Abstract
Objective
Parkinson’s disease (PD) patients are often unaware of olfactory deficits despite having hyposmia from the early stages. We aimed to evaluate whether olfactory anosognosia is a predictor of cognitive decline in PD.
Methods
In this retrospective cohort study, we recruited 77 PD patients who underwent both olfactory and neuropsychological tests and were followed-up for over 5 years. Based on the degree of olfactory dysfunction and awareness of its presence, patients were classified as normosmic patients (Normosmia group, n = 15), hyposmic patients without olfactory anosognosia (Hyposmia-OA−, n = 40), or hyposmic patients with olfactory anosognosia (Hyposmia-OA+, n = 22). We compared the rates of cognitive decline using linear mixed model and dementia conversion using a survival analysis among the groups.
Results
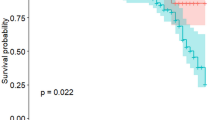
A higher proportion of patients in the Hyposmia-OA+ group had mild cognitive impairment at baseline (77.3%) and dementia converter at follow-up (50.0%). The Hyposmia-OA+ group exhibited a faster decline in frontal executive and global cognitive function than did the Normosmia and Hyposmia-OA− groups. A Kaplan–Meier analysis demonstrated that the conversion rate to dementia was significantly higher in the Hyposmia-OA+ group than in the Normosmia (P = 0.007) and Hyposmia-OA− (P = 0.038) groups. A Cox regression analysis showed that olfactory anosognosia remained a significant predictor of time to develop dementia in the Hyposmia-OA+ group compared to the Normosmia group (adjusted hazard ratio 3.30; 95% confidence interval 1.10–8.21).
Conclusion
This study suggests that olfactory anosognosia is a predictor of cognitive decline and dementia conversion in PD.


Similar content being viewed by others
References
Haehner A, Boesveldt S, Berendse HW, Mackay-Sim A, Fleischmann J, Silburn PA, Johnston AN, Mellick GD, Herting B, Reichmann H, Hummel T (2009) Prevalence of smell loss in Parkinson’s disease—a multicenter study. Parkinsonism Relat Disord 15(7):490–494. https://doi.org/10.1016/j.parkreldis.2008.12.005
Doty RL, Deems DA, Stellar S (1988) Olfactory dysfunction in parkinsonism: a general deficit unrelated to neurologic signs, disease stage, or disease duration. Neurology 38(8):1237–1244
Hawkes CH, Del Tredici K, Braak H (2007) Parkinson’s disease: a dual-hit hypothesis. Neuropathol Appl Neurobiol 33(6):599–614. https://doi.org/10.1111/j.1365-2990.2007.00874.x
Ross GW, Petrovitch H, Abbott RD, Tanner CM, Popper J, Masaki K, Launer L, White LR (2008) Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann Neurol 63(2):167–173. https://doi.org/10.1002/ana.21291
Bohnen NI, Studenski SA, Constantine GM, Moore RY (2008) Diagnostic performance of clinical motor and non-motor tests of Parkinson disease: a matched case-control study. Eur J Neurol 15(7):685–691. https://doi.org/10.1111/j.1468-1331.2008.02148.x
Bohnen NI, Muller ML, Kotagal V, Koeppe RA, Kilbourn MA, Albin RL, Frey KA (2010) Olfactory dysfunction, central cholinergic integrity and cognitive impairment in Parkinson’s disease. Brain 133(Pt 6):1747–1754. https://doi.org/10.1093/brain/awq079
Domellof ME, Lundin KF, Edstrom M, Forsgren L (2017) Olfactory dysfunction and dementia in newly diagnosed patients with Parkinson’s disease. Parkinsonism Relat Disord 38:41–47. https://doi.org/10.1016/j.parkreldis.2017.02.017
Baba T, Kikuchi A, Hirayama K, Nishio Y, Hosokai Y, Kanno S, Hasegawa T, Sugeno N, Konno M, Suzuki K, Takahashi S, Fukuda H, Aoki M, Itoyama Y, Mori E, Takeda A (2012) Severe olfactory dysfunction is a prodromal symptom of dementia associated with Parkinson’s disease: a 3 year longitudinal study. Brain 135(Pt 1):161–169. https://doi.org/10.1093/brain/awr321
Lee DH, Oh JS, Ham JH, Lee JJ, Lee I, Lee PH, Kim JS, Sohn YH (2015) Is normosmic Parkinson disease a unique clinical phenotype? Neurology 85(15):1270–1275. https://doi.org/10.1212/wnl.0000000000001999
