Abstract
Tinnitus, the perception of sound in the absence of external stimuli, is often a disturbing symptom for which the underlying functional neuroanatomy still remains poorly understood. Most studies have focused solely on functional connectivity changes in the auditory cortex of tinnitus patients. The aim of this study was to investigate whether a correlation exists between tinnitus behavioural scores and functional brain connectivity of five resting-state networks comprising the auditory, the default mode, the external control left and right, and the salience network. For this purpose, a large sample of one hundred and thirty-five subjects underwent resting-state functional magnetic resonance imaging and their behavioural scores were obtained using clinical evaluations. Networks were extracted using independent component analysis, and functional connectivity patterns in the extracted networks were evaluated by a graph theoretical approach. The effects of tinnitus for each network were investigated by correlating the graph strength of all the regions with the tinnitus behavioural scores using stepwise fit regression analysis. Results indicated that alterations of functional interactions between key neural circuits of the brain are not limited to one single network. In particular, tinnitus distress showed a strong correlation with the connectivity pattern within and between the right executive control network and the other four resting-state networks, indicating that tinnitus distress is probably the consequence of a hyperactive attention condition. Among the behavioural scores, the strongest correlation was observed between age and hearing loss, while the tinnitus objective loudness was not correlated with any behavioural scores.



Similar content being viewed by others
References
Jastreboff PJ (1990) Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 8(4):221–254
Shargorodsky J, Curhan GC, Farwell WR (2010) Prevalence and characteristics of tinnitus among US adults. Am J Med 123(8):711–718
Langguth B, Kreuzer PM, Kleinjung T, De Ridder D (2013) Tinnitus: causes and clinical management. Lancet Neurol 12(9):920–930
De Ridder D, Elgoyhen AB, Romo R, Langguth B (2011) Phantom percepts: tinnitus and pain as persisting aversive memory networks. Proc Natl Acad Sci USA 108(20):8075–8080
Eggermont JJ, Roberts LE (2004) The neuroscience of tinnitus. Trends Neurosci 27(11):676–682
Mirz F, Pedersen CB, Ishizu K, Johannsen P, Ovesen T, StÖdkilde-JÖrgensen H, Gjedde A (1999) Positron emission tomography of cortical centers of tinnitus. Heart Res 134(1–2):133–144
Schlee W, Lorenz I, Hartmann T, Müller N, Schulz H, Weisz N (2010) A global brain model of Tinnitus. In: Møller AR, Langguth B, De Ridder D, Kleinjung T (eds) Textbook of tinnitus. Springer, New York, NY
Vanneste S, De Ridder D (2012) The auditory and non-auditory brain areas involved in tinnitus. An emergent property of multiple parallel overlapping subnetworks. Front Syst Neurosci 6:31
Adjamian P, Sereda M, Hall DA (2009) The mechanisms of tinnitus: perspectives from human functional neuroimaging. Heart Res 253(1–2):15–31
Schlee W, Weisz N, Bertrand O, Hartmann T, Elbert T (2008) Using auditory steady state responses to outline the functional connectivity in the tinnitus brain. PLoS One 3(11):e3720
Schlee W et al (2009) Mapping cortical hubs in tinnitus. BMC Biol 7:80
Langguth B et al (2012) Neuroimaging and neuromodulation: complementary approaches for identifying the neuronal correlates of tinnitus. Front Syst Neurosci 6:15
Elgoyhen AB, Langguth B, De Ridder D, Vanneste S (2015) Tinnitus: perspectives from human neuroimaging. Nat Rev Neurosci 16(10):632–642
Buckner RL et al (2009) Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer’s disease. J Neurosci 29(6):1860–1873
Bressler SL, Menon V (2010) Large-scale brain networks in cognition: emerging methods and principles. Trends Cogn Sci 14:277–290. https://doi.org/10.1016/j.tics.2010.04.004
Fox MD, Raichle ME (2007) Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci 8:700–711
Biswal B, Yetkin FZ, Haughton VM, Hyde JS (1995) Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med 34:537–541
Damoiseaux JS, Rombouts SA, Barkhof F et al (2006) Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci USA 103(37):13848–13853
Moussa MN, Steen MR, Laurienti PJ, Hayasaka S (2012) Consistency of network modules in resting-state FMRI connectome data. PLoS One 7(8):e44428
Vanneste S, Plazier M, van der Loo E, Van de Heyning P, De Ridder D (2011) The difference between uni- and bilateral auditory phantom percept. Clin Neurophysiol 122(3):578–587
Vanneste S, van de Heyning P, De Ridder D (2011) The neural network of phantom sound changes over time: a comparison between recent-onset and chronic tinnitus patients. Eur J Neurosci 34(5):718–731
