Abstract
Background
Cerebellar ataxia is characterized by difficulty in the planning of movement and lack of anticipatory postural adjustments, which can result in deficits of balance. Being able to have quantitative measurements in clinical practice, to detect any improvements on balance resulting from new rehabilitation treatments or experimental drugs is very important.
Aim
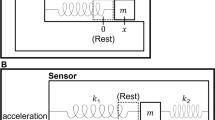
The purpose of this study was to develop an application (APP) able to assess static and dynamic balance in patients with cerebellar ataxias (CA). The APP that works by a wearable device (smartphone) placed at the breastbone level and immobilized by an elastic band, measures the body sway by means of a triaxial accelerometer.
Methods
We investigated 40 CA patients and 80 healthy subjects. All patients were clinically evaluated using the “Berg Balance Scale” (BBS) and the “Scale for the Assessment and Rating of Ataxia” (SARA). Balance impairment was quantitatively assessed using a validated static balance evaluating systems, i.e., Techno-body Pro-Kin footboard. All participants underwent static and dynamic balance assessments using the new APP.
Results
We observed a strong correlation between the APP measurements and the score obtained with the BBS, SARA, and Pro-Kin footboard. The intra-rater reliability and the test–retest reliability of the APP measurements, estimated by intraclass correlation coefficient, were excellent. The standard error of measurement and the minimal detectable change were small. No learning effect was observed.
Conclusions
We can state that the APP is an easy, reliable, and valid evaluating system to quantify the trunk sway in a static position and during the gait.




Similar content being viewed by others
References
Di Donato S, Gellera C, Mariotti C (2001) The complex clinical and genetic classification of inherited ataxias II autosomal recessive ataxias. Neurol Sci 22:219–228
Embiruçu EK, Martyn ML, Schlesinger D, Kok F (2009) Autosomal recessive ataxias: 20 types and counting. Arq Neuropsiquiatr 67:1143–1156
Shakkottai VG, Fogel BL (2013) Clinical neurogenetics: autosomal dominant spinocerebellar ataxia. Neurol Clin 31:987–1007
Friedreich N (1863) Uber degenerative Atrophie der spinalen Hinterstrange, Virchow’s Arch. Pathol Anat 26:391–419
Musselman KE, Stoyanov CT, Marasigan R, Jenkins ME, Konczak J, Morton SM et al (2014) Prevalence of ataxia in children: a systematic review. Neurology 82:80–89
Teive HA, Moro A, Moscovich M, Arruda WO, Munhoz RP, Raskin S et al (2015) Ataxia-telangiectasia. A historical review and a proposal for a new designation: ATM syndrome. J Neurol Sci 355(1–2):3–6
Stevanin G, Durr A, Brice A (2002) Spinocerebellar ataxias caused by polyglutamine expansions. Adv Exp Med Biol 516:47–77
Bodranghien F, Bastian A, Casali C, Hallett M, Louis ED, Manto M et al (2016) Consensus paper: revisiting the symptoms and signs of cerebellar syndrome. Cerebellum 15(3):369–391
Patel M, Isaacs CJ, Seyer L, Brigatti K, Gelbard S, Strawer C et al (2016) Progression of Friedreich ataxia: quantitative characterization over 5 years. Ann Clin Transl Neurol 3:684–694
Reetz K, Dogan I, Hilgers RD, Giunti P, Mariotti C, Durr A et al (2016) Biological and clinical characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS) cohort: a cross-sectional analysis of baseline data. Lancet Neurol 15:1346–1354
Diallo A, Jacobi H, Cook A, Labrum R, Durr A, Brice A et al (2018) Survival in patients with spinocerebellar ataxias types 1,2,3 and 6 (EUROSCA): a longitudinal cohort study. Lancet Neurol 17:327–334
Schmitz-Hübsch T, du Montcel ST, Balik L, Berciano J, Boesch S, Depondt C et al (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66:1717–1720
Schmitz-Hübsch T, Tezenas-Du-Montcel S, Baliko L, Boesch S, Bonato S, Fancellu R et al (2005) Reliability and validity of the international cooperative ataxia rating scale: a study in 156 spinocerebellar ataxia patients. Mov Disord 21:699–704
Tison F, Yekhlef F (2002) Application of the international cooperative ataxia scale rating in multiple system atrophy. Mov Disord 17(6):1248–1254
Winser SJ, Smith CM, Hale LA, Claydon LS, Whitney SL (2018) Clinical assessment of balance using BBS and SARAbal in cerebellar ataxia: synthesis of findings of a psychometric property analysis. Hong Kong Physiother J 38(1):53–61
