Abstract
Introduction
We sought to analyze the blood pressure (BP) circadian rhythm in Parkinson’s disease (PD), multiple system atrophy (MSA), and pure autonomic failure (PAF) and to evaluate the effect of vasoactive and dopaminergic medications on BP fluctuations during activities of daily living.
Methods
We analyzed data from patients with PD (n = 72), MSA (n = 18), and PAF (n = 17) evaluated with 24-h ambulatory BP monitoring (ABPM) at our Center between 1996 and 2015. Comparisons between groups were performed according to (a) clinical diagnosis and (b) pharmacological treatment. ABPM parameters included 24-h BP variability, BP load, nocturnal dipping, and awakening hypotension.
Results
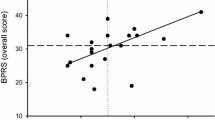
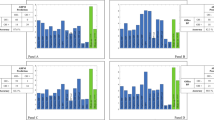
The average BP was 121 ± 14/72 ± 8 mmHg during daytime and 133 ± 20/76 ± 13 mmHg during nighttime (p < 0.01), with BP load of 24 ± 22/15 ± 16% (daytime) vs. 61 ± 36/52 ± 36% (nighttime) (p < 0.01). In-office BP measurements were consistent with OH in 95 patients (89%) and SH in 63 (59%). ABPM demonstrated increased BP variability in 67 patients (63%), awakening hypotension in 63 (59%), “reverse dipping” in 85 (79.4%), “reduced dipping” in 13 (12.1%), and “normal dipping” in 9 (8.4%). No differences were observed between PD, MSA, and PAF, but a sub-analysis of PD patients revealed two distinct patterns of BP alterations. No significant differences were observed in relation to the use of vasoactive or dopaminergic medications.
Conclusion
Regardless of the neurological diagnosis and pharmacological treatment, patients with alpha-synucleinopathies showed a BP circadian rhythm characterized by increased BP variability, reverse dipping, increased BP load, and awakening hypotension.


Similar content being viewed by others
References
Mathias CJ (2003) Autonomic diseases: clinical features and laboratory evaluation. J Neurol Neurosurg Psychiatry 74(Suppl 3):iii31–i41
Milazzo V, Di Stefano C, Milan A, Ravera A, Sobrero G, Sabia L, Veglio F, Maule S (2015) Cardiovascular complications in patients with autonomic failure. Clin Auton Res 25:133–140
Spallone V, Maiello MR, Morganti R, Mandica S, Frajese G (2007) Usefulness of ambulatory blood pressure monitoring in predicting the presence of autonomic neuropathy in type I diabetic patients. J Hum Hypertens 21:381–386
Milazzo V, Di Stefano C, Vallelonga F, Sobrero G, Zibetti M, Romagnolo A, Merola A, Milan A, Espay AJ, Lopiano L, Veglio F, Maule S (2018) Reverse blood pressure dipping as marker of dysautonomia in Parkinson disease. Parkinsonism Relat Disord 56:82–87
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Durr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71:670–676
Singer W, Berini SE, Sandroni P, Fealey RD, Coon EA, Suarez MD, Benarroch EE, Low PA (2017) Pure autonomic failure: predictors of conversion to clinical CNS involvement. Neurology 88:1129–1136
Spallone V, Ziegler D, Freeman R, Bernardi L, Frontoni S, Pop-Busui R, Stevens M, Kempler P, Hilsted J, Tesfaye S, Low P, Valensi P (2011) Cardiovascular autonomic neuropathy in diabetes: clinical impact, assessment, diagnosis, and management. Diabetes Metab Res Rev 27:639–653
Novak P (2011) Quantitative autonomic testing. J Vis Exp 19;(53):pii 2502
Lahrmann H, Cortelli P, Hilz M, Mathias CJ, Struhal W, Tassinari M (2006) EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur J Neurol 13:930–936
Fanciulli A, Jordan J, Biaggioni I et al (2018) Consensus statement on the definition of neurogenic supine hypertension in cardiovascular autonomic failure by the American Autonomic Society (AAS) and the European Federation of Autonomic Societies (EFAS): endorsed by the European Academy of Neurology (EAN) and the European Society of Hypertension (ESH). Clin Auton Res. https://doi.org/10.1007/s10286-018-0529-8
Kaufmann H, Malamut R, Norcliffe-Kaufmann L, Rosa K, Freeman R (2012) The Orthostatic Hypotension Questionnaire (OHQ): validation of a novel symptom assessment scale. Clin Auton Res 22:79–90
Parati G, Stergiou G, O’Brien E et al (2014) European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 32:1359–1366
Mancia G, Fagard R, Narkiewicz K et al (2013) ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34:2159–2219
James G, Witten D, Hastie T, Tibshirani R (2013) An Introduction to statistical learning: with applications in R. Springer texts in Statistics. Springer, New York
