Abstract
Objective
To better understand the demographic, neuropsychiatric, cognitive, and motor predictors of apathy in Parkinson’s disease (PD).
Method
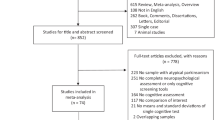
112 participants (Mage = 68.53 years; Mdisease duration = 6.17 years) were administered the Apathy Scale (AS), Beck Depression Inventory-II (BDI-II), Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), Trail Making Test (TMT), Wechsler Adult Intelligence Scale-IV Matrix Reasoning subtest, letter (F-A-S) and category (Animals) fluency, and Hopkins Verbal Learning Test-Revised. Psychosis was assessed. A stepwise logistic regression analysis was performed to investigate the ability of demographic factors and clinical assessments to predict nonapathetic (AS ≤ 13) versus apathetic (AS > 13) group membership.
Results
The regression analysis yielded a robust model in which older age, less education, elevated BDI-II, current psychosis, higher MDS-UPDRS Part III (motor score), and slower TMT-B performance predicted membership in the apathetic group, with a correct classification rate of 77.5% (Nagelkerke R2 = 0.48, p < .001). Depression (OR = 9.20, p < .001) and education (OR = 0.66, p = 0.002) contributed significantly to the overall model. A linear regression with AS score as the outcome variable was similar, but TMT-B additionally contributed significantly (p = 0.02) to the overall model, F(6, 86) = 12.02, p < .001, adjusted R2 = 0.42.
Conclusions
Of the factors examined, depression, education, and executive functioning were the strongest correlates of apathy in PD. These results support the idea that common underlying frontosubcortical disruptions in this population contribute to apathy, depression, and executive dysfunction.
Similar content being viewed by others
References
Bernal-Pacheco O, Fernandez HH (2013) Apathy in Parkinson’s disease. In: Pfeiffer RR, Bodis-Wollner I (eds) Parkinson’s disease and nonmotor dysfunction, 2nd edn. Humana Press, Totowa, pp 119–129
Thant T, Yager J (2018) Updating apathy: using research domain criteria to inform clinical assessment and diagnosis of disorders of motivation. J Nerv Ment Dis Advance on. https://doi.org/10.1097/NMD.0000000000000860
Aarsland D, Marsh L, Schrag A (2009) Neuropsychiatric symptoms in Parkinson’s disease. Mov Disord 24:2175–2186. https://doi.org/10.1002/mds.22589
Pagonabarraga J, Kulisevsky J, Strafella AP, Krack P (2015) Apathy in Parkinson’s disease: Clinical features, neural substrates, diagnosis, and treatment. Lancet Neurol 14:518–531. https://doi.org/10.1016/S1474-4422(15)00019-8
Bogart KR (2011) Is apathy a valid and meaningful symptom or syndrome in Parkinson’s disease? A critical review. Heal Psychol 30:386–400. https://doi.org/10.1037/a0022851
Leroi I, Harbishettar V, Andrews M et al (2012) Carer burden in apathy and impulse control disorders in Parkinson’s disease. Int J Geriatr Psychiatry 27:160–166. https://doi.org/10.1002/gps.2704
Starkstein SE, Brockman S (2011) Apathy and Parkinson’s disease. Curr Treat Options Neurol 13:267–273. https://doi.org/10.1007/s11940-011-0118-9
Isella V, Melzi P, Grimaldi M et al (2002) Clinical, neuropsychological, and morphometric correlates of apathy in Parkinson’s disease. Mov Disord 17:366–371. https://doi.org/10.1002/mds.10041
Leroi I, David R, Robert PH (2012) Apathy in Parkinson’s disease. In: Ebmeier KP, O’Brien JT, Taylor J-P (eds) Psychiatry of Parkinson’s disease. Karger, Basel, pp 27–40
Levy R, Dubois B (2006) Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cereb Cortex 16:916–928. https://doi.org/10.1093/cercor/bhj043
García-Ramos R, Villanueva C, del Val J, Matías-Guíu J (2010) Apathy in Parkinson’s disease. Neurología 25:40–50. https://doi.org/10.1016/S0213-4853(10)70021-9