Winser SJ, Smith CM, Hale LA, Claydon LS, Whitney SL, Mehta P (2015) Systematic review of the psychometric properties of balance measures for cerebellar ataxia. Clin Rehabil 29:69–79
Winser SJ, Smith C, Hale LA, Claydon LS, Whitney SL (2015) Balance outcome measures in cerebellar ataxia: a Delphi survey. Disabil Rehabil 37:165–170
Berg K, Wood-Dauphinee S, Williams JI (1995) The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med 27(1):27–36
Berg K, Wood-Dauphinee S, Williams JI (1995) The balance scale: reliability assessment for elderly residents and patients with an acute stroke. Scand J Rehabil Med 27:27–36
Berg K, Maki B, Williams JI, Holliday P, Wood-Dauphinee S (1992) A comparison of clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 73:1073–1083
Berg K, Wood-Dauphinee S, Williams JI, Gayton D (1989) Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 41:304–311
Downs S, Marquez J, Chiarelli P (2013) The Berg Balance Scale has high intra- and inter-rater reliability but absolute reliability varies across the scale: a systematic review. J Physiother 59(2):93–99
Saether R, Helbostad JL, Riphagen II, Vik T (2013) Clinical tools to assess balance in children and adults with cerebral palsy: a systematic review. Dev Med Child Neurol 55(11):988–999
Sorrentino G, Sale P, Solaro C, Rabini A, Cerri CG, Ferriero G (2018) Clinical measurement tools to assess trunk performance after stroke: a systematic review. Eur J Phys Rehabil Med 54(5):772–784
Verheyden G, Nieuwboer A, Van de Winckel A, De Weerdt W (2007) Clinical tools to measure trunk performance after stroke: a systematic review of the literature. Clin Rehabil 21(5):387–394
Winser SJ, Smith CM, Hale LA, Claydon LS, Whitney SL, Mehta P (2015) Systematic review of the psychometric properties of balance measures for cerebellar ataxia. Clin Rehabil 29(1):69–79
Milne SC, Murphy A, Georgiou-Karistianis N, Yiu EM, Delatycki MB, Corben LA (2018) Psychometric properties of outcome measures evaluating decline in gait in cerebellar ataxia: a systematic review. Gait Posture 61:149–162
Pérennou D, Decavel P, Manckoundia P, Penven Y, Mourey F, Launay F et al (2005) Evaluation of balance in neurologic and geriatric disorders. Ann Readapt Med Phys 48(6):317–335
Yelnik A, Bonan I (2008) Clinical tools for assessing balance disorders. Neurophysiol Clin 38(6):439–445
Petró B, Papachatzopoulou A, Kiss RM (2017) Devices and tasks involved in the objective assessment of standing dynamic balancing—a systematic literature review. PLoS One 12(9):e0185188
Smith C, Claydon LS, Hale L, Winser S (2013) Outcome measures for the assessment of balance and posture control in cerebellar ataxia. Phys Ther Rev 18(2):117
Proessel F, Swanson CW, Rudroff T, Fling BW, Tracy BL (2018) Good agreement between smart device and inertial sensor-based gait parameters during a 6-min walk. Gait Posture 64:63–67
Shirai S, Yabe I, Matsushima M, Ito YM, Yoeyamsa M, Sasaki H (2015) Quantitative evaluation of gait ataxia by accelerometers. J Neurol Sci 358(1–2):253–258
Okajima Y, Chino N, Noda Y, Takahashi H (1990) Accelerometric evaluation of ataxic gait: therapeutic uses of weighting and elastic bandage. Int Disabil Stud 12(4):165–168
Patterson JA, Amick RZ, Thummar T, Rogers ME (2014) Validation of measures from the smartphone sway balance application: a pilot study. Int J Sports Phys Ther 9(2):135–139
Galán-Mercant A, Barón-López FJ, Labajos-Manzanares MT, Cuesta-Vargas AI (2014) Reliability and criterion-related validity with a smartphone used in timed-up-and-go test. Biomed Eng Online 13:156
Daneault JF, Carignan B, Codère CÉ, Sadikot AF, Duval C (2013) Using a smart phone as a standalone platform for detection and monitoring of pathological tremors. Front Hum Neurosci 6:357
Clark RA, Bryant AL, Pua Y, McCrory P, Bennell KM (2010) Hunt validity and reliability of the Nintendo Wii balance board for assessment of standing balance. Gait Posture 31:307–310
Mauch M, Kälin X (2011) Reliability of the ProKin Type B line system (TechnoBod) balance system https://www.woodway.com/sites/default/files/manuals/reliability_prokinb_line_system.pdf. Accessed 06 Jan 2018
Saadat M, Salehi R, Negahban H, Jafar Shaterzadeh M, Mehravar M, Hessam M (2018) Postural stability in patients with non-specific chronic neck pain: a comparative study with healthy people. Med J Islam Repub Iran 32:33
