
Rehman N, Qazi SR (2019) Efficacy of topical benzocaine in maxilla: a randomized controlled trial. Anesth Prog 66(1):24–29. https://doi.org/10.2344/anpr-66-01-01
Engelborghs S, Niemantsverdriet E, Struyfs H, Blennow K, Brouns R, Comabella M, Dujmovic I, van der Flier W, Frölich L, Galimberti D, Gnanapavan S, Hemmer B, Hoff E, Hort J, Iacobaeus E, Ingelsson M, Jan de Jong F, Jonsson M, Khalil M, Kuhle J, Lleó A, de Mendonça A, Molinuevo JL, Nagels G, Paquet C, Parnetti L, Roks G, Rosa-Neto P, Scheltens P, Skårsgard C, Stomrud E, Tumani H, Visser PJ, Wallin A, Winblad B, Zetterberg H, Duits F, Teunissen CE (2017) Consensus guidelines for lumbar puncture in patients with neurological diseases. Alzheimers Dement 8:111–126. https://doi.org/10.1016/j.dadm.2017.04.007
Dakka Y, Warra N, Albadareen RJ, Jankowski M, Silver B (2011) Headache rate and cost of care following lumbar puncture at a single tertiary care hospital. Neurology 77(1):71–74. https://doi.org/10.1212/WNL.0b013e318220abc0
Acknowledgements
The members of the MADCO-PC and INTUIT Investigators Teams are: CL Amundsen, P Avasarala, MF Berry, DG Blazer, MP Bolognesi, R Brassard, BE Brigman, JN Browndyke, V Cai, J Carter, J Chapman, C Chen, V Cheong, S Christensen, HJ Cohen, JK DeOrio, TA D’Amico, D Erdmann, RM Esclamado, B Funk, S Grant, J Guercio, DK Gupta, DH Harpole, MG Hartwig, ST Hollenbeck, E Iboaya, BA Inman, DW Jang, J Kaisen, A Khan, R Huang, S Lagoo-Deenadayalan, PS Lee, WT Lee, J Lemm, H Levinson, ME Lipkin, D McDonagh, D Murdoch, CR Mantyh, DL McDonagh, J Migaly, SK Mithani, P Mosca, D Murdoch, MF Newman, K Ni, MW Onaitis, D Oyeyemi, TN Pappas, AN Perez, AC Peterson, TJ Polascik, A Podgoreanu, P Potash, GM Preminger, QJ Quinones, EN Rampersaud, A Renne, CN Robertson, SA Roman, S Runyon, CD Scales, S Smani, K Smith, M Stang, A Syed, L Talbot, JKM Thacker, J Thomas, BC Tong, Y Toulgoat-Dubois, A Tu, SN Vaslef, N Waldron, X Wang, K Weinhold, SS Wellman, H Whitson, T Wickenheisser, S Zani.
Funding
This work was supported by National Institutes of Health (Bethesda, Maryland) T32 Grant No. GM08600 (to MB), an International Anesthesia Research Society (IARS; San Francisco, California) Mentored Research Award (to MB), National Institutes of Health R03 AG050918 (to MB), National Institutes of Health Beeson K76 AG057022 (to MB), a Jahnigen Scholars Fellowship award from the American Geriatrics Society (New York, New York) and the Foundation for Anesthesia Education and Research (to MB), additional support from National Institutes of Health P30AG028716, and Duke Anesthesiology departmental funds.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
MB acknowledges income from legal consulting cases related to postoperative cognition in older adults, and material support from Massimo for a study unrelated to the data presented here. MB has also taken part in a peer-to-peer consulting session for Massimo, for which his honorarium was donated (at his request) to the Foundation for Anesthesia Education and Research. The other authors declare that they have no conflict of interest.
Ethical standards
These studies were conducted with approval from the Duke IRB (Pro00083288, Pro00045180) and are registered with clinicaltrials.gov (NCT01993836, NCT03273335). All persons gave their informed consent prior to their inclusion in the study.
Additional information
The members of the MADCO-PC and INTUIT Investigators Teams are listed in “Acknowledgements”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1. Supplemental Figure 1. Video showing the lumbar puncture procedure. (MP4 40391 kb)
415_2020_9797_MOESM2_ESM.tiff
Supplementary file2. Supplemental Figure 2. Ultrasound image showing spine anatomy to guide needle placement during LP. AP articular process, L lamina, TP transverse process, AC anterior complex (anterior dura and posterior longitudinal ligament of vertebrae). Red arrowheads: posterior complex (posterior dura and ligamentum flavum). Dotted line: distance from skin to posterior complex (in this case, about 3.2 cm). Solid line: anteroposterior diameter of the spinal canal. (TIFF 2033 kb)
415_2020_9797_MOESM3_ESM.tiff
Supplementary file3. Supplemental Figure 3. Plot of pain scores compared by pre-operative (BL), 24-h, 6-week, and 1-year post-operative LPs. Means are plotted with Q1, Q3 and SD. Non-parametric Kruskal–Wallis test was used to compare scores over time. There was no evidence of a difference in score by visit (p = 0.44). (TIFF 26 kb)
Rights and permissions
About this article
Cite this article
Nobuhara, C.K., Bullock, W.M., Bunning, T. et al. A protocol to reduce self-reported pain scores and adverse events following lumbar punctures in older adults. J Neurol 267, 2002–2006 (2020). https://doi.org/10.1007/s00415-020-09797-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09797-1