Guo Q, Lu X, Gao Y, Zhang J, Yan B, Su D, Song A, Zhao X, Wang G (2017) Cluster analysis: a new approach for identification of underlying risk factors for coronary artery disease in essential hypertensive patients. Sci Rep 7:43965
Parikh KS, Rao Y, Ahmad T, Shen K, Felker GM, Rajagopal S (2017) Novel approach to classifying patients with pulmonary arterial hypertension using cluster analysis. Pulm Circ 7:486–493
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25:2649–2653
Fanciulli A, Strano S, Ndayisaba JP, Goebel G, Gioffrè L, Rizzo M, Colosimo C, Caltagirone C, Poewe W, Wenning GK, Pontieri FE (2014) Detecting nocturnal hypertension in Parkinson’s disease and multiple system atrophy: proposal of a decision-support algorithm. J Neurol 261:1291–1299
Kang SJ, Ahn JY, Kim JS, Cho JW, Kim JY, Choi YY, Kim HT (2016) 24-h ambulatory blood pressure monitoring in SWEDDs patients with Parkinsonism. Can J Neurol Sci 43:390–397
Ejaz AA, Sekhon IS, Munjal S (2006) Characteristic findings on 24-h ambulatory blood pressure monitoring in a series of patients with Parkinson’s disease. Eur J Intern Med 17:417–420
Plaschke M, Trenkwalder P, Dahlheim H, Lechner C, Trenkwalder C (1998) Twenty-four-hour blood pressure profile and blood pressure responses to head-up tilt tests in Parkinson’s disease and multiple system atrophy. J Hypertens 16:1433–1441
Vichayanrat E, Low DA, Iodice V, Stuebner E, Hagen EM, Mathias CJ (2017) Twenty-four-hour ambulatory blood pressure and heart rate profiles in diagnosing orthostatic hypotension in Parkinson’s disease and multiple system atrophy. Eur J Neurol 24:90–97
Arnold AC, Biaggioni I (2012) Management approaches to hypertension in autonomic failure. Curr Opin Nephrol Hypertens 21:481–485
Fanciulli A, Strano S, Colosimo C, Caltagirone C, Spalletta G, Pontieri FE (2013) The potential prognostic role of cardiovascular autonomic failure in alpha-synucleinopathies. Eur J Neurol 20:231–235
Arnold AC, Okamoto LE, Gamboa A, Shibao C, Raj SR, Robertson D, Biaggioni I (2013) Angiotensin II, independent of plasma renin activity, contributes to the hypertension of autonomic failure. Hypertension 61:701–706
Shibao C, Lipsitz LA, Biaggioni I (2013) ASH position paper: evaluation and treatment of orthostatic hypotension. J Clin Hypertens 15:147–153
Tulen JH,, van Steenis HG, Mechelse K (1991) Sleep patterns and blood pressure variability in patients with pure autonomic failure. Clin Auton Res 1:309–315
Milazzo V, Maule S, Di Stefano C, Tosello F, Totaro S, Veglio F, Milan A (2015) Cardiac organ damage and arterial stiffness in autonomic failure: comparison with essential hypertension. Hypertension 66:1168–1175
Maule S, Milan A, Grosso T, Veglio F (2006) Left ventricular hypertrophy in patients with autonomic failure. Am J Hypertens 19:1049–1054
Schillaci G, Bilo G, Pucci G, Laurent S, Macquin-Mavier I, Boutouyrie P, Battista F, Settimi L, Desamericq G, Dolbeau G, Faini A, Salvi P, Mannarino E, Parati G (2012) Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension 60:369–377
Garland EM, Gamboa A, Okamoto L, Raj SR, Black BK, Davis TL, Biaggioni I, Robertson D (2009) Renal impairment of pure autonomic failure. Hypertension 54:1057–1061
Tha KK, Terae S, Yabe I, Miyamoto T, Soma H, Zaitsu Y, Fujima N, Kudo K, Sasaki H, Shirato H (2010) Microstructural white matter abnormalities of multiple system atrophy: in vivo topographic illustration by using diffusion-tensor MR imaging. Radiology 255:563–269
Vagaonescu TD, Saadia D, Tuhrim S, Phillips RA, Kaufmann H (2000) Hypertensive cardiovascular damage in patients with primary autonomic failure. Lancet 355:725–726
Umoto M, Miwa H, Ando R, Kajimoto Y, Kondo T (2012) White matter hyperintensities in patients with multiple system atrophy. Parkinsonism Relat Disord 18:17–20
Oh YS, Kim JS, Yang DW, Koo JS, Kim YI, Jung HO, Lee KS (2013) Nighttime blood pressure and white matter hyperintensities in patients with Parkinson disease. Chronobiol Int 30:811–817
Marti MJ, Tolosa E, Campdelacreu J (2003) Clinical overview of the synucleinopathies. Mov Disord 18(Suppl 6):S21–S27
Coon EA, Cutsforth-Gregory JK, Benarroch EE (2018) Neuropathology of autonomic dysfunction in synucleinopathies. Mov Disord 33:349–358
Palma JA, Mano T (2018) Central or peripheral autonomic dysfunction in Parkinson disease: does it matter? Neurology 90:1045–1046