Santangelo G, Trojano L, Barone P et al (2013) Apathy in Parkinson’s disease: Diagnosis, neuropsychological correlates, pathophysiology and treatment. Behav Neurol 27:501–513. https://doi.org/10.3233/BEN-129025
Benito-León J, Cubo E, Coronell C (2012) Impact of apathy on health-related quality of life in recently diagnosed Parkinson’s disease: the ANIMO study. Mov Disord 27:211–218. https://doi.org/10.1002/mds.23872
Cubo E, Benito-León J, Coronell C, Armesto D (2012) Clinical correlates of apathy in patients recently diagnosed with Parkinson’s disease: the ANIMO Study. Neuroepidemiology 38:48–55. https://doi.org/10.1159/000334314
Pedersen KF, Larsen JP, Alves G, Aarsland D (2009) Prevalence and clinical correlates of apathy in Parkinson’s disease: a Community-based study. Park Relat Disord 15:295–299. https://doi.org/10.1016/j.parkreldis.2008.07.006
Dujardin K, Sockeel P, Delliaux M et al (2009) Apathy may herald cognitive decline and dementia in Parkinson’s disease. Mov Disord 24:2391–2397. https://doi.org/10.1002/mds.22843
Oguru M, Tachibana H, Toda K et al (2010) Apathy and depression in Parkinson disease. J Geriatr Psychiatry Neurol 23:35–41. https://doi.org/10.1177/0891988709351834
Skorvanek M, Rosenberger J, Gdovinova Z et al (2013) Apathy in elderly nondemented patients with Parkinson’s disease: clinical determinants and relationship to quality of life. J Geriatr Psychiatry Neurol 26:237–243. https://doi.org/10.1177/0891988713500587
Dujardin K, Sockeel P, Devos D et al (2007) Characteristics of apathy in Parkinson’s disease. Mov Disord 22:778–784. https://doi.org/10.1002/mds.21316
Martínez-Horta S, Pagonabarraga J, Fernández de Bobadilla R et al (2013) Apathy in Parkinson’s disease: more than just executive dysfunction. J Int Neuropsychol Soc 19:571–582. https://doi.org/10.1017/S1355617713000131
Meyer A, Zimmermann R, Gschwandtner U et al (2015) Apathy in Parkinson’s disease is related to executive function, gender and age but not to depression. Front Aging Neurosci 6:1–6. https://doi.org/10.3389/fnagi.2014.00350
Pluck GC, Brown RG (2002) Apathy in Parkinson’s disease. J Neurol Neurosurg Psychiatry 73:636–642. https://doi.org/10.1136/jnnp.73.6.636
den Brok MGHE, van Dalen JW, van Gool WA et al (2015) Apathy in Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 30:759–769. https://doi.org/10.1002/mds.26208
Gibb WRG, Lees AJ (1988) The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 51:745–752. https://doi.org/10.1136/jnnp.51.6.745
Emre M, Aarsland D, Brown R et al (2007) Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 22:1689–1707. https://doi.org/10.1002/mds.21507
Goetz CG, Poewe W, Rascol O et al (2004) Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord 19:1020–1028. https://doi.org/10.1002/mds.20213
Tomlinson CL, Stowe R, Patel S et al (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25:2649–2653. https://doi.org/10.1002/mds.23429
Starkstein SE, Mayberg HS, Preziosi TJ et al (1992) Reliability, validity, and clinical correlates of apathy in Parkinson’s disease. J Neuropsychiatry Clin Neurosci 4:134–139. https://doi.org/10.1176/jnp.4.2.134
Marin RS, Biedrzycki RC, Firinciogullari S (1991) Reliability and validity of the Apathy Evaluation Scale. Psychiatry Res 38:143–162. https://doi.org/10.1016/0165-1781(91)90040-V
Leentjens AFG, Dujardin K, Marsh L et al (2008) Apathy and anhedonia rating scales in Parkinson’s disease: critique and recommendations. Mov Disord 23:2004–2014. https://doi.org/10.1002/mds.22229
Beck AT, Steer RA, Brown GK (1996) Manual for the beck depression inventory-II. Psychological Corporation, San Antonio
Grace J, Malloy PF (2001) Frontal systems behvaior scale: professional manual. Psychological Assessment Resources, Inc., Lutz