Schecklmann M et al (2013) Neural correlates of tinnitus duration and distress: a positron emission tomography study. Hum Brain Mapp 34(1):233–240
Maudoux A, Lefebvre P, Demertzi A, Cabay JE, Vanhaudenhuyse A, Laureys S, Soddu A (2012) Connectivity graph analysis of the auditory resting state network in tinnitus. Brain Res 1485:10–21
Schmidt SA, Akrofi K, Carpenter-Thompson JR, Husain FT (2013) Default mode, dorsal attention and auditory resting state networks exhibit differential functional connectivity in tinnitus and hearing loss. PLoS One 8(10):e76488. https://doi.org/10.1371/journal.pone.0076488
Hallam RS (1996) Manual of the Tinnitus Questionnaire (TQ). Psychological Corporation, London
Ribeiro de Paula D, Ziegler E, Abeyasinghe PM et al (2017) A method for independent component graph analysis of resting-state fMRI. Brain Behav 7(3):e00626. https://doi.org/10.1002/brb3.626
Beckmann CF, DeLuca M, Devlin JT, Smith SM (2005) Investigations into resting-state connectivity using independent component analysis. Philos Trans R Soc Lond B Biol Sci 360(1457):1001–1013
Holmes A, Friston K (1998) Generalisability, random effects and population inference. NeuroImage 7:754
Demertzi A, Gomez F, Crone JS, Vanhaudenhuyse A, Tshibanda L, Noirhomme Q, Thonnard M, Charland-Verville V, Kirsch M, Laureys S, Soddu A (2014) Multiple fMRI system-level baseline connectivity is disrupted in patients with consciousness alterations. Cortex 52:35–46
Soddu A, Vanhaudenhuyse A, Bahri M, Bruno MA, Boly M, Demertzi A, Tshibanda JF et al (2012) Identifying the default mode component in spatial IC analysis of patients with disorders of consciousness. Hum Brain Mapp 33(4):778–796
Maudoux A et al (2012) Auditory resting-state network connectivity in tinnitus: a functional MRI study. PLoS One 7(5):e36222
Gerhard S, Daducci A, Lemkaddem A, Meuli R, Thiran JP, Hagmann P (2011) The connectome viewer toolkit: an open source framework to manage, analyze, and visualize connectomes. Front Neuroinform 5:3
Cavaliere C, Kandeepan S et al (2018) Multimodal neuroimaging approach to variability of functional connectivity in disorders of consciousness: a PET/MRI Pilot study. Front Neurol 9:861. https://doi.org/10.3389/fneur.2018.00861
Chen Y-C, Chen H, Bo F et al (2018) Tinnitus distress is associated with enhanced resting-state functional connectivity within the default mode network. Neuropsychiatr Dis Treat 14:1919–1927. https://doi.org/10.2147/NDT.S164619
Trevis KJ, McLachlan NM, Wilson SJ (2016) Cognitive mechanisms in chronic tinnitus: psychological markers of a failure to switch attention. Front Psychol 7:1262. https://doi.org/10.3389/fpsyg.2016.01262
Hair JF Jr, Anderson RE, Tatham RL, Black WC (1995) Multivariate Data Analysis, 3rd edn. Macmillan, New York
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 57:289–300
World Health Organization (1991) Grades of hearing impairment. Hearing Network News 1
Bhatt JM, Lin HW, Bhattacharyya N (2016) Tinnitus epidemiology: prevalence, severity, exposures and treatment patterns in the United States: Bhatt JM: Tinnitus in the United States. JAMA Otolaryngol Head Neck Surg 142(10):959–965. https://doi.org/10.1001/jamaoto.2016.1700
Zanto TP, Gazzaley A (2013) Fronto-parietal network: flexible hub of cognitive control. Trends Cogn Sci 17(12):602–603
Boveroux P, Vanhaudenhuyse A, Bruno MA, Noirhomme Q, Lauwick S, Luxen A, Degueldre C, Plenevaux A, Schnakers C, Phillips C, Brichant JF, Bonhomme V, Maquet P, Greicius MD, Laureys S, Boly M (2010) Breakdown of within- and between-network resting state functional magnetic resonance imaging connectivity during propofol-induced loss of consciousness. Anesthesiology 113:1038–1053
Liu X, Lauer KK, Ward BD, Rao SM, Li SJ, Hudetz AG (2012) Propofol disrupts functional interactions between sensory and high-order processing of auditory verbal memory. Hum Brain Mapp 33:2487–2498
Dosenbach NU, Fair DA, Cohen AL, Schlaggar BL, Petersen SE (2008) A dual-networks architecture of top-down control. Trends Cogn Sci 12(3):99–105
Fassbender C, Simoes-Franklin C, Murphy K, Hester R, Meaney J, Robertson IH, Garavan H (2006) The role of a right fronto-parietal network in cognitive control. J Psychophysiol 20(4):286–296. https://doi.org/10.1027/0269-8803.20.4.286
Power JD, Cohen AL, Nelson SM, Wig GS, Barnes KA, Church JA, Vogel AC, Laumann TO, Miezin FM, Schlaggar BL, Petersen SE (2011) Functional network organization of the human brain. Neuron 72(4):665–678
Guldenmund P, Gantner IS, Baquero K, Das T, Demertzi A, Boveroux P, Bonhomme V, Vanhaudenhuyse A, Bruno MA, Gosseries O, Noirhomme Q (2016) Propofol-induced frontal cortex disconnection: a study of resting-state networks, total brain connectivity, and mean BOLD signal oscillation frequencies. Brain Connect 6(3):225–237