White TL, Sadikot AF, Djordjevic J (2016) Metacognitive knowledge of olfactory dysfunction in Parkinson’s disease. Brain Cogn 104:1–6. https://doi.org/10.1016/j.bandc.2016.01.004
Prigatano GP, Schacter DL (1991) Awareness of deficit after brain injury: clinical and theoretical issues. Oxford University Press, New York
Rosen HJ (2011) Anosognosia in neurodegenerative disease. Neurocase 17(3):231–241. https://doi.org/10.1080/13554794.2010.522588
Mak E, Chin R, Ng LT, Yeo D, Hameed S (2015) Clinical associations of anosognosia in mild cognitive impairment and Alzheimer’s disease. Int J Geriatr Psychiatry 30(12):1207–1214. https://doi.org/10.1002/gps.4275
Gerretsen P, Chung JK, Shah P, Plitman E, Iwata Y, Caravaggio F, Nakajima S, Pollock BG, Graff-Guerrero A (2017) Anosognosia is an independent predictor of conversion from mild cognitive impairment to Alzheimer’s disease and is associated with reduced brain metabolism. J Clin Psychiatry 78(9):e1187–e1196. https://doi.org/10.4088/JCP.16m11367
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149(2):351–356. https://doi.org/10.2214/ajr.149.2.351
Gibb WR, Lees AJ (1988) The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 51(6):745–752
Doty RL, Marcus A, Lee WW (1996) Development of the 12-item cross-cultural smell identification test (CC-SIT). Laryngoscope 106(3 Pt 1):353–356
Chung SJ, Lee Y, Lee JJ, Lee PH, Sohn YH (2017) Rapid eye movement sleep behaviour disorder and striatal dopamine depletion in patients with Parkinson’s disease. Eur J Neurol 24(10):1314–1319. https://doi.org/10.1111/ene.13388
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653. https://doi.org/10.1002/mds.23429
Scheltens P, Leys D, Barkhof F, Huglo D, Weinstein HC, Vermersch P, Kuiper M, Steinling M, Wolters EC, Valk J (1992) Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol Neurosurg Psychiatry 55(10):967–972
Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, Na DL (2010) Seoul neuropsychological screening battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci 25(7):1071–1076. https://doi.org/10.3346/jkms.2010.25.7.1071
Litvan I, Goldman JG, Troster AI, Schmand BA, Weintraub D, Petersen RC, Mollenhauer B, Adler CH, Marder K, Williams-Gray CH, Aarsland D, Kulisevsky J, Rodriguez-Oroz MC, Burn DJ, Barker RA, Emre M (2012) Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: movement disorder society task force guidelines. Mov Disord 27(3):349–356. https://doi.org/10.1002/mds.24893
Dubois B, Burn D, Goetz C, Aarsland D, Brown RG, Broe GA, Dickson D, Duyckaerts C, Cummings J, Gauthier S, Korczyn A, Lees A, Levy R, Litvan I, Mizuno Y, McKeith IG, Olanow CW, Poewe W, Sampaio C, Tolosa E, Emre M (2007) Diagnostic procedures for Parkinson’s disease dementia: recommendations from the movement disorder society task force. Mov Disord 22(16):2314–2324. https://doi.org/10.1002/mds.21844
Babinski J (1914) Contribution a l’etude des troubles mentaux dans l’hemiplegie organique cerebrale (anosognosie). Rev Neurol 27:845–848
Wilson RS, Sytsma J, Barnes LL, Boyle PA (2016) Anosognosia in dementia. Curr Neurol Neurosci Rep 16(9):77. https://doi.org/10.1007/s11910-016-0684-z
Maier F, Prigatano GP (2017) Impaired self-awareness of motor disturbances in Parkinson’s Disease. Arch Clin Neuropsychol 32(7):802–809. https://doi.org/10.1093/arclin/acx094
Maier F, Williamson KL, Tahmasian M, Rochhausen L, Ellereit AL, Prigatano GP, Kracht L, Tang CC, Herz DM, Fink GR, Timmermann L, Eggers C (2016) Behavioural and neuroimaging correlates of impaired self-awareness of hypo- and hyperkinesia in Parkinson’s disease. Cortex 82:35–47. https://doi.org/10.1016/j.cortex.2016.05.019