Ravina B, Marder K, Fernandez HH et al (2007) Diagnostic criteria for psychosis in Parkinson’s disease: Report of an NINDS, NIMH Work Group. Mov Disord 22:1061–1068. https://doi.org/10.1002/mds.21382
Goetz CG, Tilley BC, Shaftman SR et al (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov Disord 23:2129–2170. https://doi.org/10.1002/mds.22340
Nasreddine ZS, Phillips NA, Bédirian V et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
Brown DS, Bernstein IH, McClintock SM et al (2016) Use of the Montreal Cognitive Assessment and Alzheimer’s Disease-8 as cognitive screening measures in Parkinson’s disease. Int J Geriatr Psychiatry 31:264–272. https://doi.org/10.1002/gps.4320
Reitan R, Wolfson D (1985) The Halstead-Reitan Neuropsychological Test Battery. Neuropsychological Publishing Group, Tucson
Wechsler D (2008) Wechsler Adult Intelligence Scale-Fourth Edition. Pearson Education, Inc., San Antonio
Lezak MD, Howieson DB, Bigler ED, Tranel D (2012) Neuropsychological assessment, 5th edn. Oxford University Press, Inc., New York
Strauss E, Sherman EMS, Spreen O (2006) A compendium of neuropsychological tests: administration, norms, and commentary, 3rd edn. Oxford University Press, Inc., New York
Brandt J, Benedict RHB (2001) Hopkins verbal learning test-revised: professional manual. Psychological Assessment Resources, Inc., Lutz
Heaton RK, Miller SW, Taylor MJ, Grant I (2004) Revised comprehensive norms for an expanded Halstead-Reitan battery: demographically adjusted neuropsychological norms for African American and Caucasian adults. Psychological Assessment Resources, Inc., Lutz
Dalrymple-Alford JC, MacAskill MR, Nakas CT et al (2010) The MoCA: Well-suited screen for cognitive impairment in Parkinson disease. Neurology 75:1717–1725. https://doi.org/10.1212/WNL.0b013e3181fc29c9
Hoops S, Nazem S, Siderowf a D et al (2009) Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology 73:1738–1745. https://doi.org/10.1212/WNL.0b013e3181c34b47
Zgaljardic DJ, Borod JC, Foldi NS et al (2007) Relationship between self-reported apathy and executive dysfunction in nondemented patients with Parkinson disease. Cogn Behav Neurol 20:184–192. https://doi.org/10.1097/WNN.0b013e318145a6f6
Arbuthnott K, Frank J (2000) Trail Making Test, Part B as a measure of executive control: Validation using a set-switching paradigm. J Clin Exp Neuropsychol 22:518–528. https://doi.org/10.1076/1380-3395(200008)22:4;1-0;FT518
Muslimovic D, Post B, Speelman JD, Schmand B (2005) Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology 65:1239–1245. https://doi.org/10.1212/01.wnl.0000180516.69442.95
Zgaljardic DJ, Foldi NS, Borod JC (2004) Cognitive and behavioral dysfunction in Parkinson’s disease: neurochemical and clinicopathological contributions. J Neural Transm 111:1287–1301. https://doi.org/10.1007/s00702-004-0178-z
Lorant V, Deliège D, Eaton W et al (2003) Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 157:98–112. https://doi.org/10.1093/aje/kwf182
Acknowledgements
This study was funded by the American Parkinson Disease Association Center for Advanced Research at the University of Virginia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study received local institutional review board approval and has, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Written informed consent was obtained from all participants prior to their inclusion in the study.
Rights and permissions
About this article
Cite this article
Brown, D.S., Barrett, M.J., Flanigan, J.L. et al. Clinical and demographic correlates of apathy in Parkinson’s disease. J Neurol 266, 507–514 (2019). https://doi.org/10.1007/s00415-018-9166-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9166-3