Sadaghiani S, Hesselmann G, Kleinschmidt A (2009) Distributed and antagonistic contributions of ongoing activity fluctuations to auditory stimulus detection. J Neurosci 29(42):13410–13417
Chadick JZ, Gazzaley A (2011) Differential coupling of visual cortex with default or frontal-parietal network based on goals. Nat Neurosci 14(7):830
Wallhausser-Franke E et al (2012) Tinnitus: distinguishing between subjectively perceived loudness and tinnitus-related distress. PLoS One 7(4):e34583
Vidal-Piñeiro D et al (2014) Decreased default mode network connectivity correlates with age-associated structural and cognitive changes. Front Aging Neurosci 6:256
Washington SD, VanMeter JW (2015) Anterior-posterior connectivity within the default mode network increases during maturation. Int J Med Biol Front 21(2):207
Ferreira LK, Regina AC, Kovacevic N, Martin MD, Santos PP, Carneiro CD, Kerr DS, Amaro E Jr, McIntosh AR, Busatto GF (2016) Aging effects on whole-brain functional connectivity in adults free of cognitive and psychiatric disorders. Cereb Cortex 26(9):3851–3865
Meyer M, Luethi MS, Neff P, Langer N and Büchi S (2014) Disentangling Tinnitus Distress and Tinnitus presence by means of EEG power analysis. Neural Plast. https://doi.org/10.1155/2014/468546
Schlee W, Kleinjung T, Hiller W, Goebel G, Kolassa IT, Langguth B (2011) Does tinnitus distress depend on age of onset? PLoS One 6(11):e27379
Brüggemann P, Szczepek AJ, Rose M, McKenna L, Olze H, Mazurek B (2016) Impact of multiple factors on the degree of tinnitus distress. Front Human Neurosci 10:341
Balkenhol T, Wallhausser-Franke E, Delb W (2013) Psychoacoustic tinnitus loudness and tinnitus-related distress show different associations with oscillatory brain activity. PLoS One 8(1):e53180
Tyler RS, Conrad-Armes D (1983) The determination of tinnitus loudness considering the effects of recruitment. J Speech Hear Res 26(1):59–72
Acknowledgements
The authors thank the technicians of the Department of Radiology for their active participation in the MRI studies in tinnitus patients. This research was funded by Research Foundation Flanders (FWO), Tinnitus Research Initiative (TRI), TOP financiering from University Antwerp, the Belgian National Funds for Scientific Research—FNRS (F 5/4/150/5—MCF/SD—9853), the Tinnitus Prize 2011 (FNRS 9.4501.12), and the European Commission. Finally, we gratefully acknowledge the financial support provided by NSERC Discovery grant (05578-2014RGPIN).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
The study was approved by the Ethics Committee of the Antwerp University Hospital. Informed consent to participate in the study was obtained from the patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
415_2019_9390_MOESM2_ESM.tif
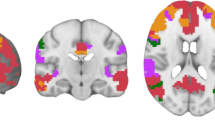
ESM_2 Axial and sagittal views of the masks of nine Resting State Network (RSN)s a) using all the regions (overlapping) belonging to the network b) using isolated regions (non-overlapping) only (TIFF 1521 kb)
415_2019_9390_MOESM3_ESM.docx
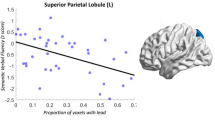
ESM_3 Correlation between BS and GS for tinnitus patients. a) Correlation between the age and GS on the auditory network. b) Correlation between the duration and GS on the DMN network. c) Correlation between the hearing loss and GS on the DMN network. d) Correlation between the subjective intensity (VAS) and GS on the salience network (DOCX 16 kb)
415_2019_9390_MOESM4_ESM.tif
ESM_4 Representation of the correlation between BS and GS of tinnitus patients for a) Aud and age, b) DMN and duration, c) DMN and hearing loss, d) Sal and subjective intensity. NB: The correlation between BS and all the networks are positive except between the Sal and subjective intensity (TIFF 373 kb)
415_2019_9390_MOESM5_ESM.docx
ESM_5 Correlation between BS and GS for tinnitus patients with different types of lateralization. a) Correlation between the distress and GS on the ECNR for bilateral tinnitus patients. b) Correlation between the age and GS on the auditory network for bilateral tinnitus patients. c) Correlation between the age and GS on the DMN for bilateral tinnitus patients. d) Correlation between the distress and GS on the ECNR for unilateral tinnitus patients (DOCX 20 kb)
415_2019_9390_MOESM6_ESM.tif
ESM_6 Representation of the correlation between BS and GS for tinnitus patients with different types of lateralization. a) ECNR and distress for bilateral. b) Aud and age for bilateral. c) DMN and age for bilateral. d) ECNR and distress for unilateral (TIFF 446 kb)
Rights and permissions
About this article
Cite this article
Kandeepan, S., Maudoux, A., Ribeiro de Paula, D. et al. Tinnitus distress: a paradoxical attention to the sound?. J Neurol 266, 2197–2207 (2019). https://doi.org/10.1007/s00415-019-09390-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09390-1