Abstract
Background
Spinal cord (SC) involvement correlates with poor prognosis in patients with multiple sclerosis (MS). Nevertheless, there is no consensus on the use of SC-MRI at follow-up, mainly because of the belief that SC lesions are nearly always symptomatic.
Objectives
The aim of the present study was to investigate the frequency of asymptomatic SC combined unique activity (CUA, new/enlarging T2 or gadolinium-positive [Gd+] lesions) on MRI in a cohort of patients diagnosed with clinically isolated syndrome (CIS) or relapsing–remitting MS (RRMS).
Methods
We retrospectively investigated all scans showing SC-CUA in patients with CIS or RRMS referred to a single Italian MS centre. We determined whether they were symptomatic and whether they had associated brain radiological activity.
Results
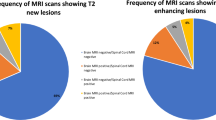
In 340 SC-MRI scans with SC-CUA (230 patients), SC-CUA was asymptomatic in 31.2%; 12.1% of SC-CUA had neither clinical activity nor brain radiological activity (44.5% and 25.4%, respectively, considering only follow-up SC-CUA). At multivariate analysis asymptomatic SC-CUAs were associated with older age at onset (34.0 ± 10.37 vs 31.0 ± 9.99 years, p = 0.006), non-spinal onset (76.4 vs 47.4%, p < 0.001), lower EDSS score at MRI (1.8 ± 0.93 vs 2.4 ± 1.28, p = 0.001) and lower number of Gd+ SC lesions (0.1 ± 0.33 vs 0.3 ± 0.54, p = 0.04), compared to symptomatic SC-CUAs.
Conclusions
A substantial proportion of our patients had SC-CUA without clinical symptoms and/or without concomitant brain MRI activity. In these patients, SC-CUA was the only sign of disease activity, suggesting that regular SC-MRI follow-up is required for reliable assessment of radiological activity and may improve the management of patients with MS.


Similar content being viewed by others
References
Kearney H, Miller DH, Ciccarelli O (2015) Spinal cord MRI in multiple sclerosis—diagnostic, prognostic and clinical value. Nat Rev Neurol 11:327–338
Muccilli A, Seyman E, Oh J (2018) Spinal cord MRI in multiple sclerosis. Neurol Clin 36:35–57
Arrambide G, Rovira A, Sastre-Garriga J et al (2018) Spinal cord lesions: a modest contributor to diagnosis in clinically isolated syndromes but a relevant prognostic factor. Mult Scler 24:301–312
Brownlee WJ, Altmann DR, Alves Da Mota P et al (2017) Association of asymptomatic spinal cord lesions and atrophy with disability 5 years after a clinically isolated syndrome. Mult Scler 23:665–674
Sombekke MH, Wattjes MP, Balk LJ et al (2013) Spinal cord lesions in patients with clinically isolated syndrome: a powerful tool in diagnosis and prognosis. Neurology 80:69–75
Okuda DT, Mowry EM, Cree BA et al (2011) Asymptomatic spinal cord lesions predict disease progression in radiologically isolated syndrome. Neurology 76:686–692
Filippi M, Rocca MA, Ciccarelli O et al (2016) MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guideline. Lancet Neurol 15:292–303
Traboulsee A, Simon JH, Stone L et al (2016) Revised recommendations of the consortium of MS centers task force for a standardized MRI protocol and clinical guidelines for the diagnosis and follow-up of multiple sclerosis. AJNR Am J Neuroradiol 37:394–401
Sormani MP, Bruzzi P (2013) MRI lesions as a surrogate for relapses in multiple sclerosis: a meta-analysis of randomised trials. Lancet Neurol 12:669–676
Wattjes MP, Rovira À, Miller D et al (2015) Evidence based guidelines: MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis—establishing disease prognosis and monitoring patients. Nat Rev Neurol 11:597–606
Cortese R, Ciccarelli O (2018) Clinical monitoring of multiple sclerosis should routinely include spinal cord imaging—yes. Mult Scler 24:1536–1537
Kearney H (2018) Clinical monitoring of multiple sclerosis should routinely include spinal cord imaging—no. Mult Scler 24:1537–1539
Zecca C, Disanto G, Sormani MP et al (2016) Relevance of asymptomatic spinal MRI lesions in patients with multiple sclerosis. Mult Scler 22:782–791
Thorpe JW, Kidd D, Moseley IF et al (1996) Spinal MRI in patients with suspected multiple sclerosis and negative brain MRI. Brain 119:709–714
Ruggieri S, Logoteta A, Tinelli E et al (2018) Measuring disease activity in multiple sclerosis: the essential role of spinal cord MRI monitoring. ECTRIMS Online Library. Ruggieri S 2018; 228465 (P621)
Thompson AJ, Banwell BL, Barkhof F et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173
Lublin FD, Reingold SC, Cohen JA et al (2014) Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology 83:278–286
Filippi M, Rocca MA, Bastianello S et al (2013) Guidelines from the Italian neurological and neuroradiological societies for the use of magnetic resonance imaging in daily life clinical practice of multiple sclerosis patients. Neurol Sci 34:2085–2093
Sormani MP, Gasperini C, Romeo M et al (2016) Assessing response to interferon-b in a multicenter dataset of patients with MS. Neurology 87:134–140
Eckstein C, Syc S, Saidha S (2011) Differential diagnosis of longitudinally extensive transverse myelitis in adults. Eur Neurol J 3:27–39
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
F. Granella has received research grants for his Institution from Biogen and Sanofi Genzyme; has served on scientific advisory boards for Biogen, Novartis, Sanofi Genzyme, Roche and Merck Serono; and has received funding for travel from Biogen, Merck Serono and Sanofi Genzyme. E. Tsantes served on scientific advisory boards for Roche and Merck & Co; has received funding for travel from Biogen, Merck & Co, Sanofi Genzyme and Roche V. Bazzurri has received funding for travel from Sanofi Genzyme, Biogen and Roche. E. Curti served on scientific advisory boards for Merck & Co and Novartis; has received funding for travel from Biogen, Merck & Co, Teva Pharmaceutical Industries, Sanofi Genzyme, Roche and Novartis. S. Graziuso and G. Crisi have nothing to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Granella, F., Tsantes, E., Graziuso, S. et al. Spinal cord lesions are frequently asymptomatic in relapsing–remitting multiple sclerosis: a retrospective MRI survey. J Neurol 266, 3031–3037 (2019). https://doi.org/10.1007/s00415-019-09526-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09526-3