Merola A, Espay AJ, Zibetti M, Romagnolo A, Rosso M, Maule S, Lopiano L (2017) Pure autonomic failure versus prodromal dysautonomia in Parkinson’s disease: insights from the bedside. Mov Disord Clin Pract 4:141–144
Kaufmann H, Norcliffe-Kaufmann L, Palma JA, Biaggioni I, Low PA, Singer W, Goldstein DS, Peltier AC, Shibao CA, Gibbons CH, Freeman R, Robertson D (2017) Natural history of pure autonomic failure: a United States prospective cohort. Ann Neurol 81:287–297
Hague K, Lento P, Morgello S, Caro S, Kaufmann H (1997) The distribution of Lewy bodies in pure autonomic failure: autopsy findings and review of the literature. Acta Neuropathol 94:192–196
Di Stefano C, Maule S (2017) Treatment of supine hypertension in autonomic failure: a case series. Clin Auton Res 28:245–246
Gibbons CH, Schmidt P, Biaggioni I, Frazier-Mills C, Freeman R, Isaacson S, Karabin B, Kuritzky L, Lew M, Low P, Mehdirad A, Raj SR, Vernino S, Kaufmann H (2017) The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol 264:1567:1582
Jordan J, Shannon JR, Pohar B, Paranjape SY, Robertson D, Robertson RM, Biaggioni I (1999) Contrasting effects of vasodilators on blood pressure and sodium balance in the hypertension of autonomic failure. J Am Soc Nephrol 10:35–42
Calne DB, Teychenne PF (1977) L-DOPA effect on blood pressure in man. Prog Brain Res 47:331–336
Noack C, Schroeder C, Heusser K, Lipp A (2014) Cardiovascular effects of levodopa in Parkinson’s disease. Parkinsonism Relat Disord 20:815–818
Fereshtehnejad SM, Zeighami Y, Dagher A, Postuma RB (2017) Clinical criteria for subtyping Parkinson’s disease: biomarkers and longitudinal progression. Brain 140:1959–1976
Iodice V, Low DA, Vichayanrat E, Mathias CJ (2011) Cardiovascular autonomic dysfunction in MSA and Parkinson’s disease: similarities and differences. J Neurol Sci 310:133–138
Norcliffe-Kaufmann L, Kaufmann H (2014) Is ambulatory blood pressure monitoring useful in patients with chronic autonomic failure? Clin Auton Res 24:189–192
Merola A, Romagnolo A, Rosso M, Lopez-Castellanos JR, Wissel BD, Larkin S, Bernardini A, Zibetti M, Maule S, Lopiano L, Espay AJ (2016) Orthostatic hypotension in Parkinson’s disease: does it matter if asymptomatic? Parkinsonism Relat Disord 33:65–71
Merola A, Romagnolo A, Rosso M, Suri R, Berndt Z, Maule S, Lopiano L, Espay AJ (2018) Autonomic dysfunction in Parkinson’s disease: a prospective cohort study. Mov Disord 33:391–397
de Lau LM, Breteler MM (2006) Epidemiology of Parkinson’s disease. Lancet Neurol 5:525–535
Bower JH, Maraganore DM, McDonnell SK, Rocca WA (1997) Incidence of progressive supranuclear palsy and multiple system atrophy in Olmsted County, Minnesota, 1976 to 1990. Neurology 49:1284–1288
Acknowledgements
Authors acknowledge the contributions of the Autonomic and Hypertension Unit staff.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Fabrizio Vallelonga reports no disclosures. Cristina Di Stefano reports no disclosures. Aristide Merola is supported by NIH (KL2 TR001426) and has received speaker honoraria from CSL Behring, Abbvie, and Cynapsus Therapeutics. He has received grant support from Lundbeck and Abbvie and personal compensation from Lundbeck, Abbvie, and Abbott. Alberto Romagnolo has received grant support and speaker honoraria from AbbVie, speaker honoraria from Chiesi Farmaceutici and travel grants from Lusofarmaco and UCB Pharma. Gabriele Sobrero reports no disclosures. Valeria Milazzo reports no disclosures. Alessio Burrello reports no disclosures. Jacopo Burrello reports no disclosures. Maurizio Zibetti has received speaker’s honoraria from Medtronic, Chiesi Farmaceutici, UCB Pharma, and AbbVie. Franco Veglio reports no disclosures. Simona Maule reports no disclosures.
Ethical standard
The authors declare that they acted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. The local institutional review board (Comitato Etico Interaziendale Città della Salute e della Scienza di Torino) approved the study and all participants provided written informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vallelonga, F., Di Stefano, C., Merola, A. et al. Blood pressure circadian rhythm alterations in alpha-synucleinopathies. J Neurol 266, 1141–1152 (2019). https://doi.org/10.1007/s00415-019-09244-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09244-w