Seltzer B, Vasterling JJ, Mathias CW, Brennan A (2001) Clinical and neuropsychological correlates of impaired awareness of deficits in Alzheimer disease and Parkinson disease: a comparative study. Neuropsychiatry Neuropsychol Behav Neurol 14(2):122–129
Sitek EJ, Soltan W, Wieczorek D, Robowski P, Slawek J (2011) Self-awareness of memory function in Parkinson’s disease in relation to mood and symptom severity. Aging Ment Health 15(2):150–156. https://doi.org/10.1080/13607863.2010.508773
McKinlay A, Grace RC, Dalrymple-Alford JC, Anderson TJ, Fink J, Roger D (2008) Neuropsychiatric problems in Parkinson’s disease: comparisons between self and caregiver report. Aging Ment Health 12(5):647–653. https://doi.org/10.1080/13607860802343225
Kawasaki I, Baba T, Takeda A, Mori E (2016) Loss of awareness of hyposmia is associated with mild cognitive impairment in Parkinson’s disease. Parkinsonism Relat Disord 22:74–79. https://doi.org/10.1016/j.parkreldis.2015.11.015
Zamboni G, Wilcock G (2011) Lack of awareness of symptoms in people with dementia: the structural and functional basis. Int J Geriatr Psychiatry 26(8):783–792. https://doi.org/10.1002/gps.2620
Gainotti G (2018) Anosognosia in degenerative brain diseases: the role of the right hemisphere and of its dominance for emotions. Brain Cogn 127:13–22. https://doi.org/10.1016/j.bandc.2018.08.002
Vannini P, Hanseeuw B, Munro CE, Amariglio RE, Marshall GA, Rentz DM, Pascual-Leone A, Johnson KA, Sperling RA (2017) Anosognosia for memory deficits in mild cognitive impairment: insight into the neural mechanism using functional and molecular imaging. Neuroimage Clin 15:408–414. https://doi.org/10.1016/j.nicl.2017.05.020
Perrotin A, Desgranges B, Landeau B, Mezenge F, La Joie R, Egret S, Pelerin A, de la Sayette V, Eustache F, Chetelat G (2015) Anosognosia in Alzheimer disease: disconnection between memory and self-related brain networks. Ann Neurol 78(3):477–486. https://doi.org/10.1002/ana.24462
Salmon E, Perani D, Herholz K, Marique P, Kalbe E, Holthoff V, Delbeuck X, Beuthien-Baumann B, Pelati O, Lespagnard S, Collette F, Garraux G (2006) Neural correlates of anosognosia for cognitive impairment in Alzheimer’s disease. Hum Brain Mapp 27(7):588–597. https://doi.org/10.1002/hbm.20203
Therriault J, Ng KP, Pascoal TA, Mathotaarachchi S, Kang MS, Struyfs H, Shin M, Benedet AL, Walpola IC, Nair V, Gauthier S, Rosa-Neto P (2018) Anosognosia predicts default mode network hypometabolism and clinical progression to dementia. Neurology 90(11):e932–e939. https://doi.org/10.1212/wnl.0000000000005120
Aarsland D, Bronnick K, Ehrt U, De Deyn PP, Tekin S, Emre M, Cummings JL (2007) Neuropsychiatric symptoms in patients with Parkinson’s disease and dementia: frequency, profile and associated care giver stress. J Neurol Neurosurg Psychiatry 78(1):36–42. https://doi.org/10.1136/jnnp.2005.083113
Macleod AD, Taylor KS, Counsell CE (2014) Mortality in Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 29(13):1615–1622. https://doi.org/10.1002/mds.25898
Parrao T, Chana P, Venegas P, Behrens MI, Aylwin ML (2012) Olfactory deficits and cognitive dysfunction in Parkinson’s disease. Neurodegener Dis 10(1–4):179–182. https://doi.org/10.1159/000335915
Acknowledgements
This study was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI16C1118).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no financial or other conflicts of interest.
Ethical standard
This study was approved by the Institutional Review Board of the Yonsei University Severance Hospital. Written informed consent was obtained from all patients who participated in this study.
Rights and permissions
About this article
Cite this article
Yoo, H.S., Chung, S.J., Lee, Y.H. et al. Olfactory anosognosia is a predictor of cognitive decline and dementia conversion in Parkinson’s disease. J Neurol 266, 1601–1610 (2019). https://doi.org/10.1007/s00415-019-09297-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09297-x