Cattaneo D, Jonsdottir J (2009) Sensory impairments in quiet standing in subjects with multiple sclerosis. Mult Scler J 15(1):59–67
Zhao W, You H, Jiang S, Zhang H, Yang Y, Zhang M (2019) Effect of Pro-kin visual feedback balance training system on gait stability in patients with cerebral small vessel disease. Medicine 98(7):e14503
You H, Zhang H, Liu J, Han T, Zhang M, Zhao W, Jiang S (2017) Effect of balance training with Pro-kin system on balance in patients with white matter lesions. Medicine 96(51):e9057
Portney LG, Watkins MP (2009) Foundations of clinical research: applications to practice. Pearson/Prentice Hall, Upper Saddle River
Portney LG, Watkins MP (2000) Foundations of clinical research: applications to practice. Pearson/Prentice Hall, Upper Saddle River
Wamper KE, Sierevelt IN, Poolman RW, Bhandari M, Haverkamp D (2010) The Harris hip score: do ceiling effects limit its usefulness in orthopedics? Acta Orthop 81(6):703–707
McHorney CA, Tarlov AR (1995) Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res 4(4):293–307
Everitt BS (2002) The Cambridge dictionary of statistics, 2nd edn. CUP, Cambridge
Cone BL, Levy SS, Goble DJ (2015) Wii Fit exer-game training improves sensory weighting and dynamic balance in healthy young adults. Gait Posture 41(2):711–715
Goble DJ, Cone BL, Fling BW (2014) Using the Wii Fit as a tool for balance assessment and neurorehabilitation: the first half decade of “Wii-search”. J Neuroeng Rehabil 11:12
Foo J, Paterson K, Williams G, Clark R (2013) Low-cost evaluation and real-time feedback of static and dynamic weight bearing asymmetry in patients undergoing in-patient physiotherapy rehabilitation for neurological conditions. J Neuroeng Rehabil 10:74
Peterson S (2018) Telerehabilitation booster sessions and remote patient monitoring in the management of chronic low back pain: a case series. Physiother Theory Pract 34(5):393–402
Lee Y, Yeh H, Kim KH, Choi O (2017) A real-time fall detection system based on the acceleration sensor of smartphone. Int J Control Autom 10(1):315–326
Mao A, Ma X, He Y, Luo J (2017) Highly portable, sensor-based system for human fall monitoring. Sensors (Basel) 17(9):2096
Author information
Authors and Affiliations
Contributions
GA contributed to structuring study design, developing the application, subject recruitment, data collection, data review, data analysis, data interpretation, writing and revising the manuscript. CM contributed to structuring study design, data interpretation, writing and revising the manuscript. RA contributed to developing the application. GD contributed to writing the manuscript, statistical data analysis, and revising the manuscript. CG contributed to recruiting patients and data collection. FP contributed to structuring study design, data analysis, and data interpretation. CC contributed to structuring study design, subject recruitment, data analysis, data interpretation, writing and revising the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The manuscript has been approved by all the authors. The authors declare that they have no financial or any kind of relationships that might lead to a conflict of interests.
Ethical standards
This study was conducted in the Department of Medical and Surgical Sciences and Biotechnologies, “Sapienza” University of Rome, at “Marco Pasquali” Institute—ICOT (Latina), from January 2018 to October 2018. All patients who participated in the study were informed of the use of measurements for research purposes and gave their written informed consent. All the procedures performed were in accordance with the ethical standards of the institutional and national research committee. The regulations of our institution concerning intellectual property have been respected. The ethical standards, laid down in 1964 Declaration of Helsinki and its later amendments, were respected.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arcuria, G., Marcotulli, C., Amuso, R. et al. Developing a smartphone application, triaxial accelerometer-based, to quantify static and dynamic balance deficits in patients with cerebellar ataxias. J Neurol 267, 625–639 (2020). https://doi.org/10.1007/s00415-019-09570-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09570-z